Strengths and Limitations of Clinical Trials
Large randomized clinical trials can provide strong evidence of the true effect of a treatment or intervention, because they provide excellent control of confounding, but they also have some limitations:
Non-adherence
Ideally, the investigators want to compare exposed subjects to non-exposed in groups that are similar with respect to confounding factors. The true benefit of a new drug will be underestimated if subjects given the active medication fail to take it, causing subjects who were actually not exposed to be mixed in with the exposed subjects who were actually taking the medication. This mixing of the exposure groups dilutes the apparent benefit causing underestimates of association. The same thing occurs if people in the placebo group begin taking the active medication. This occurred in the Physicians' Health Study in which follow up questionnaires estimated that about 15% of the subjects assigned to the aspirin group did not take it, and a similar proportion of subjects in the placebo group used aspirin fairly regularly. This would cause an underestimate of the true benefit. In this case, in which the exposure was preventive with an observed risk ratio = 0.59, the true risk ratio would have been even smaller. In other words, non-adherence caused a "bias toward the null," an underestimate of the true benefit.
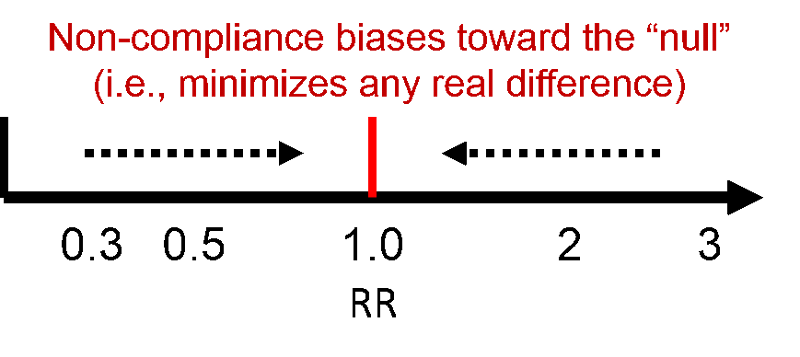
Non-compliance can occur due to side effects of the treatment, illness, or loss of interest in the study.
How to Promote Adherence in a Clinical Trial
- Begin with an interested group of participants
- Make it easy to participate
- Present a realistic picture of the protocol during informed consent
- Exclude participants with pre-existing conditions that make compliance difficult
- Simplify the protocol as much as possible
- Conduct a run-in period if necessary
- Use blinding and placebos
- Keep in touch
- Maintain frequent contact with subjects WITHOUT interfering with treatment
- Provide incentives (free check-ups, transportation, t-shirts, birthday cards)


