Physicians
How do students (younger and older) choose the careers they ultimately go into? What are the incentives? What are the rewards? Perhaps the incentives are the need to work with people, the need to contribute to the prevention and treatment of disease, or the need to change the world. For some, salary may also play a large role, especially if they are facing the possibility of $300,000 worth of debt following graduation.
In 2012 there were 13.5 million people employed in health care settings. Even with the recent recession and moderate unemployment rates across the country, the health care industry continues to add jobs. Of the 30 occupations projected to have largest percent increases in jobs between 2012 and 2022, 14 of those occupations are related to health care. Over this time the overall labor force is predicted to grow at 0.6% annually. In health care the predicted annual growth is 2.6%. This adds up to of 5 million jobs in a decade.
Becoming a Physician
The University of Pennsylvania opened the first US medical school in 1765. The curriculum included intestinal purging and blood-letting. Many practicing physicians had not attended any formal educational program and were trained by apprenticeship. In the early 1800s the field of medical education evolved to include uniform academic preparation. Today a person becomes an MD (Doctor of Medicine) or a DO (Doctor of Osteopathy) by education. The degree is only the start of the process. The license to practice medicine comes from each state, there is no national system. In most states the scope of practice is the same for MDs and DOs.
Massachusetts policy defines the practice of medicine as follows:
|
"The Practice of Medicine means the following conduct, the purpose or reasonably foreseeable effect of which is to encourage the reliance of another person upon an individual's knowledge or skill in the maintenance of human health by the prevention, alleviation, or cure of disease, and involving or reasonably thought to involve an assumption of responsibility for the other person's physical or mental well being: diagnosis, treatment, use of instruments or other devices, or the prescribing, administering, dispensing or distributing of drugs for the relief of diseases or adverse physical or mental conditions. (a) A person who holds himself or herself out to the public as a physician or surgeon, or with the initials "M.D." or "D.O." in connection with his or her name, and who also assumes responsibility for another person's physical or mental well-being, is engaged in the practice of medicine." |
Minimum requirements for an initial license in Massachusetts include the following:
|
Physicians wishing to practice in additional states must make arrangements with the individual Board of Registrations. Scope of practice regulations for any licensed medical profession are state-based. There are additional guidelines for International Medical Graduates (IMG) to allow entry to practice without repeating the complete training.
Physician Specialization
Primary care physicians (PCPs) provide preventive services and treat frequently occurring and less severe problems, while specialists must have certification in an area of medical specialization. This requires additional years of advanced residency training followed by several years of practice in that specialty.
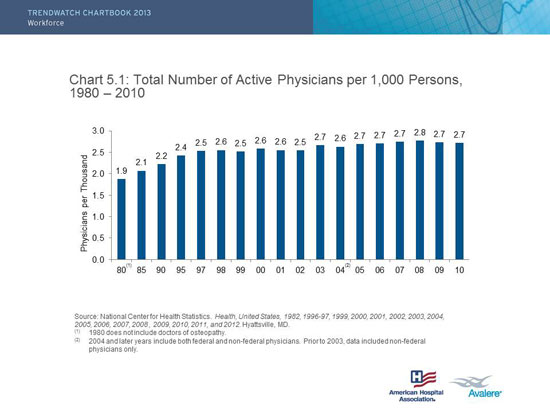
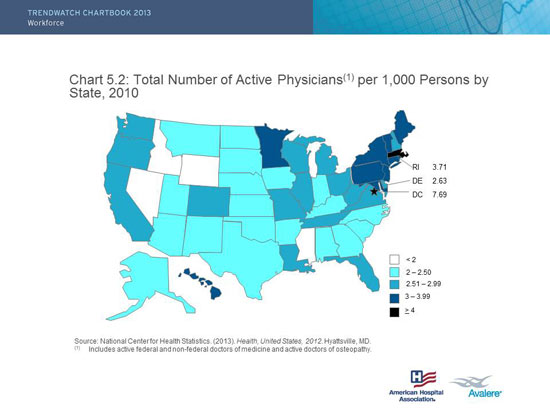
In addition to the sharp increase in the physician labor force in the US (resulting in a current oversupply), there also exists a "maldistribution" of physicians. Not only does the physician supply exceed previous projections (as well as future growth projections through the first decade of the 21st century), a surplus of physicians, among other issues we are discussing, can lead to increases in health care expenditures. This is an example of a geographic maldistribution. The number of MDs per 1000 persons is slightly increasing, or constant. The distribution across the United Stated is skewed. Note the data are adjusted for the state population.
There are two concerns. First, physician distribution across the United States is skewed (see figure). Second, it is believed that the US has far too many specialists and a shortage of primary care physicians. Specialty care is concerning because care is generally more resource incentive, tend to order more tests and procedures- resulting in higher cost. Furthermore specialists focus on their own specialty, and patient care can become fragmented without the holistic perspective of primary care to coordinate.
Explore the two statistical data graphs below from the report.
|
|
|
Source: AHA Chartbook: Trends Affecting Hospitals and Heatlh Systems
Many factors go into the decision of a physician to practice primary care including academic interest, availability of training opportunities, work-life balance, and potential income. The reality is that medical education is incredibly expensive. Specialists are paid more than primary care physician and so the ability to repay school loans is an important factor to consider.
Hospitalists
Definition of a Hospitalist and Hospital Medicine
Hospital medicine: A medical specialty dedicated to the delivery of comprehensive medical care to hospitalized patients. Practitioners of hospital medicine include physicians ("hospitalists") and non-physician providers who engage in clinical care, teaching, research, or leadership in the field of general hospital medicine. In addition to their core expertise of managing the clinical problems of acutely ill, hospitalized patients, hospital medicine practitioners work to enhance the performance of hospitals and healthcare systems by:
- Prompt and complete attention to all patient care needs including diagnosis, treatment, and the performance of medical procedures (within their scope of practice).
- Employing quality and process improvement techniques.
- Collaboration, communication, and coordination with all physicians and healthcare personnel caring for hospitalized patients.
- Safe transitioning of patient care within the hospital, and from the hospital to the community, which may include oversight of care in post-acute care facilities.
- Efficient use of hospital and healthcare resources.
Though the concept appeared a bit strange to many patients at the outset, and some patients still ask, "Where's my doctor?" hospitalists are often much more familiar with the hospital and its systems and functions. Because the hospital is the primary site of their practice, they are usually able to spend more time with patients than physicians who must juggle office patients, transportation, and often have to see their patients in between other commitments (early morning, at lunch, or at the end of a long day after office hours).
For the hospitalist model to work there must be processes in place to allow two-way communication between the hospitalist and the primary care team. Access to the patient's medical information is key. Once the patient is ready to be discharged the hospitalist must ensure there is a plan in place for a smooth transition to home and community medical services. The PCP needs access to records form the hospitalization to ensure continuity of care after discharge.