Medicaid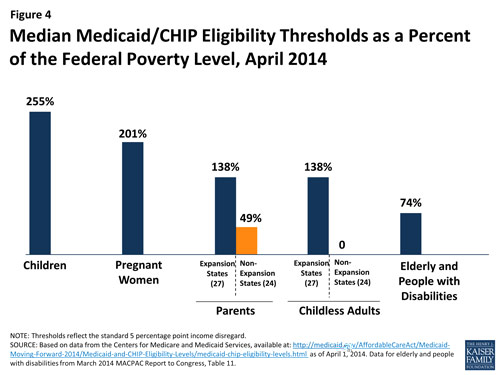
Before January 2014 state Medicaid programs were required to cover poor pregnant women and children, and the FPL cutoffs varied by group. States had the option of providing increased coverage within these groups, and to expand coverage to other people. As previously explained Medicaid expansion will cover all persons up to 133% of the FPL in states choosing to expand. If states do not expand, coverage will vary by FPL within a group. Pregnant women, children, the elderly and the disabled have minimum coverage thresholds. Many states have minimal or no coverage for adults, especially for adults without children.
Financing and Reimbursement
Medicaid is jointly funded by the US Federal Government and the individual States. The federal government pays states for a specified percentage of program expenditures (the FMAP). More information is available on the Financing and Reimbursement web page at Medicaid.gov.
Children's Health Insurance Program (CHIP)
The Children's Health Insurance Program (CHIP) provides health coverage to nearly 8 million children in families with incomes too high to qualify for Medicaid, who can't afford private coverage. Signed into law in 1997, CHIP provides federal matching funds to states to provide this coverage. See additional information on Cost Sharing.
|
If you would like more information about Medicaid, check these three sites: |
|
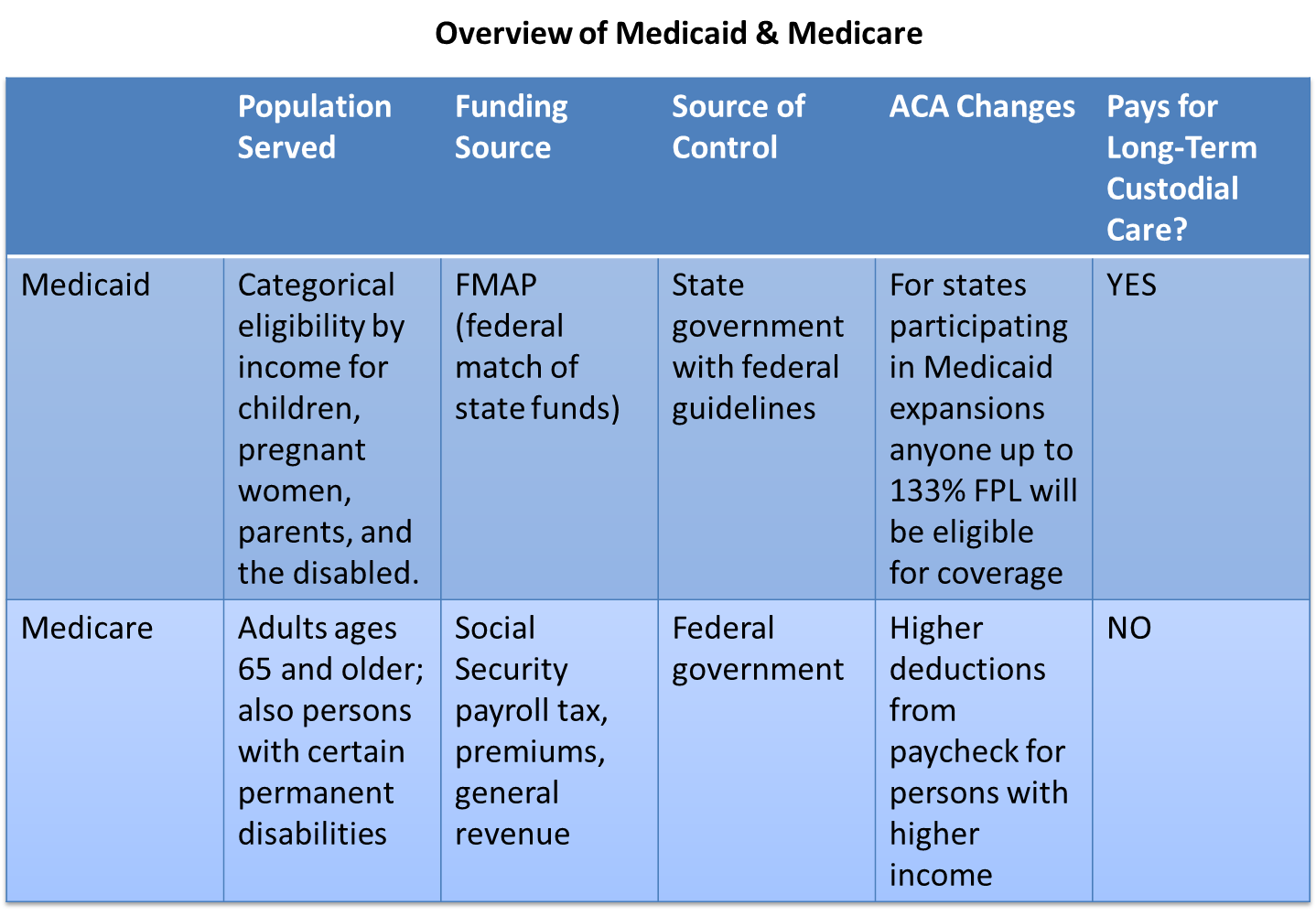
Comparison of Medicare and Medicaid |
|
|
Medicare |
Medicaid |
|
|
Dual Eligibles
Dual eligible refers to patients with both Medicare and Medicaid. The care of dual eligibles is often expensive, fragmented, and of varying quality. Innovative models of care for duals (often consider duals < 65 years separately from elderly duals) are needed to provide efficient and effective care for these vulnerable populations.
|
Dual Eligibles |
Infographic: Medicaid Spending and Enrollment: Who Is Covered and What Does the Program Spend on Their Care
Source: http://kff.org/interactive/infographic-medicaid-spending-enrollment/. The Infographic in the window above is a web page with links that you can explore on your own. You can scroll through the web page using the scroll bar on the right side of the frame.
Medicaid Information by Topic from Medicaid.gov
 |
Roll over the tabs to view more information. |
|
This content requires JavaScript enabled.
|
|
More Resources
- http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/By-Topic.html)
- http://facts.kff.org/chart.aspx?ch=464
- http://facts.kff.org/chart.aspx?ch=472
- The Commonwealth Fund site for State Health policy and Medicaid
- The Medicaid Program at a Glance (from the Kaiser Foundation)
Medicaid 101: What You Need to Know
Source: http://www.kff.org/medicaid/ahr030113.cfm