Direct Person-to Person Transmission
Sexual Transmission
Intimate sexual contact provides opportunities for transmission of several types of infectious agents:
- The infectious agent doesn't have to survive in the external environment.
- It doesn't need a large population of potential hosts to sustain transmission and survival.
- It doesn't need an animal reservoir to sustain its survival.
|
Protozoa |
Bacteria |
Viruses |
|---|---|---|
|
Chancroid (Haemophilus ducreyi) |
Viral hepatitis (B> C > [A])
|
HIV
|
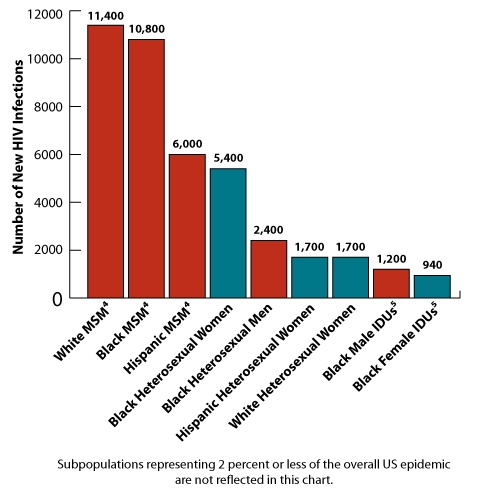
Estimates of New HIV Infections, by Race/Ethnicity, Risk Group, and Gender for the Most Affected US Populations, 2009 http://www.cdc.gov/hiv/topics/women/index.htm
|
|
Per Act Risk of HIV Transmission for Various Behaviors
These estimates are rough approximations gleaned from a number of studies. There are several factors that can modify risk, such as viral load in the infected partner. For an excellent discussion of HIV risk see Safer Sex Methods at the HIV-Insite from UCSF.
|
Exposure |
Transmission Probability (Attack Rate) |
|---|---|
|
Blood Transfusion Perinatal Penile vaginal intercourse
Penile-anal intercourse Oral sex Injecting drugs Health care (sharps injury) Mucous membrane exposure to infected blood Household Other |
>0.9 0.1-0.4 0.0005-0.0009 male-to-female 0.0003-0.0001 female-to-male 0.008 Much lower, but definitely possible <0.01 <0.003 0.0009 Rare - can occur via blood contact Virtually non-existent |
Kissing
Disease can be transmitted through kissing. A wide variety of viruses that cause upper respiratory tract infections (influenza, sore throat, cold, laryngitis, tracheitis, etc.) can be transmitted through kissing. In addition, the human papilloma virus can be transmitted through kissing, particularly oral sex, and this can contribute to the risk of oral cancers. Other diseases that can be transmitted through kissing include mononucleosis (a virus) and Streptococcus (a bacterium).
Perinatal Mother-to-Child Transmission (PMTCT; Vertical Transmission)
There are several diseases that can be transmitted from mother to child in the perinatal period. Cytomegalovirus is the most common, but HIV is also transmitted vertically with an incidence of around 25% with preventive measures.
These diseases include:
|
HIV Chagas Disease Gonorrhea Chlamydia |
Varicella-zoster virus (chicken pox) West Nile virus Eastern equine encephalitis Yellow fever |
PMTCT of HIV
Mother to child transmission of HIV can occur before, during, or after delivery (15-40%). Transmission is rare during early pregnancy, but relatively frequent in late pregnancy & during delivery.
Breastfeeding increases risk by approximately 15%. The wide range in risk estimates are due to the influence of other factors that increase the risk of vertical transmission:
- Maternal progression of infection (increased viral load).
- Premature infants are more likely to be infected.
- Long duration of membrane rupture.
|
From: Paintsil E and Andiman WA: Update on successes and challenges regarding mother-to-child transmission of HIV. Curr Opin Pediatr. 2009 February ; 21(1): 94–101.
Basic principles of mother-to-child transmission of HIV "Without any intervention to prevent transmission, the rate of MTCT of HIV is estimated at 12-40% (3). MTCT of HIV can occur before, during, and after birth. The relative contribution of each of these modes of perinatal transmission is not well defined (4). The risk factors associated with MTCT are illustrated in Table 1. In resource-limited countries, breast feeding contributes significantly to MTCT."
Prevention of mother-to-child transmission "Current interventions to prevent MTCT target the late intrauterine and intrapartum periods, when most transmission events occurs. Administration of antiretroviral drugs to an HIV infected mother and her infant, careful management of labor and delivery (with elective caesarean delivery for women with high HIV viral loads) and avoidance of breast feeding have reduced the rate of MTCT to less than 2%."
Summary "While the birth of an HIV-infected child in a resource-rich country is now a sentinel health event, in most resource-limited countries the birth of an HIV-infected child continues to be the status quo. Comprehensive PMTCT including ARV treatment for HIV-infected women and HIV-infected children should be paramount in resource-limited countries." |
Needle Injection & Occupational Sharps Exposure
There are many organisms that can be transmitted to health care workers in a clinical setting. In this section focuses primarily on occupational "sharps" injuries (direct contact) to infectious agents, including HIV, hepatitis B, and hepatitis C, although other pathogens might also be transmitted by this route. We could also include contaminated blood products and shared needles among intravenous drug users, since these also involve exposure via breaching of the skin barrier barrier. However, one might also consider these to be common vehicle modes of transmission.
Occupational injuries that result in exposure to HIV, hepatitis B & C and other agents are common. It is estimated that there are 380,000 needle stick injuries per year in hospitals, and many more in non-hospital settings. As of 2001, CDC had reports of 57 documented cases & 138 probable cases of seroconversion after occupational exposures in health care. While these injuries warrant great concern, the absolute risk of clinical infection is low. For example, it is estimated that the risk of seroconversion after exposure to HIV-infected blood from a needle stick injury in about 0.003 or 0.3%. The risk of seroconversion after mucous membrane exposure to infected blood is estimate at 0,09%, and the risk of conversion after exposure of non-intact skin to contaminated body fluid is too low to estimate. Nevertheless, these exposures are all preventable and can have dire consequences, and appropriate precautions should always be taken. For more information see the CDC information regarding healthcare-associated injuries.
The primary precautions include:
- routinely using barriers (such as gloves and/ or goggles) when anticipating contact with blood or body fluids,
- immediately washing hands and other skin surfaces after contact with blood or body fluids, and
- carefully handling and disposing of sharp instruments during and after use.
When occupational exposures occur, post-exposure prophylactic treatment should be strongly considered.
The best practice is to exercise "universal precautions" for all patients.
|
Universal Precautions |
|---|
|
Prevention of HIV
Cautious partner selection and practice of safer sex are important steps towards prevention of HIV transmission. In addition, the following comments and measures are relevant.
- CDC Recommendations for prevention of PMTCT of HIV
- Condoms: Male latex condoms & male and female polyurethane condoms provide a reliable barrier to transmission of HIV, hepatitis B virus (HBV), and other sexually transmitted agents. In contrast, natural membrane condoms do not provide consistent protection.
- Spermacides: There are conflicting reports regarding the effects of spermacides, such as Nonoxynol-9 (N-9), but these are no longer recommended as a barrier to HIV.
- Post-exposure prophylaxis (PEP) with antiretroviral drugs reduces the risk of HIV infection in health care workers after exposure from needle sticks or other contact with infected blood. Other studies have suggested that PEP may be effective in reducing the risk of HIV infection after sexual exposures, including sexual assault. The current recommendation is that treatment be initiated within 72 hours of exposure and continued for 28 days.
- Pre-exposure prophylaxis: There are settings in which barrier precautions will not be reliably employed, for Several studies have tested the effectiveness of antiretroviral medications given prior to sexual exposure (pre-exposure prophylaxis, PrEP) to reduce the risk of HIV infection. Results have been inconsistent, but a large randomized clinical trial among HIV- discordant heterosexual couples was recently reported by the Partners PrEP Study Team (Antiretroviral Prophylaxis for HIV Prevention in Heterosexual Men and Women: N Engl J Med 2012; 367:399-410) and demonstrated significant reductions in the incidence of HIV infection.
US National HIV/AIDS Strategy
The major recommendations are outlined here. The full report can be obtained from http://www.whitehouse.gov/administration/eop/onap/nhas.
Reducing New HIV Infections
- Step 1: Intensify HIV prevention efforts in the communities where HIV is most heavily concentrated
- Step 2: Expand targeted efforts to prevent HIV infection using a combination of effective, evidence-based approaches\
- Step 3: Educate all Americans about the threat of HIV and how to prevent it.
Increasing Access to Care and Improving Health Outcomes for People Living with HIV
- Step 1: Establish a seamless system to immediately link people to continuous and coordinated quality care when they learn they are infected with HIV
- Step 2: Take deliberate steps to increase the number and diversity of available providers of clinical care and related services for people living with HIV.
- Step 3: Support people living with HIV with co-occurring health conditions and those who have challenges meeting their basic needs, such as housing.
Reducing HIV-Related Disparities and Health Inequities
- Step 1: Reduce HIV-related mortality in communities at high risk for HIV infection.
- Step 2: Adopt community-level approaches to reduce HIV infection in high-risk communities.
- Step 3: Reduce stigma and discrimination against people living with HIV.
Achieving a More Coordinated National Response to the HIV Epidemic
- Step 1: Increase the coordination of HIV programs across the Federal government and between federal agencies and state, territorial, tribal, and local governments.
- Step 2: Develop improved mechanisms to monitor and report on progress toward achieving national goals.
Skin to Skin Transmission
Some disease agents can be spread by direct skin to skin contact, such Tinea capitis, the fungus that causes ringworm, Tinea pedis, the fungus that causes athlete's foot, and impetigo . However, these disease are probably more often spread via fomites
. However, these disease are probably more often spread via fomites .
.
Human Bites
Bites from humans also represent a direct method of disease transmission from human to human. Human bites frequently become infected (10-15%), because of large numbers of bacteria in saliva. Diseases acquired as a result of animal bites would be considered to represent zoonotic transmission.
 How is Ebola transmitted?
How is Ebola transmitted?