Transmission of Infectious Disease
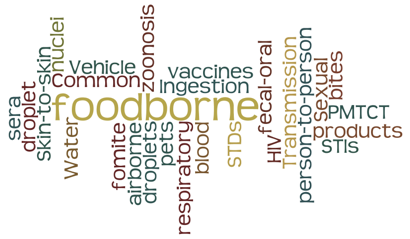
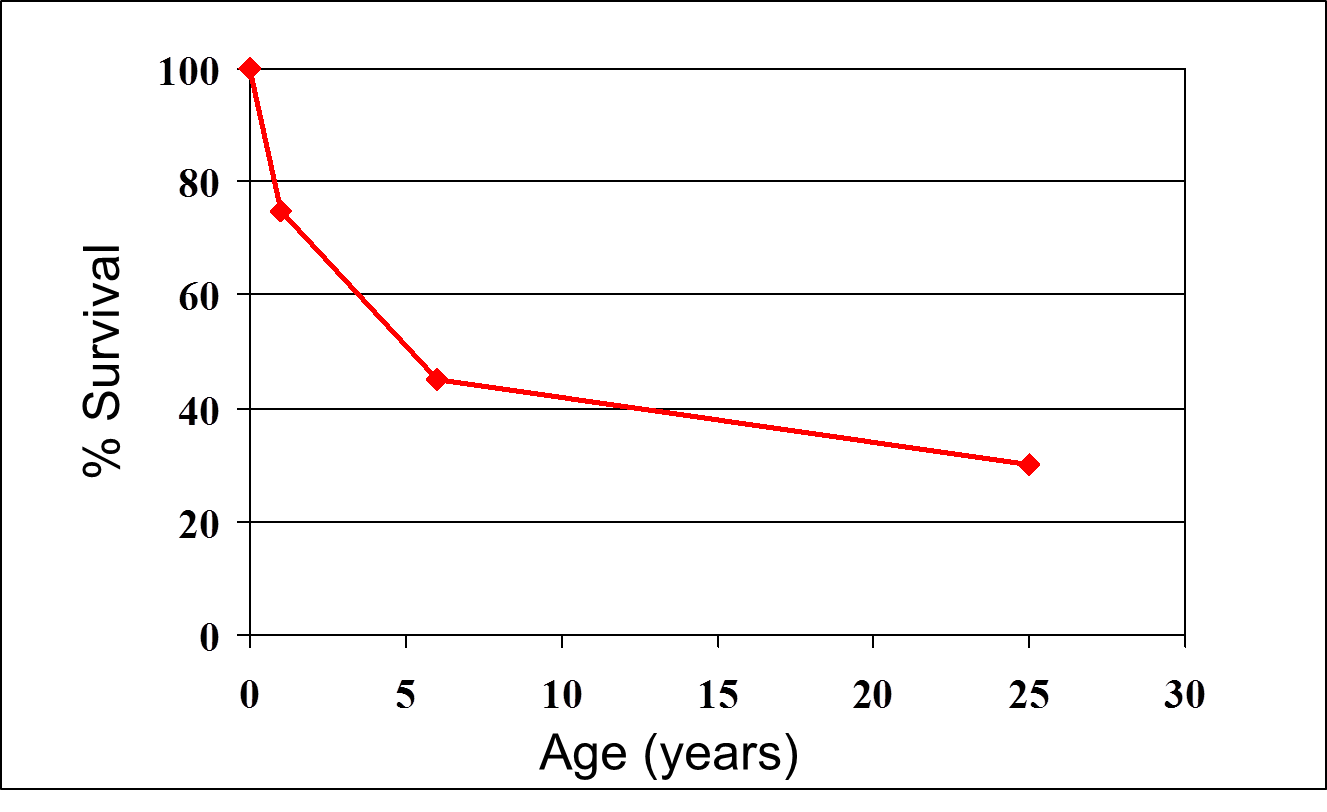 A century ago infectious diseases were by far the leading cause of death throughout the world. The graph on the right shows estimated survival among people born in the United Kingdom in the mid 1800s. Approximately 70% died before the age of 25, and the vast majority of deaths occurred among infants and children as a result of infectious disease. The emergence of "The Sanitary Idea" and the evolution of public health in the United Kingdom in the mid-1800s, the risk of infectious disease declined progressively. At present atherosclerotic heart disease and cerebrovascular disease (stroke) remain the leading causes of death worldwide, but as the table below shows, infectious diseases still remain important causes of death. Perhaps more importantly, infectious diseases remain the #1 cause of premature death throughout the world because of a particularly heavy toll in infants and children. It is estimated that 17 million people die prematurely each year, and 9 million of these are children. It is further estimated that this translates into approximately 50,000 preventable deaths per day.
A century ago infectious diseases were by far the leading cause of death throughout the world. The graph on the right shows estimated survival among people born in the United Kingdom in the mid 1800s. Approximately 70% died before the age of 25, and the vast majority of deaths occurred among infants and children as a result of infectious disease. The emergence of "The Sanitary Idea" and the evolution of public health in the United Kingdom in the mid-1800s, the risk of infectious disease declined progressively. At present atherosclerotic heart disease and cerebrovascular disease (stroke) remain the leading causes of death worldwide, but as the table below shows, infectious diseases still remain important causes of death. Perhaps more importantly, infectious diseases remain the #1 cause of premature death throughout the world because of a particularly heavy toll in infants and children. It is estimated that 17 million people die prematurely each year, and 9 million of these are children. It is further estimated that this translates into approximately 50,000 preventable deaths per day.
Public health measures have accounted for the vast majority of reductions in deaths from infectious disease through better sanitation, cleaner water, and the development of vaccines. A key to this success has been an increasingly refined understanding of the mechanisms by which infectious agents are transmitted. An understanding of mechanisms of transmission provides opportunities for simple, effective measures that will prevent disease. Moreover, an understanding of mechanisms of disease transmission is likely to provide the greatest opportunities for further reductions in premature deaths, particularly in the developing world.
After successfully completing this section, the student will be able to:
|
|
|
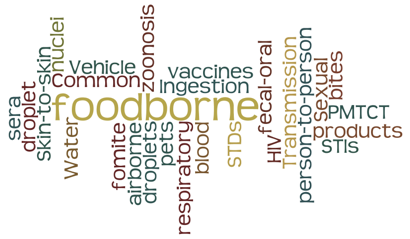
There are a number of schemes for classifying disease transmission. The various classification schemes are similar, but have slight differences, because some disease may be transmitted by more than one mechanism. For this module the outline in the table below will be followed.
|
Person-to-person Spread 1. Direct person-to-person
2. Indirect person-to-person
Common Vehicle Spread 1. Ingested: food-borne & water-borne; fecal-oral 2. Biological products: vaccines, sera, blood products
Zoonoses: from vertebrate animals 1. Animal bites (e.g., rabies virus or hepatitis from primates) 2. Blood-borne, airborne
Vector Borne: mosquitoes, flies, fleas, ticks |
![]() Two key concepts to bear in mind:
Two key concepts to bear in mind:
Intimate sexual contact provides opportunities for transmission of several types of infectious agents:
|
Protozoa |
Bacteria |
Viruses |
|---|---|---|
|
Trichomonas vaginalis |
Syphilis Gonorrhea Chlamydia Bacterial vaginosis Chancroid (Haemophilus ducreyi) Lymphogranuloma venereum |
HIV/AIDS Human papilloma virus (HPV) Genital herpes Viral hepatitis (B> C > [A])
|
|
Estimates of New HIV Infections, by Race/Ethnicity, Risk Group, and Gender for the Most Affected US Populations, 2009 http://www.cdc.gov/hiv/topics/women/index.htm
|
|
Per Act Risk of HIV Transmission for Various Behaviors
These estimates are rough approximations gleaned from a number of studies. There are several factors that can modify risk, such as viral load in the infected partner. For an excellent discussion of HIV risk see Safer Sex Methods at the HIV-Insite from UCSF.
|
Exposure |
Transmission Probability (Attack Rate) |
|---|---|
|
Blood Transfusion Perinatal Penile vaginal intercourse
Penile-anal intercourse Oral sex Injecting drugs Health care (sharps injury) Mucous membrane exposure to infected blood Household Other |
>0.9 0.1-0.4 0.0005-0.0009 male-to-female 0.0003-0.0001 female-to-male 0.008 Much lower, but definitely possible <0.01 <0.003 0.0009 Rare - can occur via blood contact Virtually non-existent |

Disease can be transmitted through kissing. A wide variety of viruses that cause upper respiratory tract infections (influenza, sore throat, cold, laryngitis, tracheitis, etc.) can be transmitted through kissing. In addition, the human papilloma virus can be transmitted through kissing, particularly oral sex, and this can contribute to the risk of oral cancers. Other diseases that can be transmitted through kissing include mononucleosis (a virus) and Streptococcus (a bacterium).
There are several diseases that can be transmitted from mother to child in the perinatal period. Cytomegalovirus is the most common, but HIV is also transmitted vertically with an incidence of around 25% with preventive measures.
These diseases include:
|
Cytomegalovirus HIV Toxoplasmosis Chagas Disease (Trypanosoma cruzi) Rubella virus Syphilis Gonorrhea Chlamydia |
Hepatitis B Coxsackie virus Epstein-Barr virus, Varicella-zoster virus (chicken pox) Human parvovirus) West Nile virus Eastern equine encephalitis Yellow fever |
Mother to child transmission of HIV can occur before, during, or after delivery (15-40%). Transmission is rare during early pregnancy, but relatively frequent in late pregnancy & during delivery.
Breastfeeding increases risk by approximately 15%. The wide range in risk estimates are due to the influence of other factors that increase the risk of vertical transmission:
|
From: Paintsil E and Andiman WA: Update on successes and challenges regarding mother-to-child transmission of HIV. Curr Opin Pediatr. 2009 February ; 21(1): 94–101.
Basic principles of mother-to-child transmission of HIV "Without any intervention to prevent transmission, the rate of MTCT of HIV is estimated at 12-40% (3). MTCT of HIV can occur before, during, and after birth. The relative contribution of each of these modes of perinatal transmission is not well defined (4). The risk factors associated with MTCT are illustrated in Table 1. In resource-limited countries, breast feeding contributes significantly to MTCT."
Prevention of mother-to-child transmission "Current interventions to prevent MTCT target the late intrauterine and intrapartum periods, when most transmission events occurs. Administration of antiretroviral drugs to an HIV infected mother and her infant, careful management of labor and delivery (with elective caesarean delivery for women with high HIV viral loads) and avoidance of breast feeding have reduced the rate of MTCT to less than 2%."
Summary "While the birth of an HIV-infected child in a resource-rich country is now a sentinel health event, in most resource-limited countries the birth of an HIV-infected child continues to be the status quo. Comprehensive PMTCT including ARV treatment for HIV-infected women and HIV-infected children should be paramount in resource-limited countries." |
There are many organisms that can be transmitted to health care workers in a clinical setting. In this section focuses primarily on occupational "sharps" injuries (direct contact) to infectious agents, including HIV, hepatitis B, and hepatitis C, although other pathogens might also be transmitted by this route. We could also include contaminated blood products and shared needles among intravenous drug users, since these also involve exposure via breaching of the skin barrier barrier. However, one might also consider these to be common vehicle modes of transmission.
Occupational injuries that result in exposure to HIV, hepatitis B & C and other agents are common. It is estimated that there are 380,000 needle stick injuries per year in hospitals, and many more in non-hospital settings. As of 2001, CDC had reports of 57 documented cases & 138 probable cases of seroconversion after occupational exposures in health care. While these injuries warrant great concern, the absolute risk of clinical infection is low. For example, it is estimated that the risk of seroconversion after exposure to HIV-infected blood from a needle stick injury in about 0.003 or 0.3%. The risk of seroconversion after mucous membrane exposure to infected blood is estimate at 0,09%, and the risk of conversion after exposure of non-intact skin to contaminated body fluid is too low to estimate. Nevertheless, these exposures are all preventable and can have dire consequences, and appropriate precautions should always be taken. For more information see the CDC information regarding healthcare-associated injuries.
The primary precautions include:
When occupational exposures occur, post-exposure prophylactic treatment should be strongly considered.
The best practice is to exercise "universal precautions" for all patients.
|
Universal Precautions |
|---|
|
Cautious partner selection and practice of safer sex are important steps towards prevention of HIV transmission. In addition, the following comments and measures are relevant.
The major recommendations are outlined here. The full report can be obtained from http://www.whitehouse.gov/administration/eop/onap/nhas.
Reducing New HIV Infections
Increasing Access to Care and Improving Health Outcomes for People Living with HIV
Reducing HIV-Related Disparities and Health Inequities
Achieving a More Coordinated National Response to the HIV Epidemic
Some disease agents can be spread by direct skin to skin contact, such Tinea capitis, the fungus that causes ringworm, Tinea pedis, the fungus that causes athlete's foot, and impetigo. However, these disease are probably more often spread via fomites.
Bites from humans also represent a direct method of disease transmission from human to human. Human bites frequently become infected (10-15%), because of large numbers of bacteria in saliva. Diseases acquired as a result of animal bites would be considered to represent zoonotic transmission.
 How is Ebola transmitted?
How is Ebola transmitted?
Fomites are inanimate objects that can become contaminated with infectious agents and serve as a mechanism for transfer between hosts. The classic example of a fomite is a park water fountain from which many people drink. Infectious agents deposited by one person can potentially be transmitted to a subsequent drinker. However, many objects that we come into contact with can serve as fomites: doorknobs, elevator buttons, hand rails, phones, writing implements, keyboards, toys in a day care center, etc. Even a stethoscope can serve as a fomite if it isn't cleansed. A 2009 study reported MRSA (methicillin-resistant Staphylococcus aureus) contamination on 15% of stethoscopes tested. Even clothing from healthcare personnel can be contaminated. Needless to say, hand washing, respiratory hygiene and period cleansing of potential fomites would substantially reduce diarrheal diseases, respiratory diseases, and soft tissue infections (e.g., impetigo and MRSA-related skin and soft tissue infections.
For detailed information on fomites, see Boone SA et al: Significance of Fomites in the Spread of Respiratory and Enteric Viral Disease. Appl Environ Microbiol. 2007 March; 73(6):1687-1696.
|
Many diseases can be spread via respiratory droplets that are propelled into the air by sneezing and coughing. The aerosols generated by coughing and sneezing contain droplets of moisture of varying size that are contaminated with infectious agents. Droplets can be propelled up to 6-12 feet depending on the size of the droplets and the force of expulsion. The largest droplets are more likely to fall to the floor or ground fairly rapidly. Medium sized droplets are more likely to enter the nasopharynx of someone nearby, and can adhere to nasopharyngeal epithelial cells where they can cause infection. Moisture in the smallest particles tends to evaporate rapidly, resulting in the formation of so-called droplet nuclei, which are very light and can remain airborne for some time. Droplet nuclei can travel from room to room or through ventilation ducts; they can also travel around the edges of standard paper masks that are typically used during surgery or other medical procedures. Because of their small size and light weight, their movement is dictated by air currents, and, if inhaled, they can flow with inhaled air far down the respiratory tract, possibly reaching the alveoli. As a result, inhaling large or medium sized droplets tends to cause upper respiratory tract infections, while inhaling the smallest particles (droplet nuclei) can cause pneumonia. Diseases that are typically spread by inhalation of medium sized droplets include bacteria (e.g., Neisseria meningitidis [a cause of bacterial meningitis] and Streptococcus) and viruses (e.g., many viruses causing the common cold, laryngitis, tracheitis and also influenza viruses). In contrast, tuberculosis (caused by the bacterium Mycobacterium tuberculosis is spread by droplet nuclei. Respiratory droplets can also contaminate inanimate objects (fomites) via coughing or sneezing or by transform from hands contaminated with a sneeze or cough. A susceptible individual can therefore acquire disease by inhalation of airborne particles. Alternatively, one can become infected by touching a person or inanimate object that is contaminated and then rubbing one's eyes or allowing the infectious particles to enter the nose or mouth. Needless to say, hand washing and respiratory hygiene provide a simple way of limiting this mode of spread. For a detailed summary of this topic, see: For an interesting perspective on respiratory transmission of infectious diseases see Musher, DM: How contagious are common respiratory infections? N Engl J Med 2003;348:1256-66. |
|
CDC Guidelines for Preventing the Transmission of Mycobacterium tuberculosis in Health-Care Facilities, 1994 |
|---|
|
(The entire document can be found at the following link.)
"M. tuberculosis is carried in airborne particles, or droplet nuclei, that can be generated when persons who have pulmonary or laryngeal TB sneeze, cough, speak, or sing (6). The particles are an estimated 1-5 um in size, and normal air currents can keep them airborne for prolonged time periods and spread them throughout a room or building (7). Infection occurs when a susceptible person inhales droplet nuclei containing M. tuberculosis, and these droplet nuclei traverse the mouth or nasal passages, upper respiratory tract, and bronchi to reach the alveoli of the lungs. Once in the alveoli, the organisms are taken up by alveolar macrophages and spread throughout the body. Usually within 2-10 weeks after initial infection with M. tuberculosis, the immune response limits further multiplication and spread of the tubercle bacilli; however, some of the bacilli remain dormant and viable for many years. This condition is referred to as latent TB infection. Persons with latent TB infection usually have positive purified protein derivative (PPD)-tuberculin skin-test results, but they do not have symptoms of active TB, and they are not infectious. In general, persons who become infected with M. tuberculosis have approximately a 10% risk for developing active TB during their lifetimes. This risk is greatest during the first 2 years after infection. Immunocompromised persons have a greater risk for the progression of latent TB infection to active TB disease; HIV infection is the strongest known risk factor for this progression. Persons with latent TB infection who become coinfected with HIV have approximately an 8%-10% risk per year for developing active TB (8). HIV-infected persons who are already severely immunosuppressed and who become newly infected with M. tuberculosis have an even greater risk for developing active TB (9-12). The probability that a person who is exposed to M. tuberculosis will become infected depends primarily on the concentration of infectious droplet nuclei in the air and the duration of exposure. Characteristics of the TB patient that enhance transmission include a) disease in the lungs, airways, or larynx; b) presence of cough or other forceful expiratory measures; c) presence of acid-fast bacilli (AFB) in the sputum; d) failure of the patient to cover the mouth and nose when coughing or sneezing; e) presence of cavitation on chest radiograph; f) inappropriate or short duration of chemotherapy; and g) administration of procedures that can induce coughing or cause aerosolization of M. tuberculosis (e.g., sputum induction). Environmental factors that enhance the likelihood of transmission include a) exposure in relatively small, enclosed spaces; b) inadequate local or general ventilation that results in insufficient dilution and/or removal of infectious droplet nuclei; and c) recirculation of air containing infectious droplet nuclei. Characteristics of the persons exposed to M. tuberculosis that may affect the risk for becoming infected are not as well defined. In general, persons who have been infected previously with M. tuberculosis may be less susceptible to subsequent infection. However, reinfection can occur among previously infected persons, especially if they are severely immunocompromised. Vaccination with Bacille of Calmette and Guerin (BCG) probably does not affect the risk for infection; rather, it decreases the risk for progressing from latent TB infection to active TB (13). Finally, although it is well established that HIV infection increases the likelihood of progressing from latent TB infection to active TB, it is unknown whether HIV infection increases the risk for becoming infected if exposed to M. tuberculosis." |
Unfortunately, the the term "common vehicle spread" is defined in several very different ways by different authors. We will use the expression to refer to transmission of disease via
These "common vehicles" potentially expose many people and can be responsible for widespread transmission. Some authors include airborne transmission in this category.
The World Health Organization takes a broad view of the potential for water-related illnesses.
|
Water-related Diseases (from WHO) |
|---|
|
"Water, sanitation and hygiene have important impacts on both health and disease. Water-related diseases include:
Water also contributes to health, for example through hygiene." |
Water is essential to life, but it is also a potential "common vehicle" for disease. Naturally occurring water has impurities, but as human populations grew and began to establish towns and cities, increasingly contaminated water became a major source of illness and premature death. All public drinking water sources in the United States are regulated by the FDA to ensure quality, although there are cases of contamination occasionally. In many parts of the world, clean water is by no means assured.
The five major classes of disease-causing agents that can be found in water are:
The first three groups of agents often enter water supplies as a result of contamination with human or animal feces. Chemical contaminants are most commonly from man-made pollution, but it can also be naturally-occurring, e.g., arsenic.
Fecal-oral transmission can occur when bacteria or viruses in the stool of one person are swallowed by another. This can occur whenever there is
Note:
The fecal-oral route can transmit diseases caused by bacteria, viruses, or protozoa.
Drugs, transfusions of blood or blood products (e.g., clotting factors for hemophiliacs), and medical devices are all considered "common vehicles," and contamination of these medical products can cause small or large disease outbreaks. In September 2012, the Centers for Disease Control and Prevention (CDC), in collaboration with state and local health departments and the Food and Drug Administration (FDA) , began investigating a multistate outbreak of fungal meningitis and other infections among patients who received contaminated methylprednisolone (an anti-inflammatory steroid) injections. The investigation began when Vanderbilt University contacted the Tennessee Department of Health to report a patient with fungal meningitis after receiving an injection of methylprednisolone. The methlyprednisolone had been prepared at the New England Compounding Center, and three lots of the drug were believed to have been contaminated. The contaminated drugs had been shipped to 75 medical facilities in 23 states, and doses had been administered to approximately 14,000 patients. The contaminated lots were recalled, and hospitals were notified, but as of March 10, 2013, 48 people had died, and 720 were being treated for persistent fungal infections.
The CDC and WHO define zoonosis (or zoonotic disease) as any disease or infection that is naturally transmissible from vertebrate animals to humans. Zoonoses can be caused by bacteria, parasites, fungi, or viruses.
|
From CDC: How do you get zoonotic diseases? |
|---|
|
"People can get zoonotic diseases from contact with infected live poultry, rodents, reptiles, amphibians, insects, and other domestic and wild animals. A common way for these diseases to spread is through the bite of a mosquito or tick. People can get diseases in most places where they might have contact with infected animals and insects, including:
Source: http://www.cdc.gov/24-7/cdcfastfacts/zoonotic.html |
Consider the following examples.
Rabies is a classic example of a zoonotic disease; an infected vertebrate (e.g., dog, bat, skunk, etc.) transmits the rabies virus to a human directly via a bite. In this case, the infected human does not transmit the disease to other humans (or animals). However, zoonotic transmission is not always limited to infection of a single human via a bite, because in many cases the disease is then transmitted from human to human
Rabies transmission to humans via an animal bite is a direct route, but zoonoses can also be transmitted from vertebrate animals to humans via vectors. Examples:
Lyme disease and West Nile disease are not transmitted from human to human, but the pneumonic form of bubonic plague (plague infection in the lungs) can be transmitted from human to human via respiratory secretions.
We usually think of Salmonella infections being acquired from eating undercooked eggs or poultry that are contaminated. However, many species of Salmonella are commonly found in the environment, they can be found in the gastrointestinal tract of many animal species, including:
Ebola would also be considered a zoonotic disease. It is believed that certain species of fruit bats in Africa are the natural reservoirs for the Ebola virus. Close contact with the secretions, organs, or body fluids of living or dead bats can infect other animals, including sub-human primates, antelopes, shrews, porcupines, agouti, and other rodents, many of which are consumed as "bush meat" in Africa. Consequently, there are several possible routes by which Ebola can be transmitted from various vertebrate animals to man. In addition, once a human is infected, the virus can be transmitted from human to human via direct contact with blood, body fluids, or organs.
Ebola
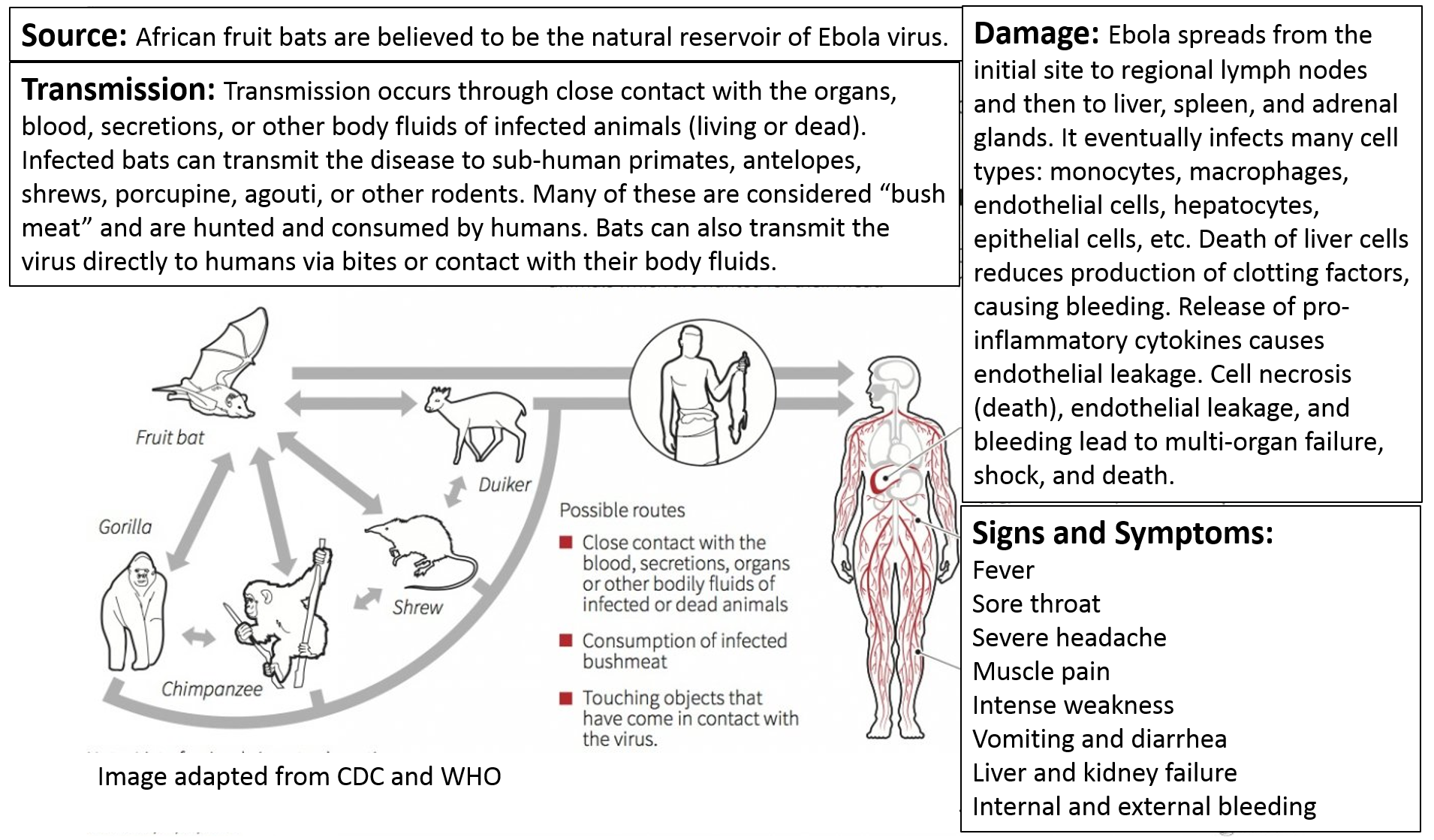
Recommended precautions for preventing Ebola transmission from infected patients.
SARS is also considered a zoonotic disease. It is believed to have originated in Chinese horseshoe bats. The virus was then transmitted to civets, small cat-like mammals that are sometimes trapped and eaten in some parts of China. Humans may have first acquired SARS from civets through exposure to their blood or organs during butchering or food preparation. However, at some point the SARS virus became capable of being transmitted from human to human via respiratory secretions.
The influenza epidemics that affect us each year can also be considered zoonotic, since they originate in wild birds and are then transmitted to domestic fowl. The virus can then jump from domestic fowl to humans, or it can be transmitted from fowl to pigs, where genetic reassortment can take place before transmission to humans. Like SARS, once the virus has jumped to humans, it can be rapidly spread via respiratory secretions.
Variant Creutzfeldt-Jakob Disease (vCJD) is acquired by humans by eating beef or beef products contaminated with the abnormal prion proteins that cause bovine spongiform encephalopathy (BSE) in cattle. As a result, vCJD meets the criterion for a zoonotic disease.
Note, however, that vCJD can also be transmitted to humans via contaminated surgical instruments or during corneal transplantation; these routes of acquisition would be better classified as "common vehicle transmission."
According to the CDC, "About 75% of recently emerging infectious diseases affecting humans are diseases of animal origin, and approximately 60% of all human pathogens are zoonotic."
As a result, many of the diseases that we now think of as distinctly human diseases, such as measles, smallpox, and diphtheria are believed to have originally jumped from animals to man.
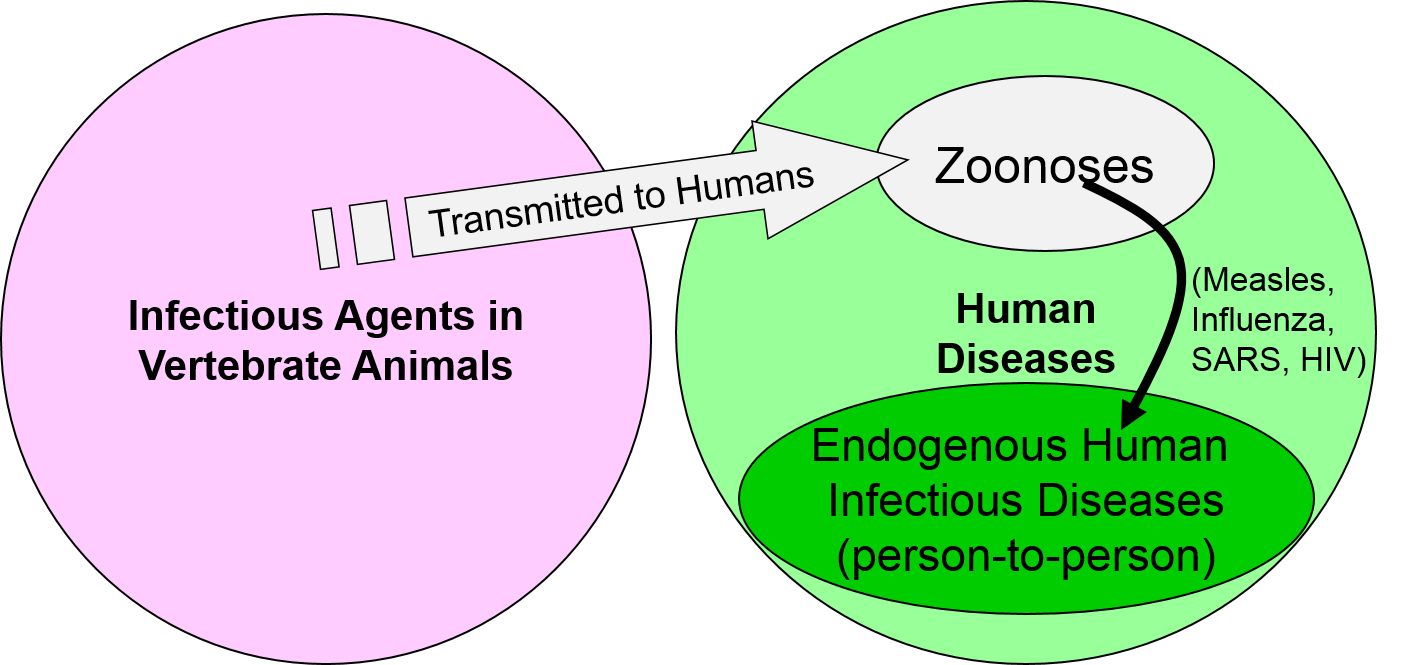
We think of measles and smallpox as distinctly human diseases, particularly since there are no known animal reservoirs for either of them. However, it is believed that measles was originally a viral disease of dogs that was similar to the distemper virus that can afflict dogs and cats today. After jumping from dogs to humans, the virus mutated over many generations, and the mutations resulted in more efficient human to human transmission via respiratory secretions and also reduced severity of illness in humans. Today's version of the measles virus has changed sufficiently that it no longer infects dogs (although dogs still are at risk of distemper). Similarly, it is believed that smallpox was originally a cowpox virus that us jumped to humans and then mutated to a form that was distinct from cowpox.
Would malaria be considered to be a zoonotic disease?
Think before you check the answer.
Answer
A vector is an organism that can transmit infectious agents from one infected person or animal to another. Vectorborne diseases are responsible for an enormous amount of morbidity and mortality across the globe, although the heaviest burden falls on countries in tropical and subtropical areas. Weather (both temperature and rainfall) has an enormous effect on the prevalence of disease and on its range and geographical distribution. Scientists are concerned that climate change will extend the range of vector-borne diseases and increase the severity of seasonal epidemics.
A partial list of diseases that can be spread by vectors is shown below.
According to WHO, "Vector-borne diseases account for 17% of the estimated global burden of all infectious diseases. The most deadly vector-borne disease, malaria, caused an estimated 627 000 deaths in 2012. However, the world's fastest growing vector-borne disease is dengue, with a 30-fold increase in disease incidence over the last 50 years."