Risk Factors for Atherosclerosis
Serum Cholesterol: LDL and HDL
It is now well-established that the risk of cardiovascular disease and mortality from coronary artery disease is directly correlated with the concentration of cholesterol in blood. The figure below summarizes this relationship in a large group of men from the MRFIT study.
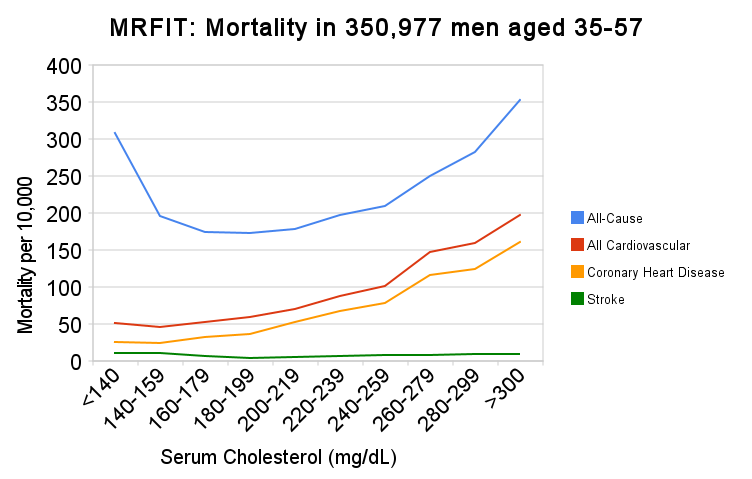
Source: Iso H, et al. N Engl J Med. 1989 Apr 6;320(14):904-10.
|
After an exhaustive review of the available evidence, the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) concluded the following: "Research from experimental animals, laboratory investigations, epidemiology, and genetic forms of hypercholesterolemia indicate that elevated LDL cholesterol
|
The NCEP panel published the risk classifications based on blood cholesterol concentrations:
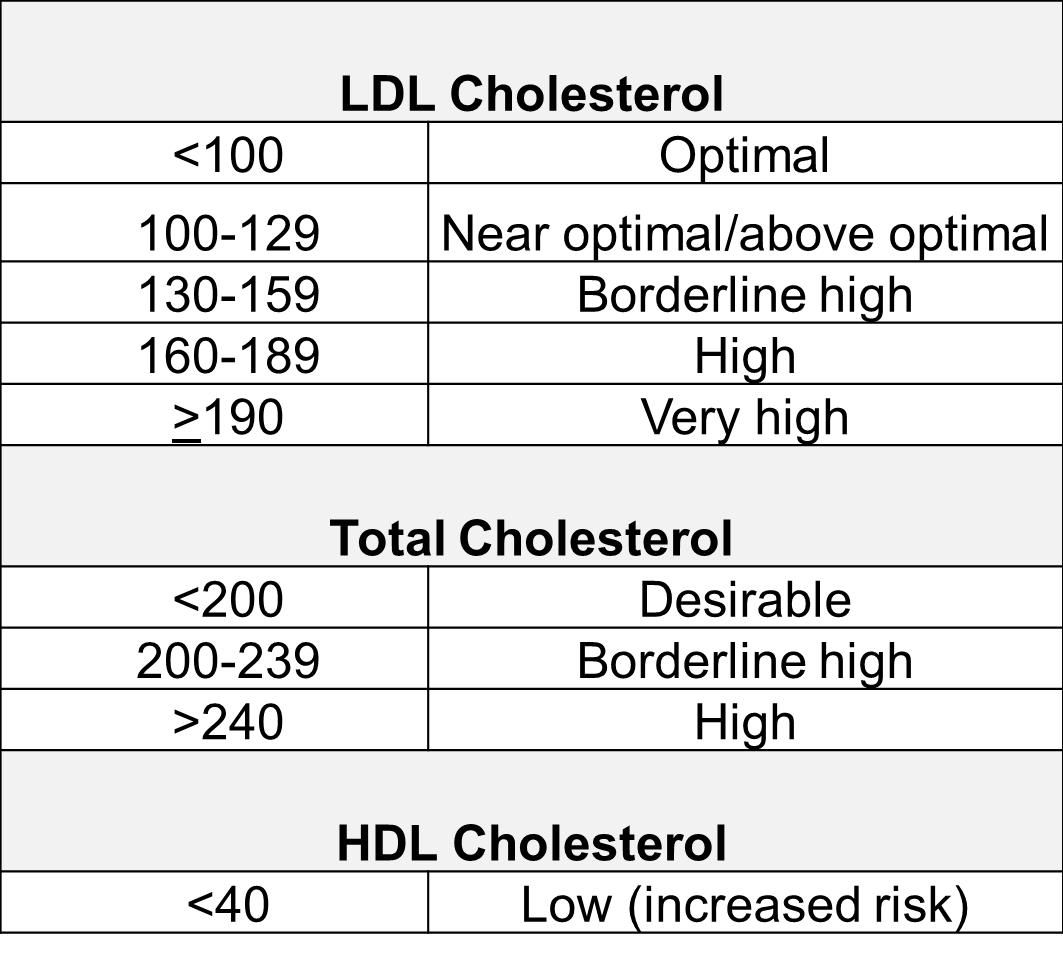
LDL
The evidence that high LDL concentrations play a causal role in coronary artery disease (CAD)is quite compelling.
- Many investigators have convincing demonstrated a progressive increase in risk that correlates directly with LDL concentrations.
- Treatments that lower LDL cholesterol reduce the risk of CAD.
- Genetic studies analyzing SNPs
 show that SNPs affecting LDL cholesterol are consistently related to risk of myocardial infarction. In other words, genetic variants associated with elevated LDL levels are consistently associated with increased risk.
show that SNPs affecting LDL cholesterol are consistently related to risk of myocardial infarction. In other words, genetic variants associated with elevated LDL levels are consistently associated with increased risk. - The presence of LDL in atherosclerotic plaques provides additional evidence of its direct involvement.
Statin Drugs
Statins are currently the most powerful cholesterol-lowering drugs available. They act by inhibiting the action of 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase, which is the rate-limiting enzyme in the sequence of steps by which cholesterol is synthesized in the liver. The liver has two sources of cholesterol: it can take up LDL particles from the blood, or it can synthesis cholesterol using HMG-CoA reductase. The diagram below illustrates cholesterol homeostasis in a liver cell. LDL (shown in red) can bind to LDL receptors on the surface of the liver.
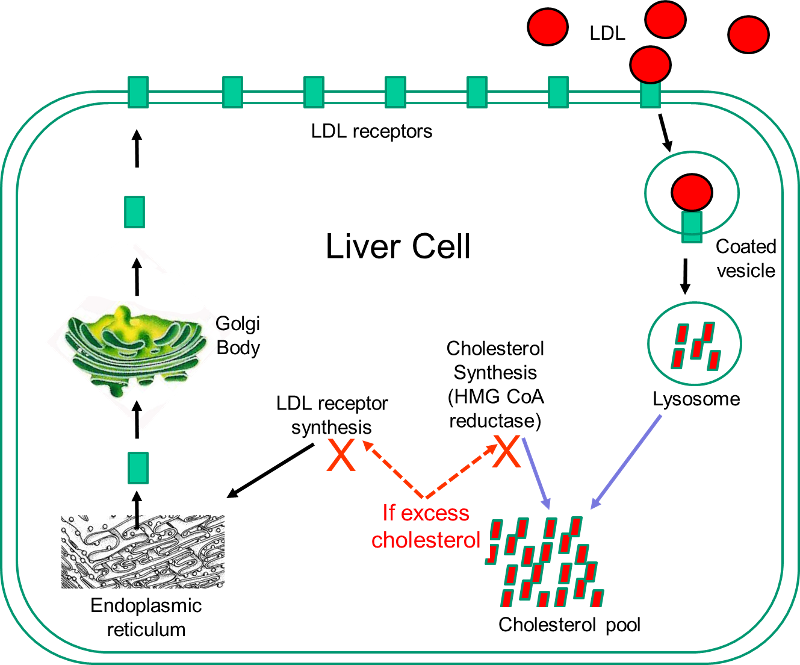
Binding causes the LDL to be taken up by the liver cell and digested in a lysosome. Fatty acids and amino acids in the LDL are recycled, and the cholesterol enters the cholesterol pool in the liver cell. Note that if the liver cell synthesizes cholesterol, this too will be added to the cholesterol pool. If the concentration of cholesterol in the liver cells exceeds a certain level, HMG CoA reductase is inhibited, and the synthesis of LDL receptors is also inhibited.
Statins act by inhibiting HMG-CoA reductase and shutting off internal cholesterol production. In this way, statins reduce cholesterol concentrations in liver cells, which causes increased production of LDL receptors and increased uptake of LDL by the liver. This ultimately results in a lowering of blood concentrations of LDL cholesterol, and this generally results in a slower progression of atherosclerotic plaques and a reduced risk of plaque rupture. However, observers occasionally report regression of atherosclerotic plaques in patient on statins.
While statins are effective in reducing LDL cholesterol levels, they can be associated with side effects.
- Muscle damage manifest as pain, tiredness, or weakness is the most common side effect and ranges from mild discomfort to difficulty in climbing stairs or walking. Statins very rarely cause severe, life-threatening rhabdomyolysis
 which can result in severe muscle pain, liver damage, kidney failure, and death.
which can result in severe muscle pain, liver damage, kidney failure, and death. - Liver damage: Statins can also damage liver cells, resulting in elevated levels of liver enzymes in blood. Liver enzyme levels should be monitored when statins are first started.
- Digestive problems: Some people experience nausea, gas, diarrhea or constipation.
- Rash or flushing
- Increased blood sugar or type 2 diabetes is occasionally seen in patients on statins.
Because of their effectiveness in reducing CAD in patients at high risk, some advocated expanding the use of statins to people who did not necessarily have elevated cholesterol levels. A number of large, well-done clinical trials have demonstrated that statins can reduce the risk of CAD in low-risk individuals, but most experts caution against this because of the cost and the risk of side effects.
|
Statins for Primary Prevention? From The Cochrane Collaboration
"Reducing high blood cholesterol, a risk factor for cardiovascular disease (CVD) events in people with and without a past history of coronary heart disease (CHD) is an important goal of pharmacotherapy. Statins are the first-choice agents. Previous reviews of the effects of statins have highlighted their benefits in people with coronary artery disease. The case for primary prevention, however, is less clear. Fourteen randomized control trials (16 trial arms; 34,272 participants) were included. Eleven trials recruited patients with specific conditions (raised lipids, diabetes, hypertension, microalbuminuria). All-cause mortality was reduced by statins (RR 0.84, 95% CI 0.73 to 0.96) as was combined fatal and non-fatal CVD endpoints (RR 0.70, 95% CI 0.61 to 0.79). Benefits were also seen in the reduction of revascularisation rates (RR 0.66, 95% CI 0.53 to 0.83). Total cholesterol and LDL cholesterol were reduced in all trials but there was evidence of heterogeneity of effects. There was no clear evidence of any significant harm caused by statin prescription or of effects on patient quality of life. Reductions in all-cause mortality, major vascular events and revascularisations were found with no excess of cancers or muscle pain among people without evidence of cardiovascular disease treated with statins. Other potential adverse events were not reported and some trials included people with cardiovascular disease. Only limited evidence showed that primary prevention with statins may be cost effective and improve patient quality of life. Caution should be taken in prescribing statins for primary prevention among people at low cardiovascular risk."
|
HDL
Blood levels of HDL are inversely related to risk of coronary artery disease, and it was thought that low HDL levels represented an independent risk factor. This led to a concerted effort to identify treatments that might prevent CAD by raising HDL concentrations. This area has been very controversial, but recent evidence suggests that although low HDL is inversely correlated with risk of CAD, the relationship is not causal. In other words, low HDL levels are a marker for other factors that cause progression of CAD. Several pieces of evidence suggest this.
- Genetic variants that are associated with high HDL levels are not consistently associated with a reduced risk of CAD. In fact, the same study that found that SNPs associated with high LDL were consistently associated with increased risk failed to show that SNPs associated with HDL had any relationship to risk of CAD. These authors also reported that a genetic variant that specifically and substantially increases plasma HDL cholesterol, did not reduce risk of myocardial infarction.
- Drugs that raise HDL levels do not reduce the risk of CAD.
How is it possible that low HDL is associated with increased risk, but the relationship is not causal? The most likely answer is that low HDL is a marker for other risk factors that do increase risk. Dr. Sekar Kathiresan, one of the coauthors of the article cited above was quoted in the New York Times as saying that a number of other risk factors track with low HDL, including obesity, being sedentary, smoking, insulin resistance, having small LDL particles, and increased coagulation of blood. Thus, the current thinking is that HDL is not a causal factor, but rather a marker for the presence of other causal factors.