Hypertension
Blood pressure is a measure of the force of blood pushing against the arterial walls as the heart pumps blood around the body. Blood pressure is highest when the heart contracts (systole ), and falls when the heart is relaxing and refilling (diastole
), and falls when the heart is relaxing and refilling (diastole ), and pressures in the arteries during these alternating phases are referred to as systolic and diastolic pressures. The figure below shows changes in pressure within large arteries during a single cardiac cycle of contraction and relaxation.
), and pressures in the arteries during these alternating phases are referred to as systolic and diastolic pressures. The figure below shows changes in pressure within large arteries during a single cardiac cycle of contraction and relaxation.
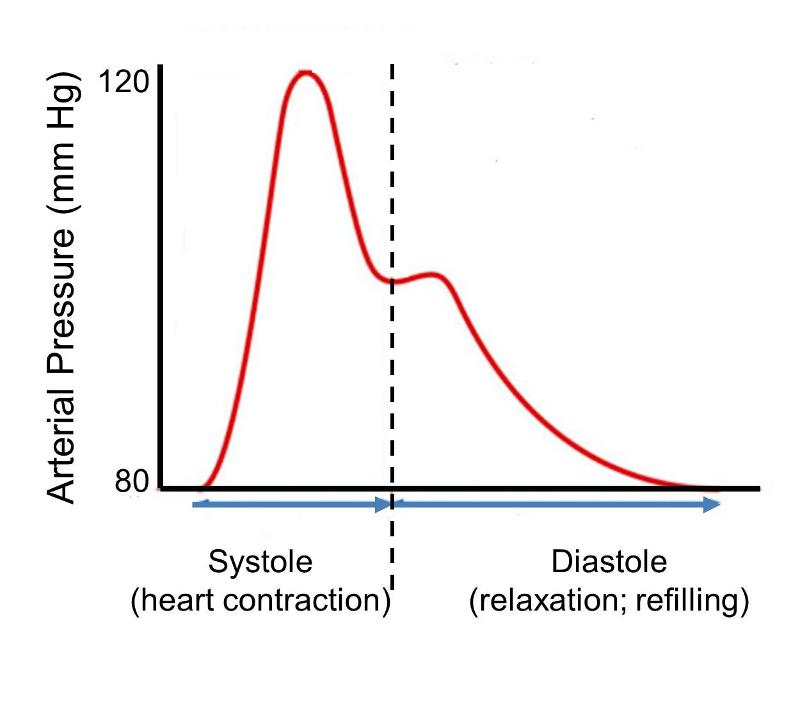
Systolic and diastolic blood pressures vary continually depending on activity and many other factors, and the range of observed pressures vary among individuals. Nevertheless, the image depicts a steeotypic normal adult with minimum diastolic pressure of 80 mm of mercury and a peak systolic pressure of 120 mm of mercury. At the and of diastole the pressure is 80. As systolic contraction begins arterial pressure rises rapidly to a peak of 120 in mid systole and then falls to about 105 by the end of systole. During diastole, when the heart relaxes, pressure declines back to 80 mm of mercury. The small secondary pressure increase in the beginning of diastole is referred to as the 'dicrotic notch' and is due to closure of the aortic valve and elastic recoil of the aortic wall. The pulse pressure depicted here indicates an arterial blood pressure of 120/80, i.e., the first number indicates peak systolic pressure, and the second indicates pressure at the end of diastole. The National Heart, Lung, and Blood Institute defines normal blood pressure at rest as 120/80 or lower. Individuals with resting blood pressures that are consistently greater than 140/90 are considered to have hypertension (high blood pressure). Hypertension leads to endothelium dysfunction. The longer hypertension goes untreated, the more damage it can cause.
Hypertension affects almost 50 million people in the US. Clinical trials have demonstrated that a diet emphasizing fruits, vegetables, low-fat dairy products, whole grains, poultry, fish, and nuts with reductions in red meat, sugar, and total and saturated fat and cholesterol lowers blood pressure in people with and without hypertension. Reducing the sodium chloride content of typical diets in the US or Europe lowers blood pressure.
Facts About Hypertension from the CDC
- About 1 in 3 U.S. adults—an estimated 68 million people—has high blood pressure.
- 69% of people who have a first heart attack, 77% of people who have a first stroke, and 74% of people with chronic heart failure have high blood pressure. High blood pressure is also a major risk factor for kidney disease.
- High blood pressure was listed as a primary or contributing cause of death for about 348,000 Americans in 2008.
- Costs directly attributable to high blood pressure for the nation total almost $131 billion annually in direct medical expenses and $25 billion in lost productivity.
- Less than half (46%) of people with high blood pressure have their condition under control.
- Almost 30% of American adults have prehypertension—blood pressure numbers that are higher than normal, but not yet in the high blood pressure range. Prehypertension raises your risk of developing high blood pressure.
- Reducing average population sodium intake from 3,300 mg to 2,300 mg per day may reduce cases of high blood pressure by 11 million and save 18 billion health care dollars annually.
From a public health perspective high blood pressure is an enormous problem that presents a real opportunity for low-cost, high-impact intervention. Hypertension is highly prevalent and substantially under diagnosed. Moreover, it contributes very significantly to atherosclerotic disease and stroke. Nevertheless, it is an ideal condition for screening , and it can be effectively treated by behavior modification and/or low-cost medication.
, and it can be effectively treated by behavior modification and/or low-cost medication.
Smoking
Smoking increases the risk of atherosclerosis, because components of tobacco smoke generate reactive oxygen species and reduce antioxidants, which causes endothelial dysfunction. Smoking tobacco in any form will have the effect of increasing LDL cholesterol, decreasing HDL cholesterol, and slightly increasing triglycerides. This negatively affects all of the cholesterol levels in the body.
Cholesterol has a direct correlation with atherosclerosis. Nicotine not only causes addiction to smoking cigarettes, but also has a negative effect on the arteries. Nicotine speeds up the heart, raises blood pressure, and constricts the arteries. Carbon monoxide minimizes the oxygen supply that travels to the heart. Both nicotine and carbon monoxide also increase blood clotting and clogging of the arteries.
Smoking accelerates the process of atherosclerosis. Each time a person smokes a cigarette, the blood vessels become sticky from the chemicals in the tobacco smoke, which leads to fat collecting and sticking to the artery walls. Smoking decreases a person's tolerance to exercise, which would help keep the heart strong. It also increases the tendency for the blood to clot due to an increase in the levels of fibrinogen, a protein that can cause the blood to clot. Smoking facilitates the progression of atherosclerosis, which leads to most of the other cardiovascular diseases and coronary heart diseases.
Gender Differences
(See Heart Disease in Women - Harvard Medical School)
Years ago it was believed that women had less risk of coronary artery disease than men, but we now know that the risk is similar, although women tend to develop heart disease about 10 years later than men. The table below shows age-specific mortality from coronary artery disease in men and women.
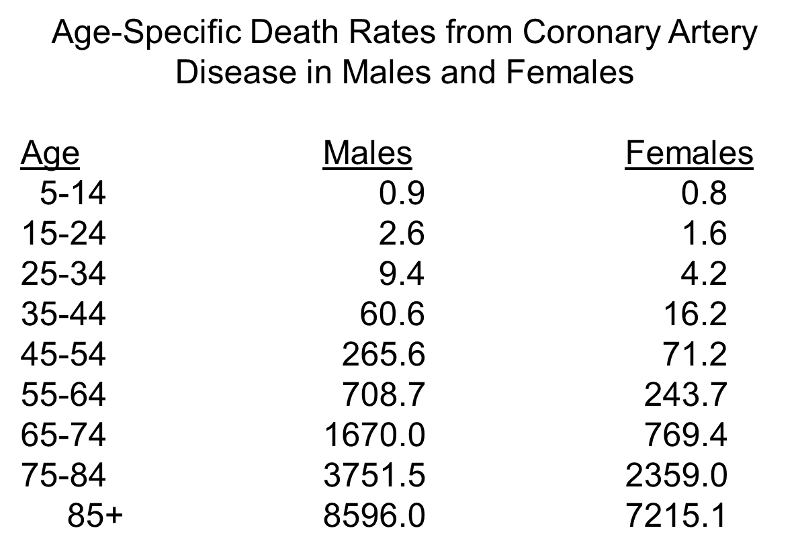
Note, first, the progressive increase in risk with increasing age. The initial age-related increase is greater in men, but after menopause in women (mostly during the 6th decade), the rate in women increases and they begin to catch up to men.
Estrogens give women a somewhat more favorable lipid profile before menopause by increasing HDL (good) cholesterol and decreasing LDL (bad) cholesterol. After menopause, however, women have higher concentrations of total cholesterol than men, and elevated triglycerides become an important risk factor in women, particularly over age 65.
Another important difference is that women frequently don't experience the classic chest pressure and crushing chest pain that often occurs in men. Instead, they may report extreme fatigue or shortness of breath, or they may have nausea or abdominal, neck, or shoulder pain.
Alcohol Consumption
Almost all of the epidemiologic studies that have examined this issue have concluded that moderate alcohol consumption is associated with a 20-40% lower incidence of coronary artery disease and lower risk of mortality from coronary artery disease compared to non-drinkers or heavy drinkers. A number of large prospective cohort studies have demonstrated that moderate drinking lowers the risk of coronary heart disease.
Mukamal KJ, et al.:Roles of Drinking Pattern and Type of Alcohol Consumed in Coronary Heart Disease in Men. N Engl J Med 2003;348:109-18.
This prospective cohort study used The Health Professionals Follow-up Study, which included 51,529 U.S. male dentists, veterinarians, optometrists, osteopathic physicians, and podiatrists 40 to 75 years of age who have been followed since 1986. In 1986 the subjects were asked to report the number of days per week that they typically drank any alcohol, with five response categories. This study included 38,077 men who did not have any history of coronary heart disease in 1986. After 12 years of follow-up, there were 1418 cases of myocardial infarction. The abstract for the report states:
"As compared with men who consumed alcohol less than once per week, men who consumed alcohol three to four or five to seven days per week had decreased risks of myocardial infarction (multivariate relative risk, 0.68 [95 percent confidence interval, 0.55 to 0.84] and 0.63 [95 percent confidence interval, 0.54 to 0.74], respectively). The risk was similar among men who consumed less than 10 g of alcohol per drinking day and those who consumed 30 g or more. No single type of beverage conferred additional benefit, nor did consumption with meals. A 12.5-g increase in daily alcohol consumption over a four-year follow-up period was associated with a relative risk of myocardial infarction of 0.78 (95 percent confidence interval, 0.62 to 0.99)."
A meta-analysis by Ronksley PE, et al. found that light to moderate alcohol consumption was associated with a reduced risk of cardiovascular disease. Relative to non-drinkers, alcohol drinkers had a rate ratio of 0.75 (95% confidence interval 0.70 - 0.80) for cardiovascular disease mortality (21 studies), 0.71 (0.66 - 0.77) for incident coronary heart disease (29 studies), 0.75 (0.68 to 0.81) for coronary heart disease mortality (31 studies), 0.98 (0.91 - 1.06) for incident stroke (17 studies), and 1.06 (0.91 - 1.23) for stroke mortality (10 studies). Their analysis suggested that the lowest risk of mortality from coronary heart disease occurred with 1-2 drinks a day, while the lowest risk for stroke occurred with ≤1 drink per day. Most other large prospective investigations have also found that moderate drinking is associated with lower risk for coronary heart disease.
found that light to moderate alcohol consumption was associated with a reduced risk of cardiovascular disease. Relative to non-drinkers, alcohol drinkers had a rate ratio of 0.75 (95% confidence interval 0.70 - 0.80) for cardiovascular disease mortality (21 studies), 0.71 (0.66 - 0.77) for incident coronary heart disease (29 studies), 0.75 (0.68 to 0.81) for coronary heart disease mortality (31 studies), 0.98 (0.91 - 1.06) for incident stroke (17 studies), and 1.06 (0.91 - 1.23) for stroke mortality (10 studies). Their analysis suggested that the lowest risk of mortality from coronary heart disease occurred with 1-2 drinks a day, while the lowest risk for stroke occurred with ≤1 drink per day. Most other large prospective investigations have also found that moderate drinking is associated with lower risk for coronary heart disease.
An negative association between moderate drinking and lower risk for CHD does not necessarily mean that alcohol itself is the cause of the lower risk. There is always the possibility that residue confounding may be responsible for an apparent beneficial effect. For example, few studies have adjusted for subjects' levels of physical activity, despite evidence physically active people tend to drink more more frequently, and exercise protects against CHD occurrence and mortality. In addition, those who drink wine may be generally more health conscious and follow a more favorable lifestyle.
Aspirin Use
Final report on the aspirin component of the ongoing Physicians' Health Study. Steering Committee of the Physicians' Health Study Research Group. N Engl J Med. 1989;321(3):129-35.
In the middle of the 20th century a number of descriptive studies suggested that people who took aspirin regularly seemed to have a lower risk of myocardial infarction. Subsequent observational studies suggested perhaps a 30% reduction in risk of myocardial infarction, but there were concerns about confounding. Several small clinical trials suggested similar reductions, but the sample sizes were too small to arrive at a solid conclusion. In the early 1980s The Physician's Health Study was conducted to test the hypothesis that 325 mg. of aspirin (one 'adult' sized aspirin, i.e., 325 mg) taken every other day would reduce mortality from cardiovascular disease (N. Engl. J. Med. 320:1238, 1989). Male physicians 40 to 84 years of age living in the US in 1980 were eligible to participate. Physicians were excluded if they had a personal history of myocardial infarction, stroke or transient ischemic attack; peptic ulcer disease; contraindication to aspirin consumption; current use of aspirin, platelet-active drugs or non-steroidal anti-inflammatory agents; intolerance to aspirin; or inability to comply with the protocol. Eligible subjects who met the inclusion criteria and who successfully completed a run-in phase were randomly assigned to receive aspirin or a placebo. Eventually 22,071 physicians were enrolled; 11,037 were assigned to aspirin, and 11,034 were assigned to placebo. The agents (aspirin and placebo) were identical in appearance and were mailed to the subjects.
From the abstract of the final report:
"There was a 44 percent reduction in the risk of myocardial infarction (relative risk, 0.56; 95 percent confidence interval, 0.45 to 0.70; P less than 0.00001) in the aspirin group (254.8 per 100,000 per year as compared with 439.7 in the placebo group). A slightly increased risk of stroke among those taking aspirin was not statistically significant; this trend was observed primarily in the subgroup with hemorrhagic stroke (relative risk, 2.14; 95 percent confidence interval, 0.96 to 4.77; P = 0.06). No reduction in mortality from all cardiovascular causes was associated with aspirin (relative risk, 0.96; 95 percent confidence interval, 0.60 to 1.54). Further analyses showed that the reduction in the risk of myocardial infarction was apparent only among those who were 50 years of age and older."
Patrono C, et al.: Low-Dose Aspirin for the Prevention of Atherothrombosis. N Engl J Med 2005;353:2373-83.
Aspirin acts by inhibiting the action of cyclooxygenases, key enzymes in the conversion of the fatty acid arachidonic acid into prostaglandins. The prostaglandins are important signaling molecules that can be produced by almost all tissues in the body. They are important regulators of physiologic function and key mediators of the inflammatory response. Arachidonic acid is a 20-carbon fatty acid with four double bonds; that is present in the phospholipids in the cell's plasma membrane. The cyclooxygenases exist in two forms, cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2). Low-dose aspirin selectively inhibits COX-1, whereas high-dose aspirin inhibits both COX-1 and COX-2. These act on arachidonic acid to create prostaglandin H2, an intermediate compound that is then converted into any one of several prostaglandins (thromboxane, prostaglandin E2, prostaglandin F2a, and prostacyclin). Thromboxane promotes platelet aggregation and clotting, while prostacyclin, produced primarily by endothelium, promotes vascular relaxation and inhibits platelet aggregation.
The effect of aspirin on prostaglandin synthesis is differential. Mature platelets express only COX-1, but vascular endothelial cells express both COX-1 and COX-2. Thromboxane derived mainly from COX-1 in platelets, and its synthesis is highly sensitive to inhibition by aspirin. In contrast, vascular PGI2 is derived predominantly from COX-2 and is less susceptible to inhibition by low doses of aspirin. As a result, aspirin induces a long-lasting inhibition of thromboxane synthesis and a prolongation of bleeding time. In contrast, low-dose aspirin little effect on prostacyclin (PGI2) production. In individuals with atherosclerotic vascular disease, low dose aspirin has been shown by many studies to reduce the risk of myocardial infarction by about 34%, and it reduces the risk of occlusive stroke by about 25%. However, long-term therapy with low-dose aspirin increases the risk of bleeding (mostly from the gastrointestinal tract) in middle-aged patients. There also appears to be a slight increase in the risk of hemorrhagic stroke. Despite the potential increased risk of bleeding which long term therapy, there is good evidence that low dose aspirin is of benefit to individuals with high risk of cardiovascular disease. On the other hand, the benefit in people with low risk is not clear.
One of the questions that arose after the results of the Physicians' Health Study were reported was whether the results could be generalized to women. This question was finally addressed by a subsequent randomized trial conducted in women and reported by Ridker et al. in 2005.
Ridker RM, et al.: A Randomized Trial of Low-Dose Aspirin in the Primary Prevention of Cardiovascular Disease in Women. N Engl J Med 2005;352:1293-304.
These investigators conducted a clinical trial among 39,876 initially healthy women 45 years of age or older who were randomly assigned to receive 100 mg of aspirin on alternate days or placebo. During roughly ten years of follow-up, there was a 17% reduction in the risk of stroke in the aspirin group (rate ratio = 0.83; 95% confidence interval, 0.69 - 0.99; P=0.04), primarily due to a 24% reduction in ischemic (occlusive) strokes and a non-significant increase in the risk of hemorrhagic stroke (rate ratio =1.24; 95% confidence interval, 0.82 - 1.87; P=0.31). However, aspirin had no significant effect on the risk of fatal or nonfatal myocardial infarction (rate ratio = 1.02; 95% confidence interval, 0.84 - 1.25; P=0.83) or death from cardiovascular causes (rate ratio = 0.95; 95% confidence interval, 0.74 - 1.22; P=0.68). Gastrointestinal bleeding requiring transfusion was more frequent in the aspirin group (rate ratio = 1.40; 95% confidence interval, 1.07 - 1.83; P=0.02). Subgroup analyses showed that aspirin significantly reduced the risk of major cardiovascular events, ischemic stroke, and myocardial infarction among women 65 years of age or older.
A follow-up letter to the editor pointed out that the majority of patients in this study (84.5 percent) had a 10-year risk of less than 5% for an incident myocardial infarction and therefore would not have received aspirin as primary prophylaxis, according to the American Heart Association guidelines. The American Heart Association recommendations indicate that aspirin should be used as primary prevention for coronary events in persons with a 10-year risk of myocardial infarction that is greater than 10%.
In a 2009 statement, the U.S. Preventive Services Task Force issued a recommendation for aspirin therapy based on analysis of evidence from literature since 2002. They recommend aspirin therapy for:
- Men aged 45-79, when the potential benefit of reduction in myocardial infarction outweighs the potential harm from gastrointestinal hemorrhage
- Women aged 55-59, when the potential benefit of reduction in stroke outweighs the potential harm from gastrointestinal hemorrhage
- They did not recommend aspirin therapy for men younger than 45 or women younger than 55.