The Future of MDR-TB & XDR-TB
The result of incorrectly treating for TB or not completing an antibiotic treatment regimen resulted in MDR-TB. To control MDR-TB, second-line drugs were developed. However, in 1993, TB strains further resistant to some of those second-line treatments emerged across the world due to improperly treated MDR-TB. These strains are known as XDR-TB and are a threat to the future of global TB control.
|
|
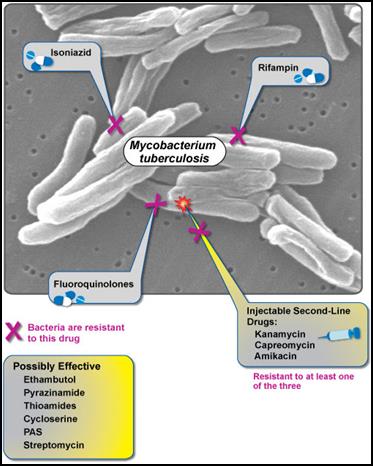
Figure 1: XDR-TB is resistant to fluoroquinolones, isoniazid, rifampin, and at least one second-line injectable drug. Currently, no effective cure is known for XDR-TB. (NIAID, 2007).
According to USAID, XDR-TB is defined as a case of TB resistant to at least isoniazid and rifampicin (among the first-line anti-TB drugs), as well as resistant to any fluoroquinolone treatment and at least one second-line injectable anti-TB drug (amikacin, capreomycin, or kanamycin) (USAID, 2009). XDR-TB evolved to resist the antibiotics because patients stopped taking their pills too early--once they felt better but before their treatment cycle was complete--which failed to kill the MDR-TB in their bodies. By not completing the regime, those patients spared the toughest strains--TB that had mutated to become even less susceptible to the drugs. This is not uncommon in poor countries where patients and clinics are unable to afford any, enough, and the right combinations of the high-quality drugs necessary to defeat the resilient strains (Shufro, 2007). Symptoms and methods of transmission are the same as TB and MDR-TB, but the more resistant the TB, the more difficult the bacteria is to control, the more fatal the disease, and the more dire the prospects. In March, 2013, WHO estimated that of the approximate 310,000 cases of MDR-TB in the world, about 9% were XDR-TB and located in 84 different countries (ALA, 2013).
|
XDR-TB as a Global Problem
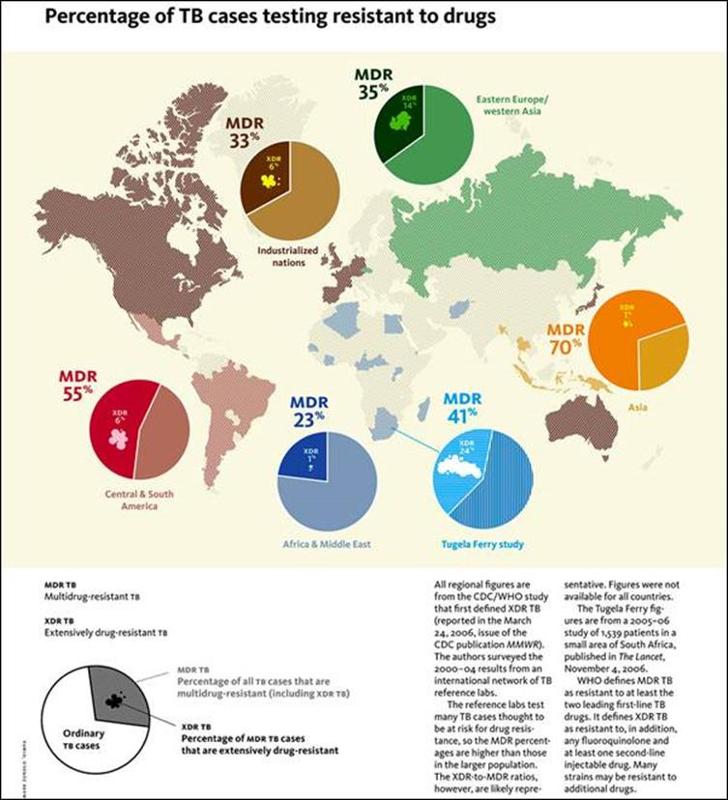
While the number of XDR-TB cases among foreign-born people between 1993 and 2006 was similar, the percentage of foreign-born cases increased from 39% to 76%, whereas the US cases declined. At least 67% of all XDR-TB cases in 2011 were disproportionate among foreign-born people, according to the American Lung Association (ALA, 2013 ). Although more people outside the US are afflicted with XDR-TB, the disease does not discriminate and may easily travel anywhere around the globe, deeming XDR-TB a global issue.
|
|
Figure 2: The map on the left uses data from the CDC/WHO (2006) to show percentages of areas around the world most afflicted with TB, including drug-resistant TB. The pie charts indicate the proportion of TB cases that are MDR-TB and the figures within the MDR-TB pie slices depict the proportion of XDR-TB. Although Asia has the highest percentage of MDR-TB, Eastern Europe/Western Asia has the highest percentage of XDR-TB. The presence of XDR-TB around the world demonstrates the need to quickly suppress TB cases and, in particular, prevent further spread of XDR-TB (Yale Alumni Magazine, 2010).
|
Drugs used to treat MDR-TB in comparison to TB are expensive, the routine treatment complex, and the side-effects more harmful, therefore, the assumption is that the discovery and implementation of effective third-line drugs used to treat XDR-TB will require exponentially more money, time, and effort resulting in drugs that require longer treatment periods and have even more deleterious side-effects. No new TB drugs have been developed over the past 40 years, explains Gerald Friedland, a Yale medical school professor and director of Yale's AIDS program as well as a lead scientist for a TB and HIV co-infection study in South Africa : "'doctors whose patients face resistant TB can't turn to "third-line" drugs: none exists'" (Shufro, 2007). In a CDC pod cast titled "Emergence of Extensively Drug Resistant Tuberculosis," Dr. Peter Cegielski, team leader for drug-resistant TB in the Division of Tuberculosis Elimination at CDC, is asked questions about XDR-TB. He stated that XDR-TB cannot be treated efficiently because efficient treatment calls for at least four effective drugs, which are unavailable for the magnitude of resistance posed by XDR-TB. To add, there are currently no existing third-line drugs powerful enough to cure XDR-TB (CDC, 2008). The third-line drugs that are available include: clofazimine, linezolid, amoxicillin plus clavulanate, imipenem plus cilastatin, and clarithromycin, but their efficacy is unclear and roles undefined (Zumla, Nahid, & Cole, 2013). In addition, "the cost of second-line drugs had always been so high that middle- and lower-income countries couldn't afford them," (CDC, 2008), implying that third-line drugs are also too costly for most afflicted with MDR- and XDR-TB.
Monitoring programs, like DOT, and record-keeping databases, like NTBSS, while effective in treating and controlling for TB, are not as effective for MDR-TB and XDR-TB because not all cases of resistant TB are diagnosed correctly. As Dr. Cegielski states, "not every lab tests every isolate for all of the second-line drugs"(CDC, 2008); resistance may not be just due to one drug, but a combination of drugs (CDC, 2008); and testing may take weeks to months to confirm resistance. According to scientists studying the effectiveness of innovative drug-resistant-TB technology, "the burden of XDR-TB is increasing due to inadequate monitoring, lack of proper diagnosis, and treatment" (Singh, Maurya, Kant, Umrao, Kushwaha, Nag, & Dhole, 2013). The technique of diagnosing resistant TB via sputum sample, used in poor countries, is antiquated and time-consuming (Shufro, 2007). To prevent the further spread of XDR-TB, locating and confirming cases early and quickly, allocating necessary effective third-line drugs, and monitoring treatment regimes of those with the disease before individuals transmit the bacteria are crucial requirements for decreasing the incidence and prevalence of XDR-TB across the globe.
Without effective, accessible, and affordable third-line drugs and monitoring programs to ensure proper diagnosis and treatment compliance, XDR-TB will continue to be a global threat affecting a myriad of people across the globe, and particularly in developing and impoverished nations.