HIPAA
The Health Insurance Portability and Accountability Act (HIPAA)
The Health Insurance Portability and Accountability Act (HIPAA) was enacted in 1996 to address confidentiality of patient information and to confer certain patient rights with regard to information contained in their medical records.
Watch the following videos:
|
Privacy Rights in Your Health Information Privacy and Protection |
The Internet and e-Health
The Internet has made patients more active participants in their own health care. e-Health includes all forms of electronic health care delivered over the Internet (information, education, products, services, etc.)
Other applications include:
- Registering patients
- Pharmaceutical ordering
- Early notice for physicians or updates prior to hospital rounds/visits
- Virtual visits
The Internet and E-health have seen increased use by patients and physicians. Certain applications can make physicians more productive. For certain health conditions, virtual visits are appropriate for monitoring and follow up. But telemedicine has faced several barriers as well, such as problems with licensure of physicians and other providers across state lines, concerns about legal liability, lack of reimbursement, and questionable cost-effectiveness. But, many remote in-home patient monitoring programs are proving to be cost-effective. So, time will tell, and more research and evaluation will be needed.
Read E-Health Opportunities for Seniors
Connecting more older Americans to the Internet is expected to improve opportunities to protect their well-being and reduce national costs for care.
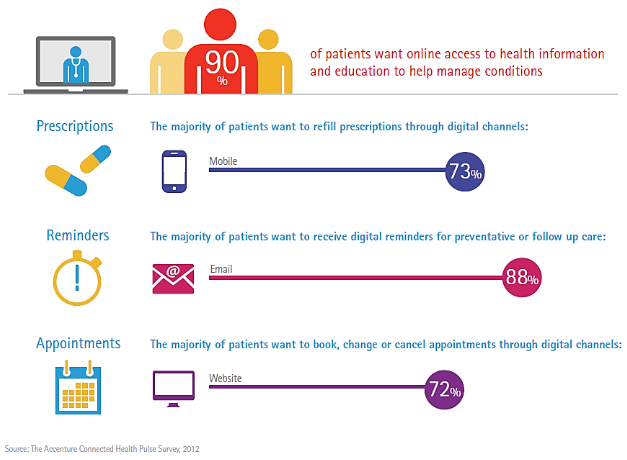
Infographic: Most Patients Want to Self-Manage Healthcare Online
The iPad in the Workplace
See the following articles on the use of the iPad in the workplace, including health care, as well as the war between iPad, Android, Blackberry, HP, and other medical tablets. Physicians may be ready to use them, but are hospitals and clinical environments ready to accommodate their needs?
Read the following article from the Science secion of the New York Times: Redefining Medicine with Apps and iPads
Keeping in mind the various aspects of medical and information technology, as well as EHR, HIPAA, and privacy issues, let's now expand our discussion to include more real concerns about patient safety, medical errors, and health communication. The use of apps for self-monitoring is becoming more of a controversy on several fronts. One concern is privacy and how much of what an individual enters into an app is shared for commercial interests. Consumers have no HIPAA protection here and there is big money in data mining for industry. How many of us read and think about each word when we agree to a 'terms of use' screen? Another concern is with the quality of the information in the applications. As more consumers use apps in managing health and illness the stakes get higher. Providers use these as well in clinical decision making. On the other hand the ability for an individual to track and compare health behaviors (exercise, sleep, water intake, food diary) is powerful and may contribute to improved health habits. I am personally very motivated (maybe over motivated some days) by my Fitbit. I set goals and complete against myself. I am also a fan of GPS mapping my bike trips and get excited when I see I am getting faster, going further, or that I conquered higher elevation. Other people prefer to share and complete with others on Facebook and other online communities. Currently the Food and Drug Administration (FDA) does not regulate these apps. The Federal Trade Commission (FTC) also has a stake, since part of their mission is to protect consumers against false claims to and misleading advertising.
What about use of social media by the health care workforce? Where should lines be drawn? This will continue to be a high growth area and an opportunity for health communicators. Listen to the two brief NPR pieces below.
|
http://www.npr.org/player/v2/mediaPlayer.html?action=1&t=1&islist=false&id=155977692&m=156577709 http://www.npr.org/player/v2/mediaPlayer.html?action=1&t=1&islist=false&id=166240156&m=166381967
|
Telemedicine: Benefits and Challenges
Telemedicine is a rapidly developing application of clinical medicine where medical information is transferred through interactive audiovisual media for the purpose of consulting, videoconferencing, remote medical procedures, or examinations. Telemedicine generally refers to the use of communications and information technologies for the delivery of clinical care.
Telemedicine has several forms
- Real-time communication between a health care provider and a patient using technology (audio and video, often with transmission of data from devices at location of patient)
- Real-time communication between providers either about a specific patient (often a consultation with specialists or for educational purposes
- Forwarding of digital information between practitioners (radiology images, pictures of skin findings)
Telemedicine is seen as a way to increases access to care, especially in rural areas and for the homebound. Challenges in telemedicine include security of information transmission, lack of standards for reimbursement, scope of practice issues if the patient and provider are in different states, and liability.
Telemedicine can extend access to individuals in remote areas or to those patients confined to home. For this week you were asked to read an example from rural areas of South Dakota. Imagine someone you care about needing emergency care and needing to travel 200 miles to be seen by a physician with the necessary training and expertise.
A particularly vulnerable population is veterans receiving care at the Veteran's Health Administration. Remember that VA coverage is generally coverage at VA locations. It is not the same as having an insurance care to use in other locations. Veterans live across the country, including rural areas. VHA facilities are across the nation, certainly not accessible to all.
|
Source: NPR.org
|




