Ambulatory Care
Medical care is divided into two categories - inpatient and ambulatory care. Ambulo is Latin for walk, so you can think of ambulatory care as patients walking in and out of the facility on the same day. Much of ambulatory care takes place in small physician practices. This is rapidly changing as mergers and consolidations bring more practices under the auspices of a larger hospital. Many medical school graduates in ambulatory care are choosing to become hospital employees instead of working inindependent practice settings.
Ambulatory care settings:
- Private offices
- Free standing HMOs
- Hospital ambulatory care services
- Diagnostic centers (MRI)
- Ambulatory surgical centers (minor procedures on eyes, joints, cosmetics)
- Urgent care centers, incudingincluding those in pharmacies and stores
When looking at office visits by type, including hospital clinics, primate offices, community health centers and HMOs, we generally divide them into primary care visits and specialty care visits. Specialty care if further divided into medical and surgical specialties.
Primary Care
|
"Primary care is the level of a health services system that provides entry into the system for all new needs and problems, provides person-focused (not disease-oriented) care over time, provides care for all but very uncommon or unusual conditions, and coordinates or integrates care, regardless of where the care is delivered and who provides it. It is the means by which the two main goals of a health services system, optimization and equity of health status, are approached." |
The acronym PCP has two meanings. I refer to the broader term Primary Care Providers, which may be a physician, nurse practitioner or physician's assistant. You will also see this used for the more narrow Primary Care Physician. Primary care providers see patients in a range of locations: hospital outpatient departments, free-standing practices, community health centers*, schools, and as home visits.
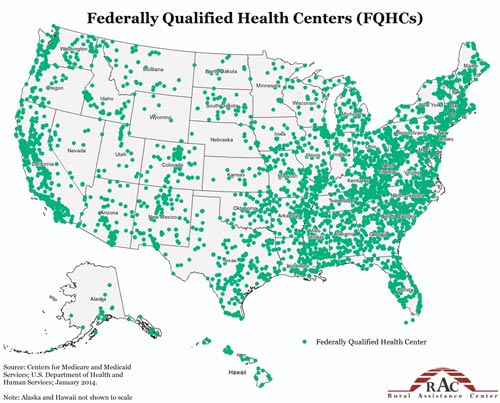
Community health centers (CHCs) are located in underserved areas (urban and rural). These organizations provide comprehensive primary care services to those in their geographic area. These are safety-net providers and do not turn away uninsured patients. CHCs vary in their degree and mode of federal support, they are all are not-for-profit organizations. Some CHCs are Federally Qualified Health Centers (FQHC).
Intended Impact of the ACA on Primary Care
- Increase workforce for physicians and other professionals:
- Increased training slots
- Expand the National Health Services Corps
- Loan forgiveness for those agreeing to work in underserved areas
- Federally Funded Community Health Center (CHC) expansion and new construction
- Increase Medicaid payments to primary care visits to the level of Medicare
- Extra payments from Medicare to physicians in primary care
- Many of the essential benefits and preventive services covered in the ACA without cost sharing are primary care related and will bring more patients into primary care
Potential Adverse ACA Impact on Primary Care
You may want to review the excellent piece on access by Aaron Carroll (Why Improving Access to Health Care Does Not Save Money).
When thinking about the expansion of insurance coverage it is important to remember the following:
- Increasing the number of insured will increase demand (remember that access increases utilization).
- It is unclear if the already strained primary care system can handle the volume (could even create an access problem for the previously insured).
- Expect an increase in system cost for primary care services.
- One cannot assume/conclude this will result in a decrease in system costs in other medical care areas. One cannot assume this will decrease utilization in other areas or improve population level health (especially chronic conditions).

