
Primary Care, PCMHs, and ACOs
|
|
This module focuses on primary care, and it will also include discussions of the Patient-Centered Medical Home (PCMH) and Accountable Care Organizations (ACO).
|
|

Medical care is divided into two categories - inpatient and ambulatory care. Ambulo is Latin for walk, so you can think of ambulatory care as patients walking in and out of the facility on the same day. Much of ambulatory care takes place in small physician practices. This is rapidly changing as mergers and consolidations bring more practices under the auspices of a larger hospital. Many medical school graduates in ambulatory care are choosing to become hospital employees instead of working inindependent practice settings.
Ambulatory care settings:
When looking at office visits by type, including hospital clinics, primate offices, community health centers and HMOs, we generally divide them into primary care visits and specialty care visits. Specialty care if further divided into medical and surgical specialties.
|
"Primary care is the level of a health services system that provides entry into the system for all new needs and problems, provides person-focused (not disease-oriented) care over time, provides care for all but very uncommon or unusual conditions, and coordinates or integrates care, regardless of where the care is delivered and who provides it. It is the means by which the two main goals of a health services system, optimization and equity of health status, are approached." From: The Johns Hopkins Primary Care Policy Center |
The acronym PCP has two meanings. I refer to the broader term Primary Care Providers, which may be a physician, nurse practitioner or physician's assistant. You will also see this used for the more narrow Primary Care Physician. Primary care providers see patients in a range of locations: hospital outpatient departments, free-standing practices, community health centers*, schools, and as home visits.
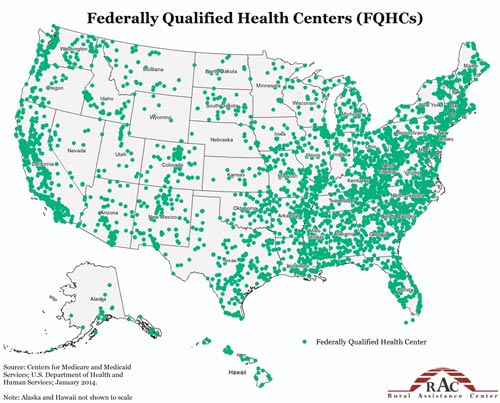
Community health centers (CHCs) are located in underserved areas (urban and rural). These organizations provide comprehensive primary care services to those in their geographic area. These are safety-net providers and do not turn away uninsured patients. CHCs vary in their degree and mode of federal support, they are all are not-for-profit organizations. Some CHCs are Federally Qualified Health Centers (FQHC).
You may want to review the excellent piece on access by Aaron Carroll (Why Improving Access to Health Care Does Not Save Money).
When thinking about the expansion of insurance coverage it is important to remember the following:
The patient centered medical home is a model of care. It is not about a physical location. The PCMH could be in a physician practice, or in a patient's own home. The PCMH is about the organization and delivery of primary care services.
Family Centered Medical Home
 The family centered medical home is American Academy of Pediatrics (AAP) model for delivering primary care to all children and youth, including children and youth with special health care needs. Remember in pediatrics that the 'patient' is the family as care of children is always within the family context.
The family centered medical home is American Academy of Pediatrics (AAP) model for delivering primary care to all children and youth, including children and youth with special health care needs. Remember in pediatrics that the 'patient' is the family as care of children is always within the family context.
Watch the video below from the American Academy of Pediatrics' National Center on Medical Home Implementation.
|
What is the medical home approach to care? - Calvin C.J. Sia, MD, FAAP
|
Defining elements of the PCMH from the AHRQ Patient Centered Medical Home Research Center:
1. Comprehensive Care
2. Patient-Centered
3. Coordinated Care
4. Accessible Services
5. Quality and Safety
In theory the PCMH is a solution to many of our challenges in health care: fragmented care, duplication of services, excessive use of specialty care, and lack of preventive services.
Here is where the acronyms start to jumble up. Remember the PCMH is not a type of insurance or payment. It was in existence in pediatrics long before the ACA was created. We are going to start out with what I think of as the capital A, capital C, capital O. These ACOs were established in the ACA and are expressly for Medicare patients. This is not the same as Medicare Part C or Medicare Advantage Programs.
The ACO is a new payment structure created for the Medicare population as part of the ACA. The provider organization is responsible for all of the care needs for the group of enrolled patients. The outcomes in terms of quality, cost, and patient satisfaction determine payments. The ACO is complex, and we will not cover the specific details, consider this to be an overview.
The ACO goes beyond the primary care office, but the primary care practice may be the face of the ACO for the patient. Many ACOs may also be PCMH in how they chose to structure and deliver care services. Providers are NOT required to be in an ACO to see Medicare patients, this is an optional program.
Note: Private payors have created their own structures for accountable care. These plans may have very similar design to the Medicare ACO, but were not part of the ACA.
What is an ACO and how is it defined by the Centers for Medicare and Medicaid Services (CMS)?
|
"Authorized legal entity composed of a group of providers and suppliers of services (e.g., hospitals, physicians, and others involved in patient care) that will work together to manage and coordinate care for the patients they serve in original Medicare." |
According to the CMS, there are multiple models including group practice arrangements, networks of individual practices, partnerships or joint ventures, arrangements between hospitals and ACO professionals, hospitals employing ACO professionals.
|
Aspects of Accountable Care Organizations
In contrast, Health Maintenance Organizations (HMOs) have responsibility AND control. |
ACOs are not a panacea. In fact, some health care economists fear that the race to form ACOs could have a significant downside that would actually drive health costs up: hospital mergers and provider consolidation. By becoming integrated systems, many ACOs are joining forces to buy physician practices, leaving fewer independent hospitals and doctors which could lead to greater market power and more leverage in negotiations with insurers (which could potentially increase health costs.)
|
Frequently Asked Questions
|