Asthma
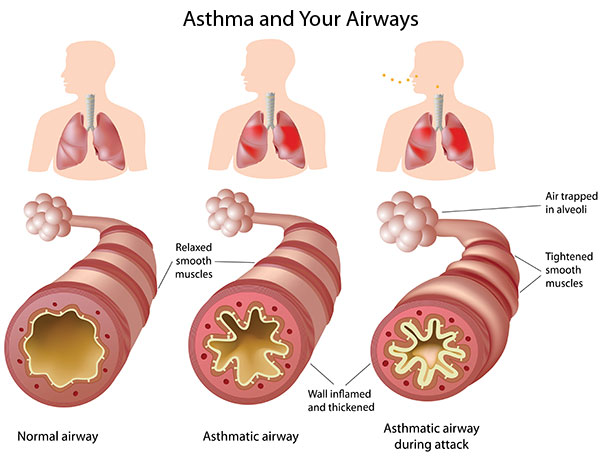
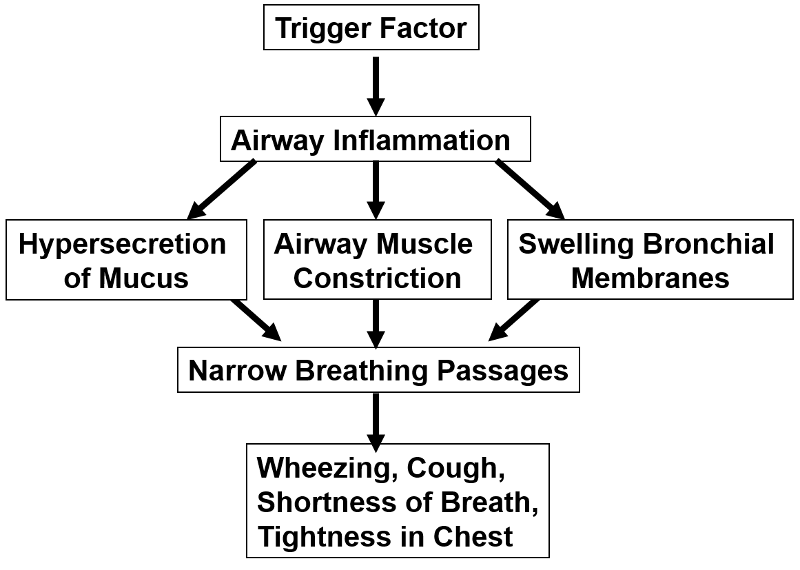
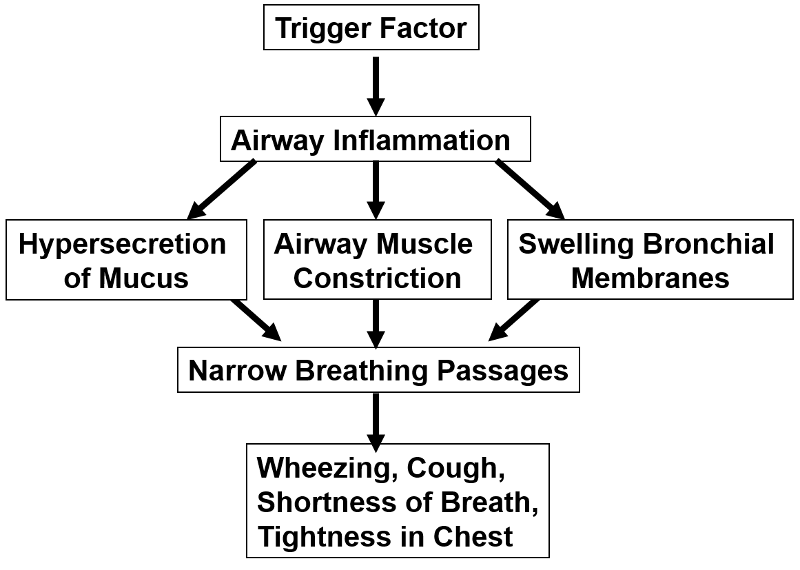
Asthma is a common, chronic syndrome characterized by intermittent episodes of symptoms, which can be severe and life-threatening. The clinical episodes are triggered by antigens, viruses, exercise, or inhalation of irritating substances. Any of these stimuli can trigger a hyperactive allergic response which produces:
- Inflammation of the respiratory tract,
- bronchoconstriction, and
- hypersecretion of mucus
Source: Image source: http://www.nlm.nih.gov/medlineplus/magazine/issues/fall11/articles/fall11pg4.html
These, in turn, cause varying degrees of airflow obstruction, causing shortness of breath, wheezing, cough, tightness in the chest, and sometimes severe "air hunger" and panic. The episodes can resolve spontaneously, but they can be severe, unrelenting and fatal if not treated. The audio files below give an indication breath sounds during auscultation with a stethoscope in a normal person and in a person having an acute asthma attack.
Normal breath sounds
Breath sounds during an asthma attack
The CDC estimates that approximately 20 million Americans have asthma. Asthma is more common in children than in adults, more common in women compared with men, and more common in blacks than in whites. The mortality from asthma rose in the 1980s, but then plateaued, and mortality rates have declined since 1999, probably due to improved treatment.
Asthma Facts from EPA
Asthma Pathophysiology
The pathophysiologic basis of asthma is not well understood. It appears to have a complex, multifactorial etiology which results from an interplay of many hereditary factors and a number of environmental factors. Bronchial biopsies from patients with even mild asthma have evidence of chronic inflammation, and cytokines and other mediators of inflammation are found in bronchial washings from asthma patients. Some families are more prone to development of allergies, and there is a well-known association between allergies and asthma. This suggests a genetic predisposition, but it appears that a number of genes are involved. Allergic reactions are mediated by antibodies of the IgE class. People who are prone to IgE-mediated allergic reactions are said to be "atopic meaning that they have a genetic predisposition to make IgE antibodies in response to certain allergens. While allergic reactions are mediated by IgE antibodies, T and B lymphocytes play an important role in the production of IgE. There are two types of T helper cells (Th lymphocytes) designated Th1 and Th2. Th1 cells tend to promote cell-mediated immune responses by producing interferon-gamma, interleukin-2 (IL-2), and TNF-β. In contrast, Th2 cells promote the production of IgE antibodies by producing IL-4 and IL-13, which are interleukins that act B lymphocytes (B cells) to promote the production of IgE antibodies to a specific antigen. People who are prone to develop allergies, i.e., atopic people, are believed to have a higher ratio of Th2/Th1 cells, and this is believed to be an important factor in their tendency to produce allergy-mediating IgE antibodies. These observations are clearly relevant to asthma, since biopsies of the bronchial mucosa of patients with asthma have an excess of activated Th2 cells. Many authors take these observations to indicate that an imbalance in Th2/Th1 plays an important role in the development of allergies and, specifically, of asthma.
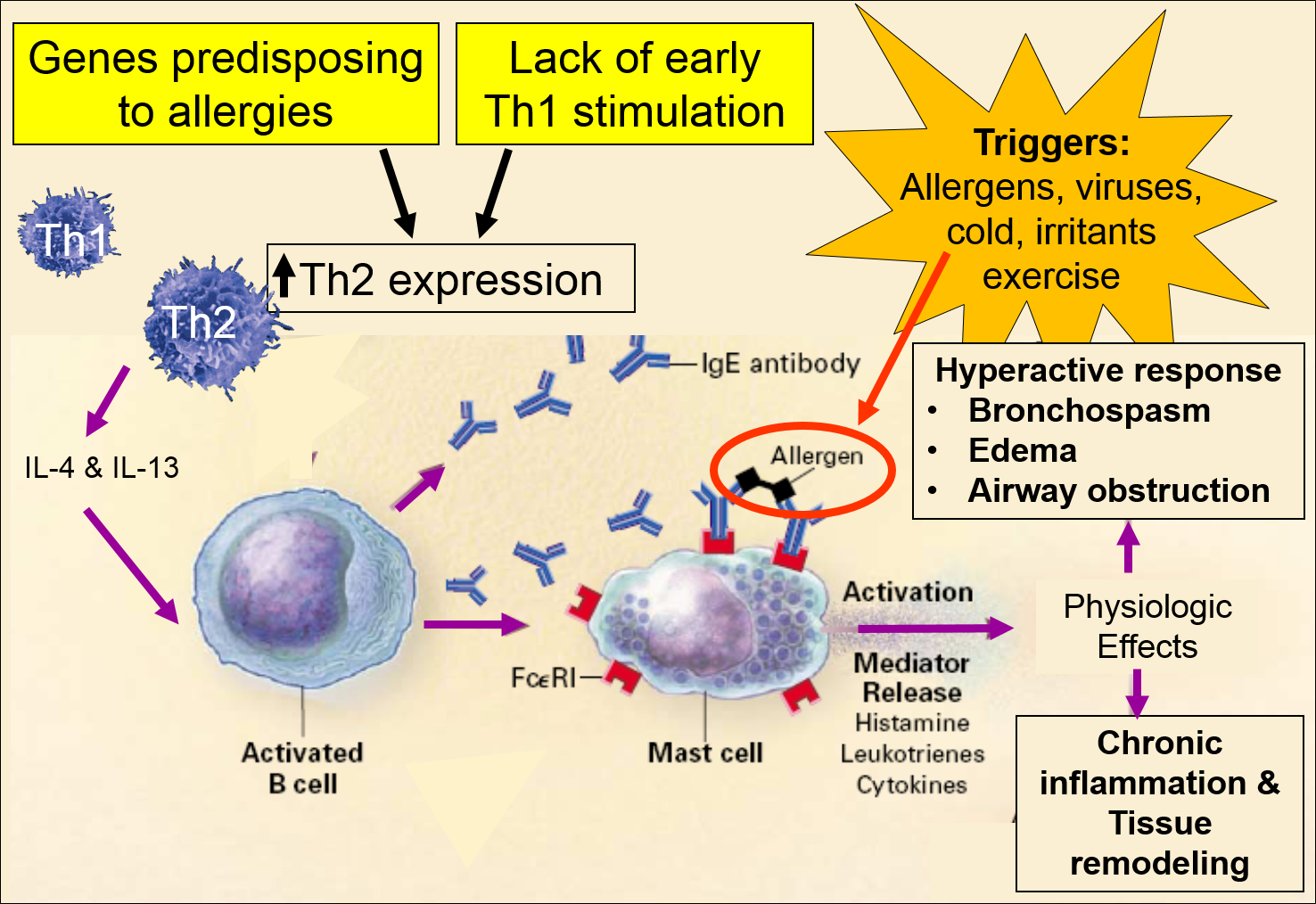
Image adapted from: Busse W. & Lemanske R: N. Engl. J. Med. 2001;344(5):350-362
The Hygiene Hypothesis
Genetic factors clearly play a role in predisposing to allergic reactions, but there is also evidence to suggest that environmental exposures in utero and in early infancy also play a role. This is supported by the increasing prevalence of asthma in industrialized parts of Western countries and an increased prevalence in urban environments compared to rural settings. Epidemiologic studies indicate that certain exposures in early life are associated with stimulation of Th1 mediated responses and a decreased risk of developing asthma and other allergic disorders. These include:
- infection with Mycobacterium tuberculosis, measles virus, or hepatitis A virus
- increased exposure to infectious agents through contact with older siblings
- attendance at a day-care facility during the first six months of life
- early exposure to farm animals, cats, and dogs
In contrast, widespread use of antibiotics may increase the risk of allergies by impairing the development Th2-mediated responses. Newborn infants generally have a preponderance of Th2 cells, and it may be that early exposure to antigens from certain infectious agents may be critical to promoting an appropriate balance between Th2 and Th1 mediated responses. As a result, the combination of genetic predisposition and understimulation of Th1-immune responses may set the stage for later development of allergies and, specifically, asthma.
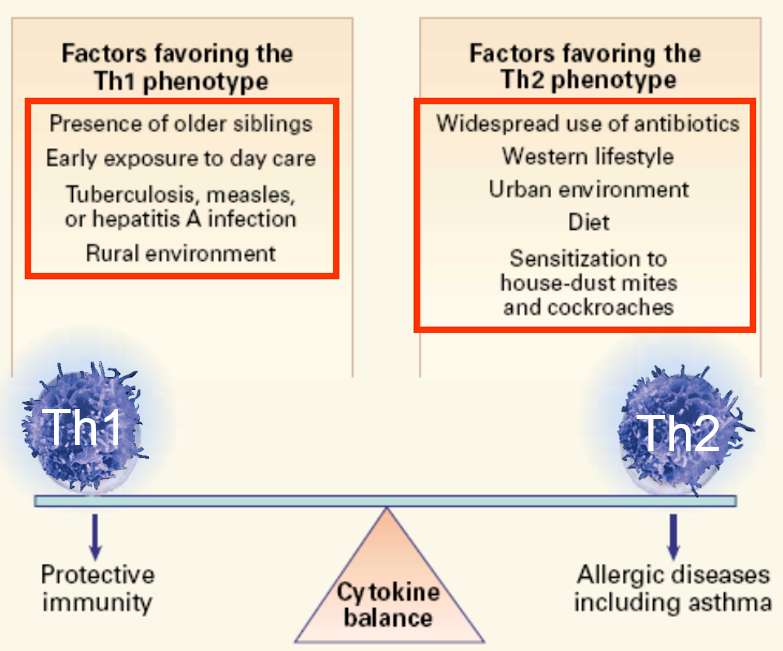
Image adapted from: Busse W. & Lemanske R: N. Engl. J. Med. 2001;344(5):350-362
Allergen Sensitization
Hereditary factors and failure to stimulate Th1 immune response set the stage for allergies , and the final phase is sensitization to one or more allergens
, and the final phase is sensitization to one or more allergens , which then act as the triggers for acute allergic or asthmatic reactions. The initial exposure to an antigen evokes a primary immune response. For example, when an allergen like pollen is inhaled, it is phagocytized by dendritic cells
, which then act as the triggers for acute allergic or asthmatic reactions. The initial exposure to an antigen evokes a primary immune response. For example, when an allergen like pollen is inhaled, it is phagocytized by dendritic cells in the epithelium. After internalization, the dendritic cell breaks down the components and "presents" the antigen fragments on their cell surface where they can activate specific T lymphocytes with receptors that bind to specific epitopes on the fragment. Th2 lymphocytes activate B-lymphocytes which then transform into plasma cells that manufacture IgE antibodies specific for the particular antigen. The IgE-antibodies enter the circulation for distribution. One portion of the IgE antibody binds to receptors on mast cells, but another portion of the IgE remains available to bind to the allergen. If the allergen binds to the IgE on the mast cell, the mast cell becomes activated to release histamine, leukotrienes, and other cytokines. Subsequent exposures to the antigen result in a secondary immune response (memory response) which is much more rapid and vigorous than the primary immune response. Allergen-specific IgE is rapidly produced, and mast cells degranulate and release an array of inflammatory mediators which cause edema, hypersecretion of mucus, and bronchoconstriction by caused contraction of smooth muscle cells surrounding the airways. In addition to episodic acute asthmatic attacks, asthmatics also have remodeling of the the airways which results in thickening and chronic presence of increased numbers of inflammatory cells and mediators.
in the epithelium. After internalization, the dendritic cell breaks down the components and "presents" the antigen fragments on their cell surface where they can activate specific T lymphocytes with receptors that bind to specific epitopes on the fragment. Th2 lymphocytes activate B-lymphocytes which then transform into plasma cells that manufacture IgE antibodies specific for the particular antigen. The IgE-antibodies enter the circulation for distribution. One portion of the IgE antibody binds to receptors on mast cells, but another portion of the IgE remains available to bind to the allergen. If the allergen binds to the IgE on the mast cell, the mast cell becomes activated to release histamine, leukotrienes, and other cytokines. Subsequent exposures to the antigen result in a secondary immune response (memory response) which is much more rapid and vigorous than the primary immune response. Allergen-specific IgE is rapidly produced, and mast cells degranulate and release an array of inflammatory mediators which cause edema, hypersecretion of mucus, and bronchoconstriction by caused contraction of smooth muscle cells surrounding the airways. In addition to episodic acute asthmatic attacks, asthmatics also have remodeling of the the airways which results in thickening and chronic presence of increased numbers of inflammatory cells and mediators.
While the pathophysiologic basis of asthma is far from complete, this discussion attempts to summarize the basic aspects of our current understanding.
Asthma Triggers
- Allergens:
- Inhaled: pollen, dust, molds, animal dander, cockroach allergens
- Ingested: e.g., shellfish
- Tobacco smoke (active or passive): a common trigger.
- Exercise/activity: can trigger asthma (especially in cold air), as well as laughing, crying, holding one's breath, and hyperventilating.
- Weather: Cold air, wind, rain, and sudden changes in the weather can bring on an asthma episode in some people.
- Medications:
- Air pollutants & irritants: paint fumes, smog, aerosol sprays & even perfume.
- Sinusitis
- Respiratory Tract Infections: including flu & common cold (Flu shots would decrease hospitalizations from asthma.)
- Sulfites — preservatives added to some perishable foods
- Emotional stress
- GERD (gastroesophageal reflux disease): aspiration of gastric
- Some occupational exposures (chemicals and irritants)
Environmental Remediation for Asthma
The medical management of asthma and treatment of acute attacks has improved substantially, but the prevalence of asthma continues to rise in urban settings in industrialized Western countries. There is still controversy about the hygiene hypothesis, and it is not yet clear that early exposure to certain antigens could be exploited as a preventive measure. Given what is known about asthma, avoidance of asthma trigger factors would be expected to at least reduce the frequency and severity of symptoms. EPA recommendations for an "Asthma Friendly House" are shown in the iFrame below.
EPA Recommendations Asthma Friendly House
For additional measures, also see the EPA Home Environment Checklist.
There is some evidence that interventions to reduce dust, animal dander, mold, and exposure to cockroaches are effective, but the literature indicates that allergen reduction is difficult to achieve and the effectiveness is not as great as expected. The four articles cited below (one randomized clinical trial and three systematic reviews of the literature) suggest that environmental remediation interventions that target one or two potential targets are of limited, if any value. However, they suggest that multifaceted interventions can reduce symptoms, school absences, and hospital visits for acute asthma care.
From the Abstract:
"We enrolled 937 children with atopic asthma (age, 5 to 11 years) in seven major U.S. cities in a randomized, controlled trial of an environmental intervention that lasted one year (intervention year) and included education and remediation for exposure to both allergens and environmental tobacco smoke. Home environmental exposures were assessed every six months, and asthma-related complications were assessed every two months during the intervention and for one year after the intervention.
Results
For every 2-week period, the intervention group had fewer days with symptoms than did the control group both during the intervention year (3.39 vs. 4.20 days, P<0.001) and the year afterward (2.62 vs. 3.21 days, P<0.001), as well as greater declines in the levels of allergens at home, such as Dermatophagoides farinae (Der f1) allergen in the bed (P<0.001) and on the bedroom floor (P=0.004), D. pteronyssinus in the bed (P=0.007), and cockroach allergen on the bedroom floor (P<0.001). Reductions in the levels of cockroach allergen and dust-mite allergen (Der f1) on the bedroom floor were significantly correlated with reduced complications of asthma (P<0.001)."
Summary:
"Asthma is a chronic inflammatory disease of the airways. The prevalence of asthma has increased and it is now the commonest chronic disease among children. Asthma is triggered by allergens (substances that cause an allergic reaction) and house dust presents a problem in some people with asthma. The major allergen in house dust comes from mites and it is hypothesized that controlling exposure to house dust mites will reduce asthma symptoms in people who are sensitive to house dust mites.
We included 55 randomized trials on 3121 people with asthma. There are both chemical (10 trials) and physical methods such as mattress encasings (37 trials) of reducing mite allergen levels and we included both types in this review. There were also eight trials that used both physical and chemical methods. Many trials were of poor quality and would therefore be expected to exaggerate the reported effect, but we did not find an effect of the interventions. There was no difference in peak flow (a measure of lung function), asthma symptoms and medication scores, or the number of patients reporting an improvement in their asthma symptoms.
While reducing exposure to house dust mites is recommended in guidelines, we did not find an effect of control measures to reduce the exposure to mites or their products." .
From the Abstract:
"Evidence synthesis
In the 20 studies targeting children and adolescents, the number of days with asthma symptoms (symptom-days) was reduced by 0.8 days per 2 weeks, which is equivalent to 21.0 symptom-days per year (range of values: reduction of 0.6 to 2.3 days per year); school days missed were reduced by 12.3 days per year (range of values: reduction of 3.4 to 31.2 days per year); and the number of asthma acute care visits were reduced by 0.57 visits per year (interquartile interval: reduction of 0.33 to 1.71 visits per year). Only three studies reported outcomes among adults with asthma, finding inconsistent results.
Conclusions
Home-based, multi-trigger, multicomponent interventions with an environmental focus are effective in improving overall quality of life and productivity in children and adolescents with asthma. The effectiveness of these interventions in adults is inconclusive due to the small number of studies and inconsistent results. Additional studies are needed to (1) evaluate the effectiveness of these interventions in adults and (2) determine the individual contributions of the various intervention components."
Summary
"Although many studies evaluating a single environmental control strategy fail to show an improvement in clinical outcomes, comprehensive environmental controls may provide some benefit. Additionally, studies that relocate patients to low allergen environments tend to demonstrate clinical improvement."
Additional References for Asthma
- National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. (MD): National Heart, Lung, and Blood Institute (US); 2007 Aug. Section 2, Definition, Pathophysiology and Pathogenesis of Asthma, and Natural History of Asthma.
- Lang DM, Erzurum SC, Kavu M: Asthma. 20th Annual Board Review Symposium. Cleveland Clinic.
- Busse W. & Lemanske R: Advances in Immunology: Asthma. N Engl J Med, 2001;344(5):350-362.
- World Allergy Organization: IgE in Clinical Allergy and Allergy Diagnosis.
- Morgan WJ, Crain EF, et al. Results of a Home-Based Environmental Intervention among Urban Children with Asthma. N Engl J Med 2004; 351:1068-1080