Respiratory Health
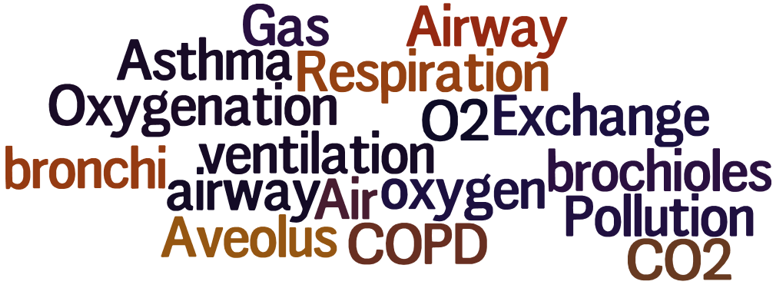
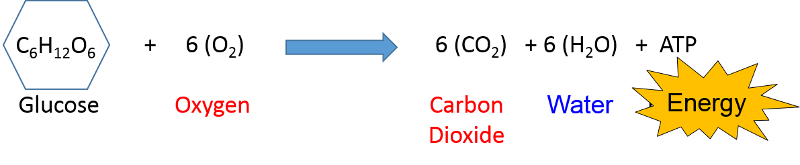
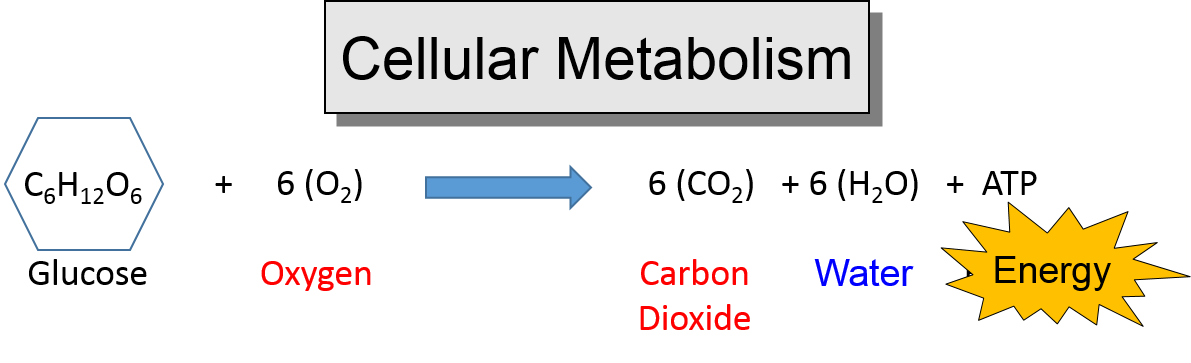
The equation below illustrates how nutrients (e.g., glucose) are converted to cellular energy in the form of adenosine triphosphate (ATP). All animals need oxygen to metabolize nutrients to generate cellular energy. Note also that carbon dioxide is produced as a by-product of metabolism.
As a result, humans and other animal species continually need to be able to take in oxygen from the environment and distribute to all tissues, and the carbon dioxide that is generated needs to be excreted. The lungs are the interface between our blood stream and the external environment and the site where oxygen (O2) is taken up and carbon dioxide (CO2) leaves the bloodstream and is expelled to the environment. The intimacy of this interface between our internal and external environment and the continual need to exchange air with the environment has a major impact on health for several reasons. First, continual exposure of the respiratory tract to air from the environment provides an important portal for entry of viruses and bacteria that can cause infection. Second, disease processes that impede the mechanics of ventilation (e.g., emphysema and asthma) can cause severe illness or death; these processes are triggered or exacerbated by substance in the air we breath. Finally, air is a variable and complex mixture of many substances, including particulate matter and chemicals that can have a detrimental effect on lung function; moreover, many of these chemicals can be absorbed into circulating blood and cause a wide range of health problems throughout the body.
After successfully completing this section, the student will be able to:

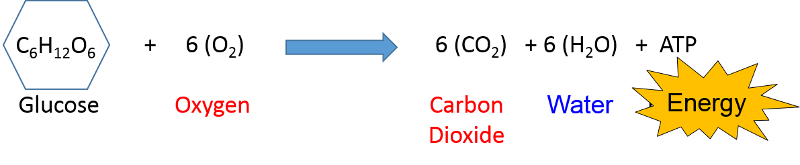
Respiration continually brings air from the environment in contact with the delicate cells in our lungs to provide oxygen and to expel carbon dioxide, which is a by product of metabolism. Nevertheless, inspired air can also carry chemical and particulate contaminants which can be harmful, and several mechanisms have evolved to mitigate the effects of these contaminants. Nasal hairs and mucus can trap dust and other particulate matter.
Stem cells in the respiratory epithelium give rise to progenitor cells that differentiate into several cell types whose function is critical to respiration. Clara cells are complex cells whose structure and function changes depending on circumstances. They can differentiate into mucus-secreting "goblet" cells; a mucus layer on the epithelial cell surfaces protects the cells and traps dust and other foreign material. Clara cells can also differentiate into ciliated cells which have hair-like projects that move rhythmically and sweep mucus and trapped particles upwards where it can be either swallowed or expectorated.
Source: Adapted from http://www.influenzareport.com/ir/pathogen.htm
The brief video below illustrates the functions of these cells.
The YouTube video below (3:09) illustrates oxygen transport from the lungs to cells throughout the body.
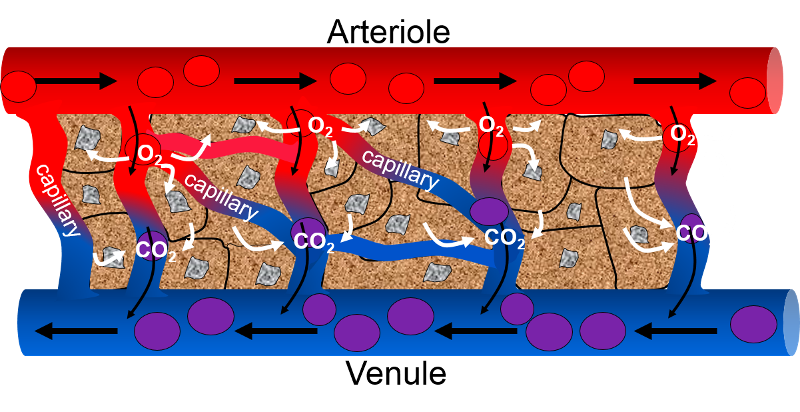
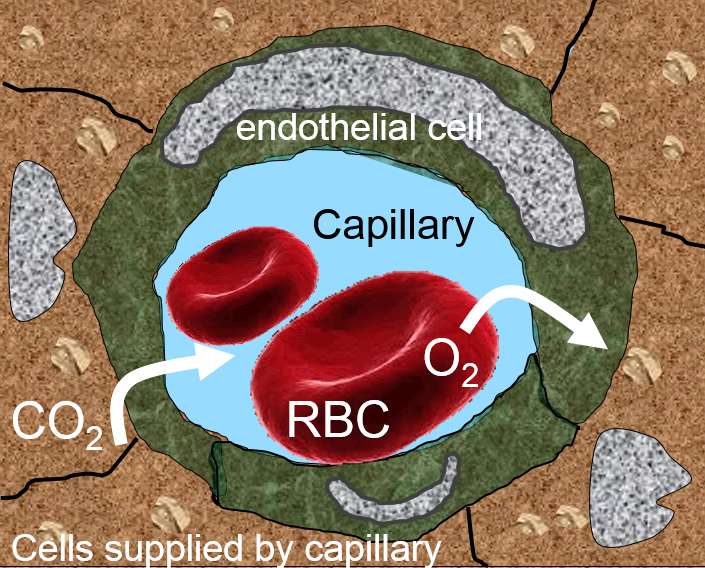
Oxygen is necessary for cells to be able to generate cellular energy from glucose or fatty acids. After blood is reoxygenated in the lungs, it leaves the left ventricle of the heart and is distributed throughout the body in increasingly branched blood vessels. Arteries branch into arterioles, which, in turn, eventually branch into capillaries. The image below on the left shows an arteriole branching into smaller capillaries which supply nutrients and oxygenated red blood cells (RBCs) to metabolizing cells (shown in stippled brown). As RBCs pass through the capillaries and release oxygen to the cells, they become progressively deoxygenated (purple RBCs). At the same time, carbon dioxide and other wastes are transferred into capillary blood for excretion. Capillary blood then enters venules to be returned to the heart and lungs, where CO2 is exhaled and blood becomes reoxygenated.The image on the right shows a capillary that has been cut in cross-section. The lumen (interior) of the capillary is shown in blue with a single RBC, since capillaries are so fine that RBCs often pass through them one at a time. The endothelial cells lining the capillary are shown in green, and the metabolizing cells receiving oxygen and nutrients from the capillary are shown in stippled brown.
This video (56 sec.) illustrates how CO2 is transported from tissues to the lungs.
Tobacco smoke is a complex mixture of toxic and carcinogenic chemicals and particulate matter. A review article by Talhout et al. (Int J Environ Res Public Health. Feb 2011; 8(2): 613–628.) concluded that emission levels of 98 components in mainstream smoke constituted a human inhalation risk with the potential to contribute to the many established adverse health effects associated with smoking.
The CDC web page on Health Effects of Cigarette Smoking states that
Table - Premature Deaths Caused by Smoking and Exposure to Secondhand Smoke from 1965 to 2014
|
Cause of Death |
Total Number |
|---|---|
|
Smoking-related cancers |
6,587,000 |
|
Cardiovascular and metabolic diseases |
7,787,000 |
|
Pulmonary disease |
3,804,000 |
|
Conditions related to pregnancy and birth |
108,000 |
|
Residential fires |
86,000 |
|
Lung cancers from exposure to secondhand smoke |
263,000 |
|
Coronary heart disease from secondhand smoke |
2,194,000 |
|
TOTAL |
20,830,000 |
Source: CDC, National Center for Chroic Disease Prevention and Health Promotion, Office on Smoking and Health.
Modified from the Executive Summary of The Health Consequences of Smoking - 50 Years of Progress:
A Report of the Surgeon General, U.S. Department of Health and Human Services, 2014
Regular smoking has the following effects:
Tobacco smoke contains a number of established carcinogens, and smoking is associated with an increased risk of cancer throughout the body, including:
Smoking can cause cancer almost anywhere in your body:
For more information on the causes of cancer, see the online learning module on The Biology of Cancer. Page 5 of the module focuses specifically on the evolution of lung cancer.
Smoking decreases fertility in women and men, and women who smoke during pregnancy have an increased risk of the following::
Postmenopausal women who smoke have lower bone density and increased risk of hip fracture compared to women who never smoked.
Effects of Active Smoking
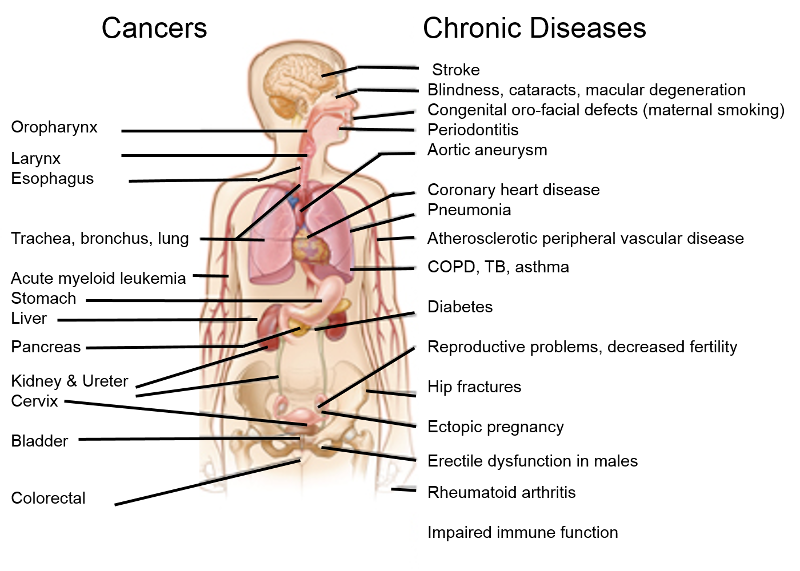
Adapted from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/
Effects of Environmental Tobacco Smoke
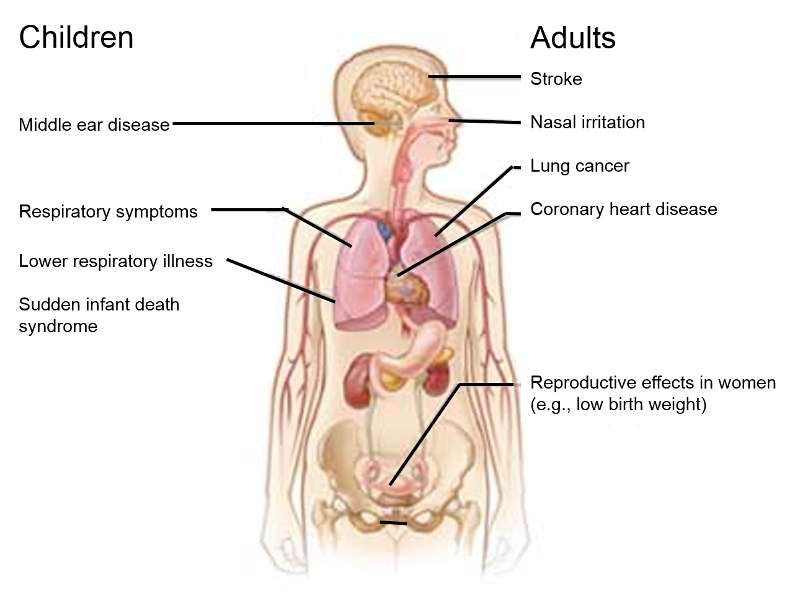
Adapted from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/
Link to more information: The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General, 2014.
Chronic obstructive pulmonary disease (COPD) is a global health problem that affects millions of people and is an important cause of morbidity, mortality, and extensive utilization of health care resources. COPD is one of the top ten causes of death worldwide, and the direct costs of treating COPD in the United States alone are estimated to be around $30 billion per year. COPD actually represents a spectrum of disease ranging from destruction of the alveoli and thickening of the terminal airways on one extreme (emphysema) to thickening of the airways with chronic inflammation and repeated bouts of infection (chronic bronchitis) on the other extreme. Most frequently there are elements of both of these clinical pictures.
The likelihood of COPD is heavily influenced by both environmental/behavior risk factors and by hereditary factors. In most cases, COPD is caused by chronic inhalation of harmful particles and gases (e.g., in tobacco smoke), which triggers pathophysiologic changes in the small airways, in the alveoli, and in blood vessels in the lung. All smokers have inflammation in their lungs and airways, and they all have thickening of the airways, damage to ciliated cells, and hypersecretion of mucus. Immune fun
In addition, the normal processes for breakdown and repair of cellular elements and immune defense are impaired. These abnormalities produce a spectrum of largely irreversible changes ranging from mucous hypersecretion (chronic bronchitis), to chronic small airway inflammation and fibrosis (bronchiolitis), and outright tissue destruction and impaired airflow (emphysema).
One of the hallmarks of COPD is reduced airflow, which occurs as the result of one or more of the following:
The clinical manifestations of COPD are labored breathing and shortness of breath, cough, hypoxemia, and excessive mucous production. Once the fundamental changes of COPD, they are irreversible, but individuals with COPD will intermittently experience acute exacerbations during episodes of lung infection. These episodes can be treated, but the underlying pathology remains unchanged.

Adapted from http://www.nature.com/nature/journal/v489/n7417_supp/full/489S2a.htm
Spirometry is a method of measuring changes in airflow during inspiration and expiration, and it provides a sensitive way of identifying abnormalities in ventilatory function.The first image below on the left shows a subject breathing through a tube connected to a spirometer, which measures changes in air flow. The graph on the right shows normal changes in lung volume over time during inspiration and expiration, both at rest and during forced inspiration and expiration. Move your cursor over the lines of the graph to get a more detailed explanation.
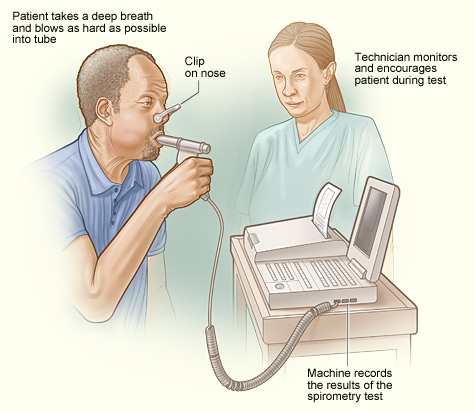
Image source: http://www.nhlbi.nih.gov/health/health-topics/topics/copd/diagnosis.html
Spirometry is abnormal in people with COPD. The graph below on the right shows that the obstructive changes in COPD reduce the ability to expire air, and this results in an increased residual volume. As a result, the ability to move air in and out of the lungs is progressively impaired, ultimately leading to diminished oxygenation of blood. Move your cursor over the phases of the line graph for a more complete explanation.
The graph below on the left from Fletcher and Peto shows the natural history of changes in FEV1 in non-smokers, smokers, and smokers who quit smoking. Note that decreases in FEV1 lead to symptoms, disability, and death.
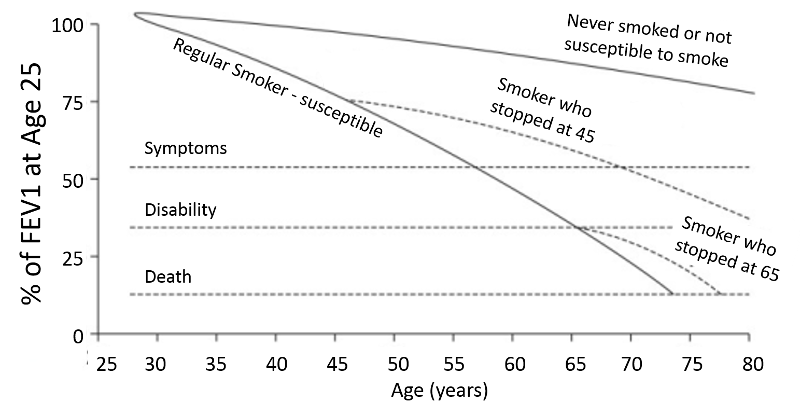
Modified from Fletcher C. and Peto R.: The natural history of chronic airflow obstruction. Br Med J. 1977;1(6077):1645–1648.
,
Table - Frequency and Activity of Several Known Genotypes for Alpha-1 Antitrypsin
|
Genotype |
Fraction of Population |
Activity (% of normal MM genotype) |
|---|---|---|
|
MM |
0.90 |
100% |
|
MZ |
0.038 |
60% |
|
SS |
0.001 |
55% |
|
SZ |
0.0012 |
33% |
|
ZZ |
0.0004 |
12% |

Adapted from Larsson C. Acta Med. Scand. 1978;204:345-351
COPD is a chronic progressive disease, and, eventually the pathophysiologic changes in the lung lead to chronic inflammation, destruction of alveoli, impaired ventilation (air trapping), and hypoxemia with progressive disability frequently leading to premature death.. The patient in the photograph below illustrates the clinical features of end-stage COPD. Notice that he is wearing a nasal c annula that is providing supplemental oxygen. He is thin due to muscle wasting, which is characteristic of end stage COPD, but he is "barrel-chested" due to chronic air trapping. Because of the airway obstruction and difficulty in moving air, he is hunched forward with his hands on his knees in order to enable him to use his accessory muscles of respiration, i.e., muscles in his neck and shoulders and chest wall. Note also that he is pursing his lips; this enables him to increase airway pressure during expiration in order to prevent from airway collapse. The insert at the upper left side of the photo shows a blackened lung that was removed from a chronic smoker.

Image sources: http://meded.ucsd.edu/clinicalmed/lung.htm (patient) and http://www.myvmc.com/diseases/emphysema (lung)
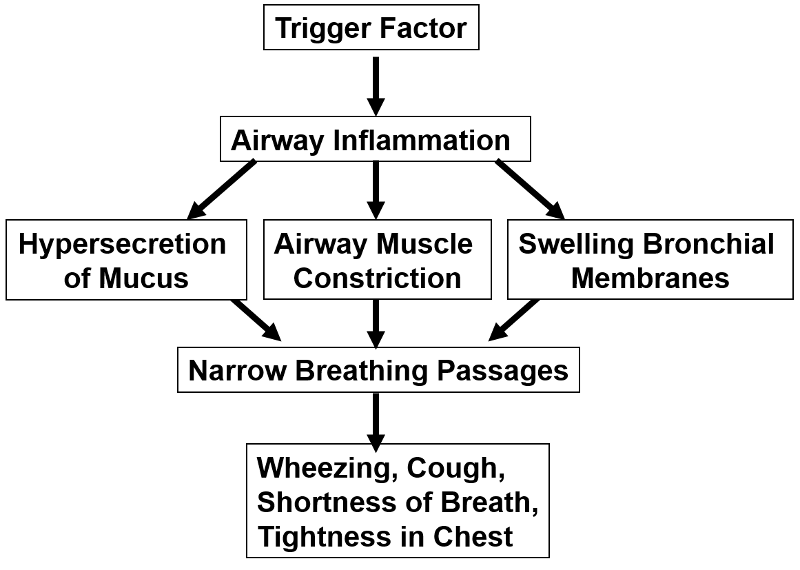
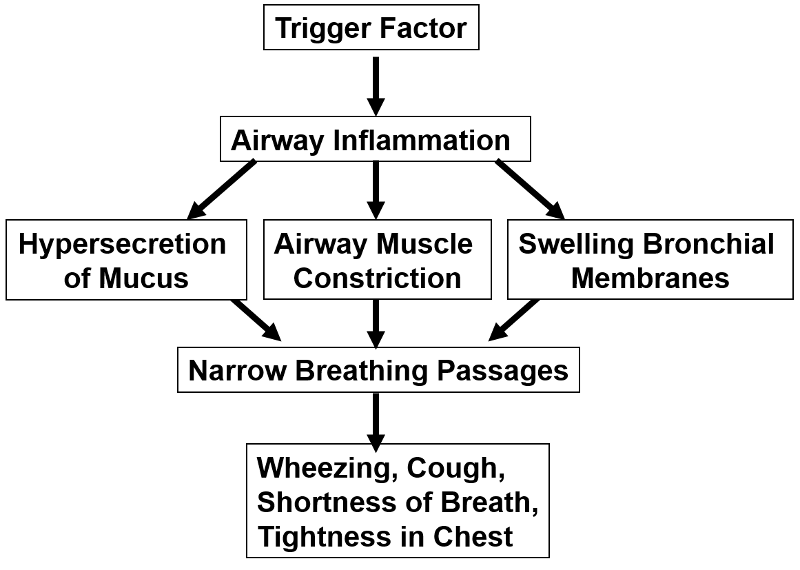
Asthma is a common, chronic syndrome characterized by intermittent episodes of symptoms, which can be severe and life-threatening. The clinical episodes are triggered by antigens, viruses, exercise, or inhalation of irritating substances. Any of these stimuli can trigger a hyperactive allergic response which produces:
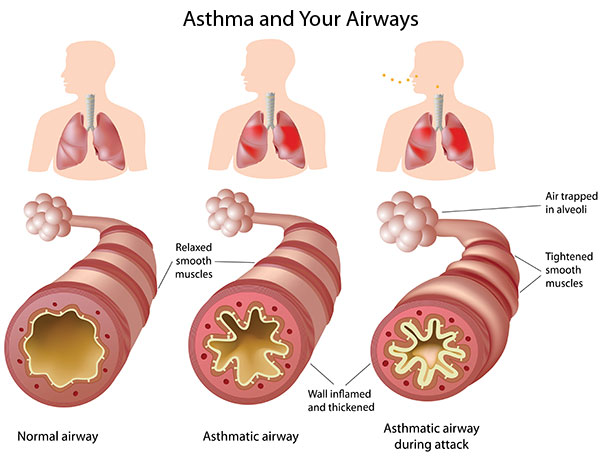
Source: Image source: http://www.nlm.nih.gov/medlineplus/magazine/issues/fall11/articles/fall11pg4.html
These, in turn, cause varying degrees of airflow obstruction, causing shortness of breath, wheezing, cough, tightness in the chest, and sometimes severe "air hunger" and panic. The episodes can resolve spontaneously, but they can be severe, unrelenting and fatal if not treated. The audio files below give an indication breath sounds during auscultation with a stethoscope in a normal person and in a person having an acute asthma attack.
Normal breath sounds
Breath sounds during an asthma attack
The CDC estimates that approximately 20 million Americans have asthma. Asthma is more common in children than in adults, more common in women compared with men, and more common in blacks than in whites. The mortality from asthma rose in the 1980s, but then plateaued, and mortality rates have declined since 1999, probably due to improved treatment.
The pathophysiologic basis of asthma is not well understood. It appears to have a complex, multifactorial etiology which results from an interplay of many hereditary factors and a number of environmental factors. Bronchial biopsies from patients with even mild asthma have evidence of chronic inflammation, and cytokines and other mediators of inflammation are found in bronchial washings from asthma patients. Some families are more prone to development of allergies, and there is a well-known association between allergies and asthma. This suggests a genetic predisposition, but it appears that a number of genes are involved. Allergic reactions are mediated by antibodies of the IgE class. People who are prone to IgE-mediated allergic reactions are said to be "atopic meaning that they have a genetic predisposition to make IgE antibodies in response to certain allergens. While allergic reactions are mediated by IgE antibodies, T and B lymphocytes play an important role in the production of IgE. There are two types of T helper cells (Th lymphocytes) designated Th1 and Th2. Th1 cells tend to promote cell-mediated immune responses by producing interferon-gamma, interleukin-2 (IL-2), and TNF-β. In contrast, Th2 cells promote the production of IgE antibodies by producing IL-4 and IL-13, which are interleukins that act B lymphocytes (B cells) to promote the production of IgE antibodies to a specific antigen. People who are prone to develop allergies, i.e., atopic people, are believed to have a higher ratio of Th2/Th1 cells, and this is believed to be an important factor in their tendency to produce allergy-mediating IgE antibodies. These observations are clearly relevant to asthma, since biopsies of the bronchial mucosa of patients with asthma have an excess of activated Th2 cells. Many authors take these observations to indicate that an imbalance in Th2/Th1 plays an important role in the development of allergies and, specifically, of asthma.
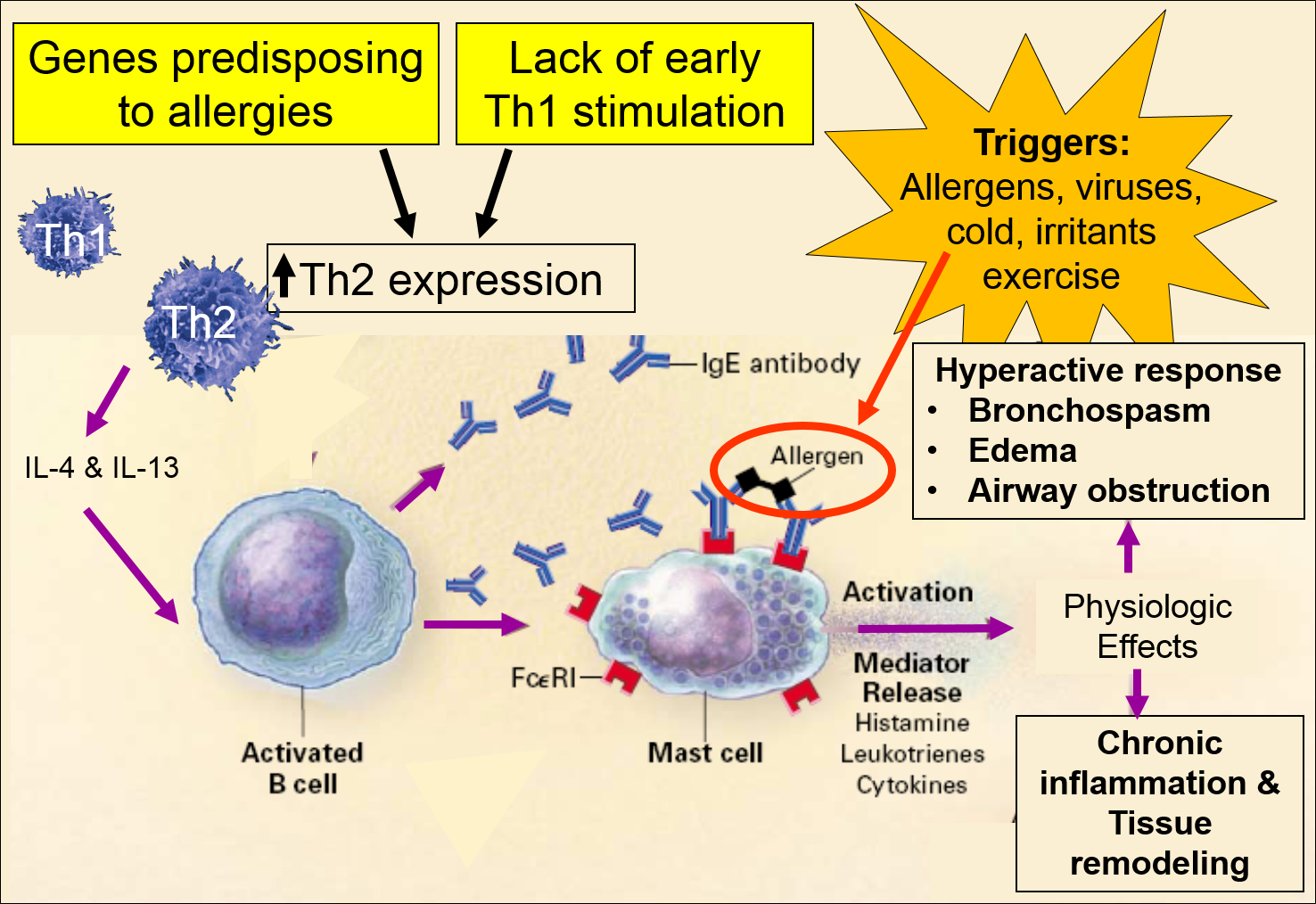
Image adapted from: Busse W. & Lemanske R: N. Engl. J. Med. 2001;344(5):350-362
Genetic factors clearly play a role in predisposing to allergic reactions, but there is also evidence to suggest that environmental exposures in utero and in early infancy also play a role. This is supported by the increasing prevalence of asthma in industrialized parts of Western countries and an increased prevalence in urban environments compared to rural settings. Epidemiologic studies indicate that certain exposures in early life are associated with stimulation of Th1 mediated responses and a decreased risk of developing asthma and other allergic disorders. These include:
In contrast, widespread use of antibiotics may increase the risk of allergies by impairing the development Th2-mediated responses. Newborn infants generally have a preponderance of Th2 cells, and it may be that early exposure to antigens from certain infectious agents may be critical to promoting an appropriate balance between Th2 and Th1 mediated responses. As a result, the combination of genetic predisposition and understimulation of Th1-immune responses may set the stage for later development of allergies and, specifically, asthma.
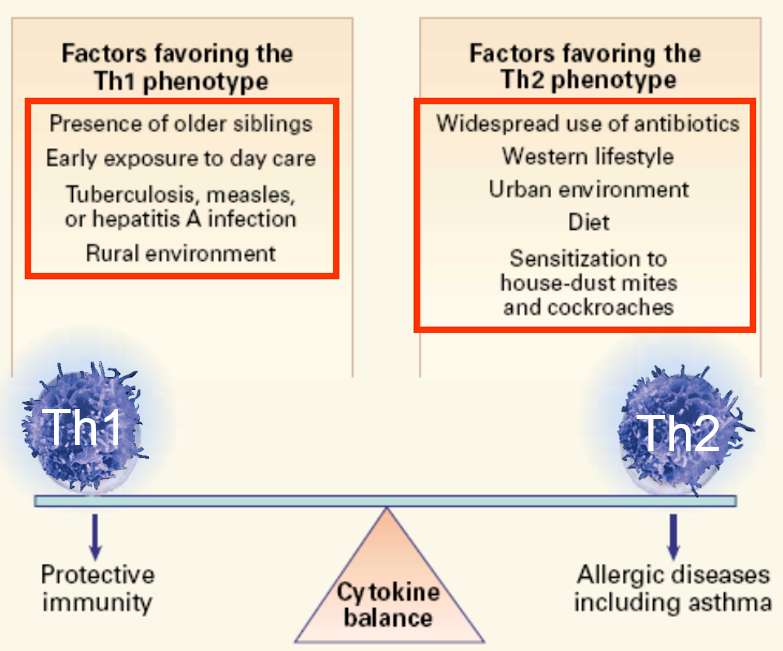
Image adapted from: Busse W. & Lemanske R: N. Engl. J. Med. 2001;344(5):350-362
Hereditary factors and failure to stimulate Th1 immune response set the stage for allergies, and the final phase is sensitization to one or more allergens, which then act as the triggers for acute allergic or asthmatic reactions. The initial exposure to an antigen evokes a primary immune response. For example, when an allergen like pollen is inhaled, it is phagocytized by dendritic cells in the epithelium. After internalization, the dendritic cell breaks down the components and "presents" the antigen fragments on their cell surface where they can activate specific T lymphocytes with receptors that bind to specific epitopes on the fragment. Th2 lymphocytes activate B-lymphocytes which then transform into plasma cells that manufacture IgE antibodies specific for the particular antigen. The IgE-antibodies enter the circulation for distribution. One portion of the IgE antibody binds to receptors on mast cells, but another portion of the IgE remains available to bind to the allergen. If the allergen binds to the IgE on the mast cell, the mast cell becomes activated to release histamine, leukotrienes, and other cytokines. Subsequent exposures to the antigen result in a secondary immune response (memory response) which is much more rapid and vigorous than the primary immune response. Allergen-specific IgE is rapidly produced, and mast cells degranulate and release an array of inflammatory mediators which cause edema, hypersecretion of mucus, and bronchoconstriction by caused contraction of smooth muscle cells surrounding the airways. In addition to episodic acute asthmatic attacks, asthmatics also have remodeling of the the airways which results in thickening and chronic presence of increased numbers of inflammatory cells and mediators.
While the pathophysiologic basis of asthma is far from complete, this discussion attempts to summarize the basic aspects of our current understanding.
The medical management of asthma and treatment of acute attacks has improved substantially, but the prevalence of asthma continues to rise in urban settings in industrialized Western countries. There is still controversy about the hygiene hypothesis, and it is not yet clear that early exposure to certain antigens could be exploited as a preventive measure. Given what is known about asthma, avoidance of asthma trigger factors would be expected to at least reduce the frequency and severity of symptoms. EPA recommendations for an "Asthma Friendly House" are shown in the iFrame below.
EPA Recommendations Asthma Friendly House
For additional measures, also see the EPA Home Environment Checklist.
There is some evidence that interventions to reduce dust, animal dander, mold, and exposure to cockroaches are effective, but the literature indicates that allergen reduction is difficult to achieve and the effectiveness is not as great as expected. The four articles cited below (one randomized clinical trial and three systematic reviews of the literature) suggest that environmental remediation interventions that target one or two potential targets are of limited, if any value. However, they suggest that multifaceted interventions can reduce symptoms, school absences, and hospital visits for acute asthma care.
Link to Paper #1 - Morgan WJ, Crain EF, et al. Results of a Home-Based Environmental Intervention among Urban Children with Asthma. N Engl J Med 2004; 351:1068-1080
From the Abstract:
"We enrolled 937 children with atopic asthma (age, 5 to 11 years) in seven major U.S. cities in a randomized, controlled trial of an environmental intervention that lasted one year (intervention year) and included education and remediation for exposure to both allergens and environmental tobacco smoke. Home environmental exposures were assessed every six months, and asthma-related complications were assessed every two months during the intervention and for one year after the intervention.
Results
For every 2-week period, the intervention group had fewer days with symptoms than did the control group both during the intervention year (3.39 vs. 4.20 days, P<0.001) and the year afterward (2.62 vs. 3.21 days, P<0.001), as well as greater declines in the levels of allergens at home, such as Dermatophagoides farinae (Der f1) allergen in the bed (P<0.001) and on the bedroom floor (P=0.004), D. pteronyssinus in the bed (P=0.007), and cockroach allergen on the bedroom floor (P<0.001). Reductions in the levels of cockroach allergen and dust-mite allergen (Der f1) on the bedroom floor were significantly correlated with reduced complications of asthma (P<0.001)."
Link to Paper #2 - Gøtzsche PC, Johansen HK: Does controlling exposure to house dust mites improve asthma? Cochrane Collaborative Review. 5 Oct. 2011
Summary:
"Asthma is a chronic inflammatory disease of the airways. The prevalence of asthma has increased and it is now the commonest chronic disease among children. Asthma is triggered by allergens (substances that cause an allergic reaction) and house dust presents a problem in some people with asthma. The major allergen in house dust comes from mites and it is hypothesized that controlling exposure to house dust mites will reduce asthma symptoms in people who are sensitive to house dust mites.
We included 55 randomized trials on 3121 people with asthma. There are both chemical (10 trials) and physical methods such as mattress encasings (37 trials) of reducing mite allergen levels and we included both types in this review. There were also eight trials that used both physical and chemical methods. Many trials were of poor quality and would therefore be expected to exaggerate the reported effect, but we did not find an effect of the interventions. There was no difference in peak flow (a measure of lung function), asthma symptoms and medication scores, or the number of patients reporting an improvement in their asthma symptoms.
While reducing exposure to house dust mites is recommended in guidelines, we did not find an effect of control measures to reduce the exposure to mites or their products." .
Link to Paper #3 - Crocker DD, Kinyota S, et al:Task Force on Community Preventive Services. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011;(2 Suppl 1):S5-32.
From the Abstract:
"Evidence synthesis
In the 20 studies targeting children and adolescents, the number of days with asthma symptoms (symptom-days) was reduced by 0.8 days per 2 weeks, which is equivalent to 21.0 symptom-days per year (range of values: reduction of 0.6 to 2.3 days per year); school days missed were reduced by 12.3 days per year (range of values: reduction of 3.4 to 31.2 days per year); and the number of asthma acute care visits were reduced by 0.57 visits per year (interquartile interval: reduction of 0.33 to 1.71 visits per year). Only three studies reported outcomes among adults with asthma, finding inconsistent results.
Conclusions
Home-based, multi-trigger, multicomponent interventions with an environmental focus are effective in improving overall quality of life and productivity in children and adolescents with asthma. The effectiveness of these interventions in adults is inconclusive due to the small number of studies and inconsistent results. Additional studies are needed to (1) evaluate the effectiveness of these interventions in adults and (2) determine the individual contributions of the various intervention components."
Link to Paper #4 - Mims JW and Biddy AC: Efficacy of environmental controls for inhalant allergies. Current Opinion in Otolaryngology & Head & Neck Surgery. 2013;21(3):241-247.
Summary
"Although many studies evaluating a single environmental control strategy fail to show an improvement in clinical outcomes, comprehensive environmental controls may provide some benefit. Additionally, studies that relocate patients to low allergen environments tend to demonstrate clinical improvement."
re of gases and a variety of naturally occurring and made-made particles and contaminants. The gases in air are:
Air pollutants are the particles, vapors, and contaminants not found in pure air. Pollutants can be naturally occurring or the result of human activity (anthropogenic).
|
Naturally Occurring Pollution |
Man-made Pollution |
|---|---|
|
|
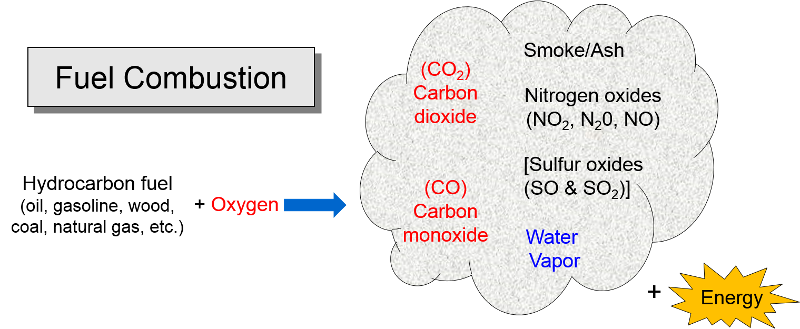
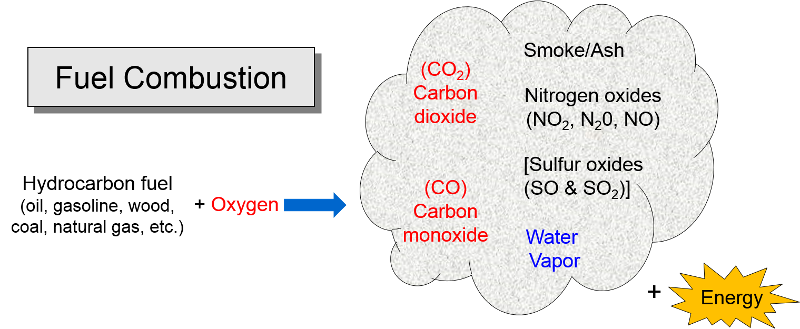
Air pollution is primarily the result of burning hydrocarbon fuels and releasing the by-products into the atmosphere. At the beginning of this module it was noted that cellular metabolism involves the oxidation of glucose or fat (hydrocarbon compounds) in order to release energy in the form of ATP that can be used for a variety of cellular processes that require energy.
The energy that humans require for heat, electricity, automobiles, industry etc. is mostly derived by combustion of hydrocarbon fuels. Combustion also involves oxygen combining with hydrocarbonsl (gasoline, oil, coal, propane, natural gas, wood, diesel fuel, etc.) to produce energy. The by-products are carbon dioxide (CO2), carbon monoxide (CO), water vapor, smoke, and ash (particulate residue). Carbon monoxide (CO) tends to be formed when there is insufficient oxygen for the hydrocarbon to be oxidized (burned) completely. Nitrogen is the most abundant gas in the air we breath, and it too combines with oxygen during combustion to form a series of compounds called nitrogen oxides (NO2, N20, NO); these are sometimes collectively referred to as "NOx." Sulfur dioxide (SO2) is also formed during combustion of sulfur-containing fuels such as coal or unrefined oil. Combustion of hydrocarbon fuels also produces "particulates", some of which are visible as smoke and some are so small that they are invisible. As we will see, these by-products of combustion pose threats to health and to the environment.
Other pollutants can also be released by combustion, depending on the combustion of what is being burned. Sulfur dioxide is present in coal and crude oil, but sulfur is removed when oil is refined to produce gasoline, so coal is the primary source of SO2.

Source: National Geographic
http://environment.nationalgeographic.com/environment/global-warming/pollution-overview/
Coal also contains small concentrations of elemental mercury which vaporizes when coal is burned. The vapors can remain in the atmosphere for some time and travel with wind currents until the mercury eventually returns to earth during precipitation. Some bacteria are able to convert elemental mercury into methylmercury, an organic form which can be taken up by algae. Methylmercury then moves up through the food chain from algae to zooplankton and then to fish of increasing size. Through this process of bioaccumulation and biomagnification mercury can be found in the high concentrations large saltwater such as tuna and swordfish. Fetuses, infants and small children exposed to methylmercury can have severely impaired neurological development. For more information see the EPA web page on health effects of mercury.
Lead is another toxic heavy metal that enter the atmosphere during combustion of materials in which it is present. In the 1920s gasoline producers began adding lead in order to reduce "engine knock". The combustion of gasoline in vehicles using leaded gas produced high levels of lead in the atmosphere. As the health hazards of lead became increasingly apparent, the use of lead additives declined, and they were banned in the US in 1995. Most other countries have subsequently banned lead additives. At present industrial sources (e.g. smelters, battery manufacture, metal processing) are responsible for the majority of lead in the atmosphere. Lead is also neurotoxic and can cause a spectrum of problems ranging from subtle impairments in development to severe impairments in nerve function, learning, and hearing. It can also cause anemia and, in severe cases death. For more information see the EPA web page on health effects of lead.
VOCs are organic compounds (i.e., hydrocarbons) that evaporate readily at room temperature and enter the atmosphere. VOCs are in present gasoline and other fuels and in many industrial and household products, such as organic solvents, cleaning supplies, paint, lacquer, varnish, paint strippers, cleaning supplies, pesticides, building materials, copiers and printers. VOCs are important participants in the generation of ozone, which is a secondary pollutant which is discussed below in the section on Criteria Pollutants.
PAHs represent a large family of molecules that can be naturally occurring, but they are also produced when coal, oil, gas, and garbage are burned incompletely. PAHs can also be generated by cooking meats at high temperatures. One can be exposed to PAHs in the air, or they can be ingested in contaminated food or water, and also by direct contact with PAH-contaminated soil or products like heavy oils, coal tar, roofing tar, or creosote. PAHs cause tumors and birth defects in rodents exposed to PAHs through food inspired inspired air, or direct contact with skin.
Examples of PAHs
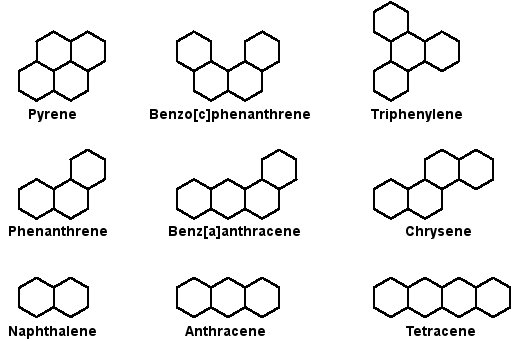
Image source: http://www.astrochem.org/sci/Cosmic_Complexity_PAHs.php
In the video clip below (<3 min.), Dr. David Sherr, from the environmental health department at BUSPH, discusses the potential role of environmental pollutants as risk factors for breast (and other) cancers. Dr. Sherr's research is exploring the molecular mechanisms that initiate and maintain breast cancer. Much of his research has focused on the role of an environmental chemical receptor (the aryl hydrocarbon receptor - AhR) and the role of polycyclic aromatic hydrocarbons (PAHs), which are atmospheric pollutants generated by burning fuel and by cooking meat at high temperatures (e.g., grilling). PAHs are also found in smoked fish. In this video, Dr. Sherr also discusses the difficulties in establishing a causal link between environmental pollutants and cancer.
From the EPA (http://www.epa.gov/airquality/urbanair/):
"The Clean Air Act requires EPA to set National Ambient Air Quality Standards for six common air pollutants. These commonly found air pollutants (also known as "criteria pollutants") are found all over the United States. They are particle pollution (often referred to as particulate matter), ground-level ozone, carbon monoxide, sulfur oxides, nitrogen oxides, and lead. These pollutants can harm your health and the environment, and cause property damage. Of the six pollutants, particle pollution and ground-level ozone are the most widespread health threats. EPA calls these pollutants "criteria" air pollutants because it regulates them by developing human health-based and/or environmentally-based criteria (science-based guidelines) for setting permissible levels. The set of limits based on human health is called primary standards. Another set of limits intended to prevent environmental and property damage is called secondary standards.
Click on one of the pollutants below for information on sources of the pollutant, why the pollutant is of concern, health and environmental effects, efforts underway to help reduce the pollutant, and other helpful resources."
|
Sources of Air Pollution Data from http://www.epa.gov/air/emissions/index.htm |
Health Effects of Criteria Pollutants From http://www.epa.gov/region7/air/quality/health.htm |
Pollutant Concentrations Over Time Data from http://www.epa.gov/airtrends/index.html |
|
|
Carbon Dioxide "Carbon monoxide is a colorless odorless poisonous gas formed when carbon in fuels is not burned completely. It is a byproduct of motor vehicle exhaust, which contributes more than two-thirds of all CO emissions nationwide. In cities, automobile exhaust can cause as much as 95 percent of all CO emissions."
"Carbon monoxide enters the bloodstream and reduces oxygen delivery to the body's organs and tissues. The health threat from CO is most serious for those who suffer from cardiovascular disease. Healthy individuals are also affected, but only at higher levels of exposure. Exposure to elevated CO levels is associated with visual impairment, reduced work capacity, reduced manual dexterity, poor learning ability, and difficulty in performing complex tasks."
NOTE: High concentrations, e.g., from a car running in an unvented garage or from poorly vented kerosene heaters, can be fatal.
See also CO in Smokers. |
|
|
|
Lead "Exposure to lead mainly occurs through inhalation of air and ingestion of lead in food, paint, water, soil, or dust. Lead accumulates in the body in blood, bone, and soft tissue. Because it is not readily excreted, lead can also affect the kidneys, liver, nervous system, and other organs. Excessive exposure to lead may cause anemia, kidney disease, reproductive disorders, and neurological impairments such as seizures, mental retardation, and/or behavioral disorders. Even at low doses, lead exposure is associated with changes in fundamental enzymatic, energy transfer, and other processes in the body. Fetuses and children are especially susceptible to low doses of lead, often suffering central nervous system damage or slowed growth. Recent studies show that lead may be a factor in high blood pressure and subsequent heart disease in middle-aged white males. Lead may also contribute to osteoporosis in postmenopausal women."
After banning lead additives in gasoline, the primary source of lead in the has become smelters and battery plants. The highest concentrations of lead are found in the vicinity of nonferrous smelters and other stationary sources of lead emissions.
|
|
|
|
Nitrogen Oxides Nitrogen oxides form when fuel is burned at high temperatures and come principally from motor vehicle exhaust and stationary sources such as electric utilities and industrial boilers. A suffocating, brownish gas, nitrogen dioxide is a strong oxidizing agent that reacts in the air to form corrosive nitric acid, as well as toxic organic nitrates. It also plays a major role in the atmospheric reactions that produce ground-level ozone (or smog).
Health and Other Effects: Nitrogen dioxide can irritate the lungs and lower resistance to respiratory infections such as influenza. The effects of short-term exposure are still unclear, but continued or frequent exposure to concentrations that are typically much higher than those normally found in the ambient air may cause increased incidence of acute respiratory illness in children. EPA's health-based national air quality standard for NO2 is 0.053 ppm (measured as an annual average). Nitrogen oxides are important in forming ozone and may affect both terrestrial and aquatic ecosystems. Nitrogen oxides in the air are a potentially significant contributor to a number of environmental effects such as acid rain and eutrophication in coastal waters like the Chesapeake Bay. Eutrophication occurs when a body of water suffers an increase in nutrients that reduce the amount of oxygen in the water, producing an environment that is destructive to fish and other animal life."
|
|
|
|
Particulate Matter (PM2.5 and PM10) "Particulate matter is the term for solid or liquid particles found in the air. Some particles are large or dark enough to be seen as soot or smoke. Others are so small they can be detected only with an electron microscope. Because particles originate from a variety of mobile and stationary sources (diesel trucks, wood stoves, power plants, etc.), their chemical and physical compositions vary widely."
Particles less than 10 microns (micrometers) in diameter can be inhaled, and these are divided into PM-10 and PM2.5. PM-10 includes particles with a diameter of 10 microns or less; these tend to be generated by wind or mechanical agitation from plowing, grinding, etc. Particles between 2.5-10 microns tend to adhere to the mucus in the trachea and bronchi; they are then gradually swept up to the pharynx by the cilia on epithelial cells lining the respiratory tract. Once they reach the pharynx, they can be swallowed or expectorated.
PM-2.5 particles with a diameter of 2.5 microns or less, often referred to as "fine particulates", are mostly generated from combustion. Ultrafine particles, <0.1 microns, are generated from diesel engines, particularly when they are idling. Particles <2.5 microns are able to reach the lower respiratory tract and alveoli because they are small and light and can be carried easily with the inspired air.
Health Effects: "Major concerns for human health from exposure to particulate matter are: effects on breathing and respiratory systems, damage to lung tissue, cancer, and premature death. The elderly, children, and people with chronic lung disease, influenza, or asthma, tend to be especially sensitive to the effects of particulate matter. Acidic particulate matter can also damage manmade materials and is a major cause of reduced visibility in many parts of the U.S. Click here for more information on the health effects of particulate matter."
|
|
|
|
Sulfur Oxides "These gases are formed when fuel containing sulfur (mainly coal and oil) is burned, and during metal smelting and other industrial processes.
Health and Other Effects: The major health concerns associated with exposure to high concentrations of SO2 include effects on breathing, respiratory illness, alterations in pulmonary defenses, and aggravation of existing cardiovascular disease. Major subgroups of the population that are most sensitive to SO2 include asthmatics and individuals with cardiovascular disease or chronic lung disease (such as bronchitis or emphysema) as well as children and the elderly. EPA's health-based national air quality standard for SO2 is 0.03 ppm (measured on an annual average) and 0.14 ppm (measured over 24 hours). Emissions of SO2 also can damage the foliage of trees and agricultural crops. EPA has a secondary SO2 national ambient air quality standard of 0.50 ppm (measured over 3 hours) designed to prevent this type of environmental deterioration. Together, SO2 and NOX are the major precursors to acid rain, which is associated with the acidification of lakes and streams, accelerated corrosion of buildings and monuments, and reduced visibility."
|
|
|
|
Volatile Organic Compounds "Unlike other pollutants, ozone is not emitted directly into the air by specific sources. Ozone is created by sunlight acting on nitrogen oxides (NOx) and volatile organic compound (VOC) emissions in the air. There are literally thousands of sources of these gases. Some of the more common sources include gasoline vapors, chemical solvents, combustion products of various fuels, and consumer products. They can originate from large industrial facilities, gas stations, and small businesses such as bakeries and dry cleaners. Often these "precursor" gases are emitted in one area, but the actual chemical reactions, stimulated by sunlight and temperature, take place in another. Combined emissions from motor vehicles and stationary sources can be carried hundreds of miles from their origins, forming high ozone concentrations over very large regions. Health and Other Effects: Scientific evidence indicates that ground-level ozone not only affects people with impaired respiratory systems (such as asthmatics), but healthy adults and children as well. Exposure to ozone for 6 to 7 hours, even at relatively low concentrations, significantly reduces lung function and induces respiratory inflammation in normal, healthy people during periods of moderate exercise. It can be accompanied by symptoms such as chest pain, coughing, nausea, and pulmonary congestion. Recent studies provide evidence of an association between elevated ozone levels and increases in hospital admissions for respiratory problems in several U.S. cities. Results from animal studies indicate that repeated exposure to high levels of ozone for several months or more can produce permanent structural damage in the lungs. |
|
|
Ozone Formation The naturally occurring ozone in the stratosphere protects the earth from the damaging effects of ultraviolet radiation from the sun. However, so called ground level ozone that forms as a result of man-made pollution, is harmful to health. Ozone is produced in the atmosphere by a chemical reaction between nitrogen oxides, volatile organic compounds, and light and heat energy from the sun.
|
||
The effects of air pollution are greatly magnified when temperature inversions, or weather inversions, occur. The video below on the right explains temperature inversions. Ordinarily, air temperature is greatest at the earth's surface and decrease as altitude increases. Certain weather patterns can result in a blanket of warm air being inserted above cooler air at the earth's surface (an inversion), and this can prevent air mixing and trap pollutants at ground level.
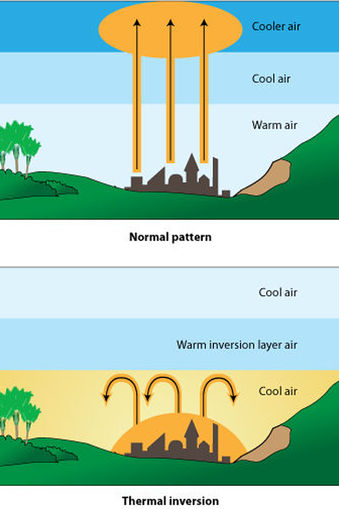
Image source http://www.sciencelearn.org.nz/Contexts/Enviro-imprints/Sci-Media/Images/Temperature-inversion
This video (3 min.) from the National Weather Service in Medford, Oregon, provides a succinct explanation of temperature inversions.
Source http://www.youtube.com/watch?v=L7i7N-je-aM
The widget below shows the air quality for the 02118 zip code in Boston. To insert the widget into a web page for another zip code, paste the following HTML code into your web page:
<iframe height="200" width="310" src="http://epa.gov/cgi-bin/widget.cgi?ZIPCODE"></iframe>,
and insert the zip code of interest in place of ZIPCODE.
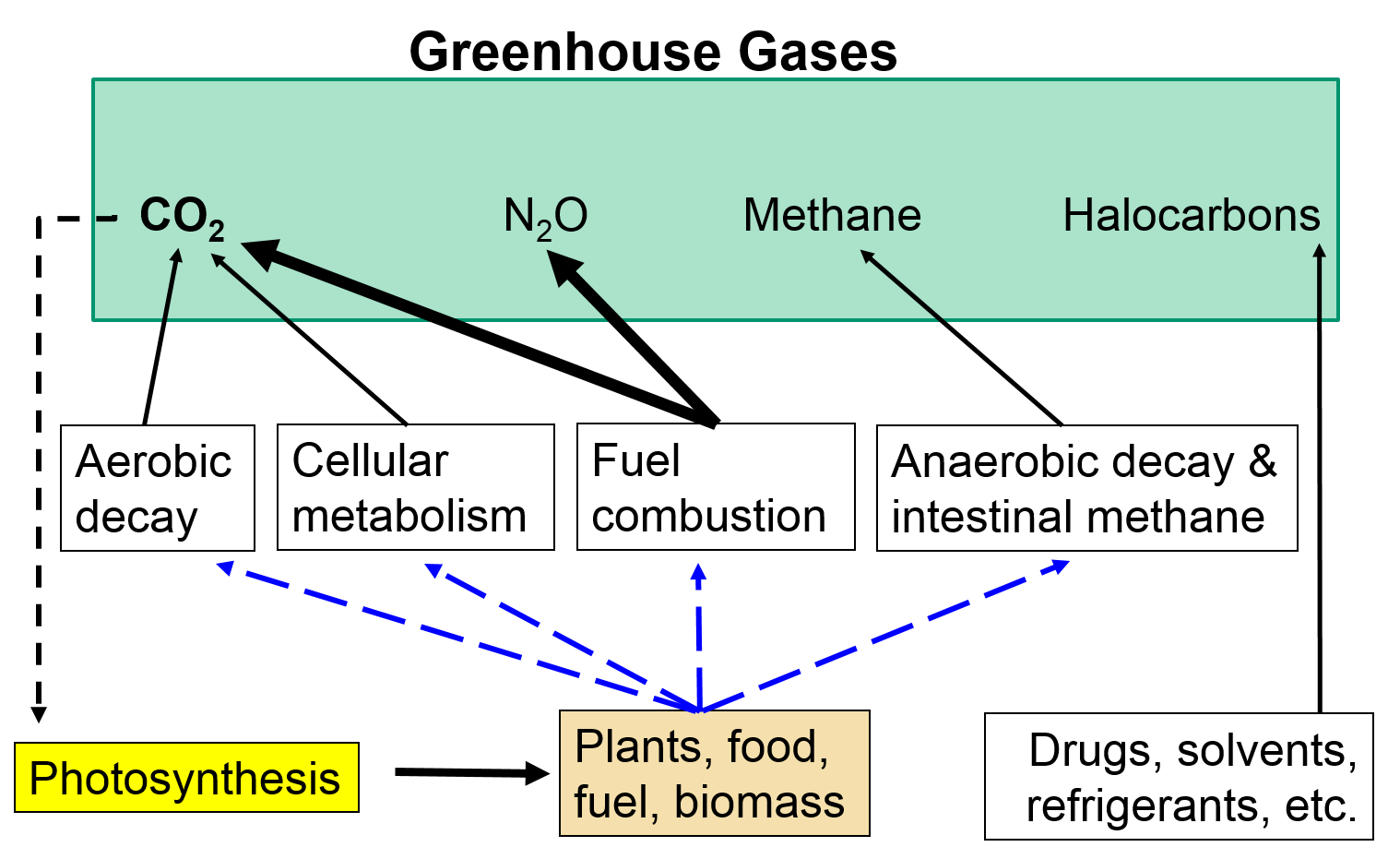
Greenhouse gases are gases that trap heat in the atmosphere. Excess heat trapping produces an undesirable increase in the temperature of the earth that can have far-reaching effects on climate, weather patterns, and human health and well-being.
Carbon dioxide is the most important greenhouse gas, because it it produced in such enormous amounts. We noted earlier that during cellular metabolism food components such as glucose, starch, and fats are combined with oxygen to produce energy, and CO2 and water are by- products.
Fuel combustion similarly oxidizes fuels to produce energy, releasing CO2, nitrogen oxides, and sulfur oxides as byproducts.
And photosynthesis in plants is just the reverse of this in that it uses energy in the form of sunlight to convert CO2 and water into glucose and oxygen.
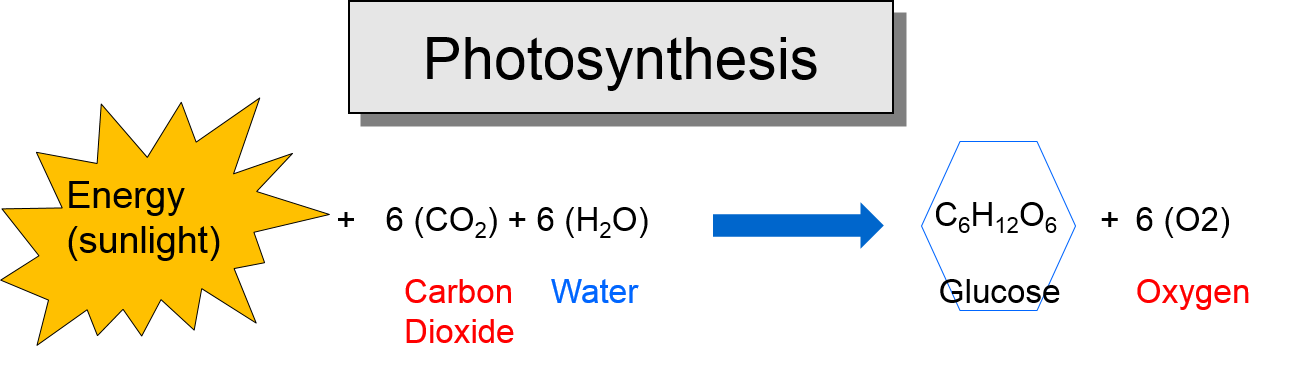
Thus, carbon dioxide is a naturally occurring compound that plays an essential role in the carbon cycle from photosynthesis to cellular metabolism. Nevertheless, the growing combustion of fossil fuels over the past three centuries has pumped enormous amounts of carbon dioxide into the atmosphere.
The iFrame below will enable you to explore the EPA's web pages on greenhouse gases and climate change. Pay particular attention to the links on the upper left hand side of the web page, and be sure to explore the links on
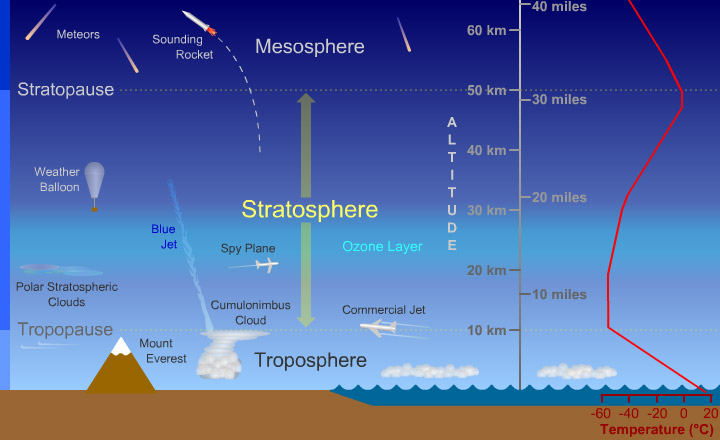
Image source: https://www.windows2universe.org/earth/Atmosphere/images/stratosphere_diagram_big_jpg_image.html