Risk of Breast Cancer
For an excellent and succinct summary of risk factors for breast cancer, see http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-risk-factors
The National Cancer Society also provides an online breast cancer risk calculator.
BRCA1 and BRCA2 Mutations
As noted above, the BRCA1 and BRCA2 mutations can be inherited and lead to an increased risk of breast and other types of cancer. The National Cancer Institute Fact Sheet on BRCA1 and BRCA2 states:
"A woman's lifetime risk of developing breast and/or ovarian cancer is greatly increased if she inherits a harmful mutation in BRCA1 or BRCA2. Such a woman has an increased risk of developing breast and/or ovarian cancer at an early age (before menopause) and often has multiple, close family members who have been diagnosed with these diseases. Harmful BRCA1 mutations may also increase a woman's risk of developing cervical, uterine, pancreatic, and colon cancer (1, 2). Harmful BRCA2 mutations may additionally increase the risk of pancreatic cancer, stomach cancer, gallbladder and bile duct cancer, and melanoma (3).
Men with harmful BRCA1 mutations also have an increased risk of breast cancer and, possibly, of pancreatic cancer, testicular cancer, and early-onset prostate cancer. However, male breast cancer, pancreatic cancer, and prostate cancer appear to be more strongly associated with BRCA2 gene mutations (2–4).
The likelihood that a breast and/or ovarian cancer is associated with a harmful mutation in BRCA1 or BRCA2 is highest in families with a history of multiple cases of breast cancer, cases of both breast and ovarian cancer, one or more family members with two primary cancers (original tumors that develop at different sites in the body), or an Ashkenazi (Central and Eastern European) Jewish background. However, not every woman in such families carries a harmful BRCA1 or BRCA2 mutation, and not every cancer in such families is linked to a harmful mutation in one of these genes. Furthermore, not every woman who has a harmful BRCA1 or BRCA2 mutation will develop breast and/or ovarian cancer."
Nevertheless, it is estimated that 85% of breast cancers are sporadic, i.e., not do to an inherited mutation.
Hormonal Factors
A woman's risk of developing breast cancer depends on hormonal and reproductive history. In essence, any factor that increases a women's total lifetime exposure to estrogens (either endogenous or exogenous
or exogenous ) increases her risk. Estrogens stimulate growth of breast tissue and appear to have a role in the development & growth of breast cancer. Estrogens promote the development of mammary cancer in rodents. They also stimulate proliferation of human breast cancer cells grown in cell culture.
) increases her risk. Estrogens stimulate growth of breast tissue and appear to have a role in the development & growth of breast cancer. Estrogens promote the development of mammary cancer in rodents. They also stimulate proliferation of human breast cancer cells grown in cell culture.
Factors that would contribute to lifetime exposure to endogenous estrogens would include:
- Beginning menstruation at an early age
- Experiencing menopause at a late age
- Later age at first pregnancy or not having children: From American Cancer Society: "Women who have had no children or who had their first child after age 30 have a slightly higher breast cancer risk. Having many pregnancies and becoming pregnant at a young age reduce breast cancer risk. Pregnancy reduces a woman's total number of lifetime menstrual cycles, which may be the reason for this effect."
Exogenous Sources of Estrogen (from an external source, i.e., medications and birth control)
- Recent oral contraceptive use: Studies have found that women using oral contraceptives (birth control pills) have a slightly greater risk of breast cancer than women who have never used them. This risk seems to go back to normal over time once the pills are stopped. Women who stopped using oral contraceptives more than 10 years ago do not appear to have any increased breast cancer risk. When thinking about using oral contraceptives, women should discuss their other risk factors for breast cancer with their health care team.
|
Oral Contraceptives and Cancer From National Cancer Institute: "A 1996 analysis of epidemiologic data from more than 50 studies worldwide by the Collaborative Group on Hormonal Factors in Breast Cancer found that women who were current or recent users of birth control pills had a slightly higher risk of developing breast cancer than women who had never used the pill (2). The risk was highest for women who started using oral contraceptives as teenagers. However, 10 or more years after women stopped using oral contraceptives, their risk of developing breast cancer had returned to the same level as if they had never used birth control pills...."
http://www.cancer.gov/cancertopics/factsheet/Risk/oral-contraceptives http://jnci.oxfordjournals.org/content/94/23/1773.long
|
- Depot-medroxyprogesterone acetate (DMPA; Depo-Provera®) is an injectable form of progesterone that is given once every 3 months as birth control. Women currently using DMPA seem to have an increase in risk, but the risk doesn't seem to be increased if this drug was used more than 5 years ago.
- Postmenopausal Hormone Replacement Therapy (HRT): Hormone therapy with estrogen has been used for many years to relieve symptoms of menopause and to help prevent osteoporosis. The effects on risk of cancer have been very controversial because of conflicting results in epidemiologic studies. There is evidence that combined hormone therapy (estrogen + progesterone) increases the risk of breast cancer. However, the risk gradually reduces to normal 5-10 years after discontinuing usage. within 5 years of stopping combined treatment. The use of postmenopausal estrogen alone does not appear to increase the risk of developing breast cancer. Although ET does not seem to increase breast cancer risk, it does increase the risk of blood clots and stroke. At present, the benefits of HRT do not seem to out way the risks.
|
Tamoxifen - An Estrogen Blocking Drug Tamoxifen is a drug that has an estrogen-blocking effect in the breast, but estrogen-like effects on some other tissues, e.g. uterus & bone.
The Breast Cancer Prevention Trial studied effect of Tamoxifen for 5 years in a large group of women at increased risk. Women ages 35 and older who took a daily dose of 20 mg Tamoxifen for up to 5 years had 50% reduction in risk of breast cancer.
|
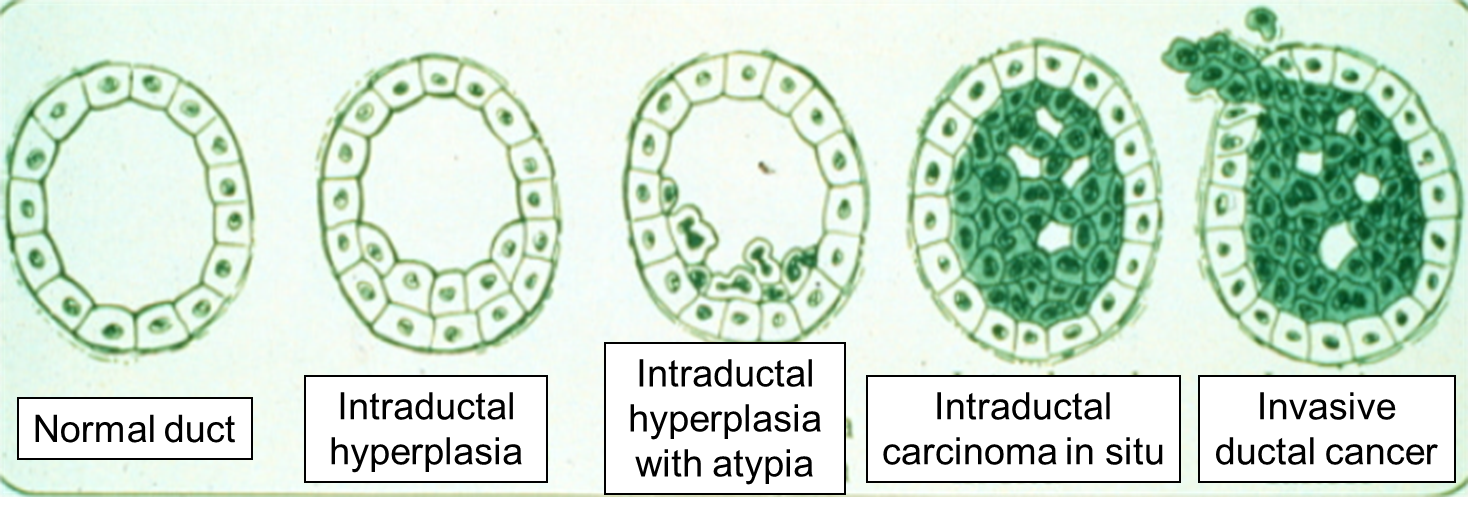
Carcinogens and Breast Cancer
In the video clip below, Dr. David Sherr, from the environmental health department at BUSPH, discusses the potential role of environmental pollutants as risk factors for breast (and other) cancers. Dr. Sherr's research is exploring the molecular mechanisms that initiate and maintain breast cancer. Much of his research has focused on the role of an environmental chemical receptor (the aryl hydrocarbon receptor - AhR) and the role of polycyclic aromatic hydrocarbons (PAHs), which are atmospheric pollutants generated by burning fuel and by cooking meat at high temperatures (e.g., grilling). PAHs are also found in smoked fish. In this video, Dr. Sherr also discusses the difficulties in establishing a causal link between environmental pollutants and cancer.
Other Risk Factors for Breast Cancer
- Alcohol: Drinking alcohol increases the risk of developing breast cancer and other forms of cancer.
- Being overweight or obese: Adipose tissue produces small amounts of estrogen. Being overweight after menopause increases the risk of breast cancer risk by increasing the production of estrogen from adipose tissue.
- Physical activity: There is evidence to suggest that physical activity reduces the risk of breast cancer.