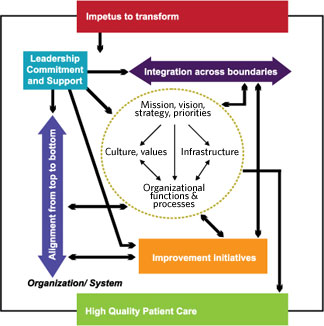
Integration across Boundaries
Integration across traditional organizational boundaries generally occurs at a later stage of transformation. Integration is needed to break down and bridge boundaries between individual components so that a system operates as a fully interconnected unit to support organization-wide goals (Baldrige National Quality Program, 2005). Integration is represented as a horizontal line to signify the importance of working across intra-organizational boundaries. Integration is a multi-faceted concept that applies to all organizational levels and is both an end state for a high-performing system and a strategy for transformation. As a strategy, integrating structures and processes can facilitate the spread of improved clinical practices across the organization.
At the front line multidisciplinary improvement teams that encouraged communication and problem solving across work units facilitate care integration. By themselves, improvement teams often run up against the limits of traditional intra-organizational boundaries. Often teams cannot obtain the commitment of resources or the cooperation from other departments needed to effect change. Without such collaboration, improvement efforts cannot fully make the changes necessary to address sources of problems and to build improvement into the organization such that lasting change occurs.
As part of their transformation organizations/systems often work to integrate clinical care to improve coordination and continuity of care. At the front line, extensive work on patient flow, case management, and electronic support systems (e.g., clinical reminders, registries) is aimed toward improving care for individual patients or populations. Some organizations develop comprehensive planned care models to integrate patient care processes across workgroups, microsystems or the entire organization. Some organizations use service lines to integrate providers and support staff to improve coordination of patient care. However, some service line structures also created new silos, integrating care within the lines but impeding integration across them.
To move beyond the limits of a team’s or service line’s authority and resources, integration also is needed at the systems or organizational level in the form of structures and processes that involve managers with decision-making authority and responsibilities spanning the organization. However, integration at these high levels appears to be more difficult to achieve than integration at the font line.
A deliberate focus on integration often occurs after an organization has learned to do redesign work and to address alignment. Many organizations/systems use quality management steering committees to address cross-organizational issues in high-priority QI efforts, but only a few move beyond integration around improvement projects to build integration into the way they work by using standard or newly-invented management structures.
Example
Some organizations/systems working on medication errors are unable to acquire resources to implement new technologies, such as bar coding, which result in less than fully effective workarounds.
Example
Site D redesigned its horizontal management structures to create multidisciplinary groups responsible for care processes defined by patients’ experiences (e.g., inpatient, outpatient, and emergency care teams). In addition, an integration committee staffed by senior leaders, including the CEO, addressed redundancy, conflicts, and the spread of best practices across groups. Site D saw these structures as transitional, recognizing inconsistencies with other structures in the medical center.
