Diabetes
The rise in blood sugar after a meal or snack stimulates the secretion of the hormone insulin from the β-cells in the pancreas. Insulin circulates in the blood and binds to insulin receptors on muscle and fat cells. Binding to the receptor triggers phosphorylation of a protein called 'insulin receptor substrate' or IRS-1. This, in turn, triggers the insertion of specialized glucose transporters (GLUT4) into the cell membrane, where they act as a conduit to facilitate the entry of glucose from the blood stream into the cell. These events are depicted in the image below showing how glucose molecules in a capillary enter a muscle cell.
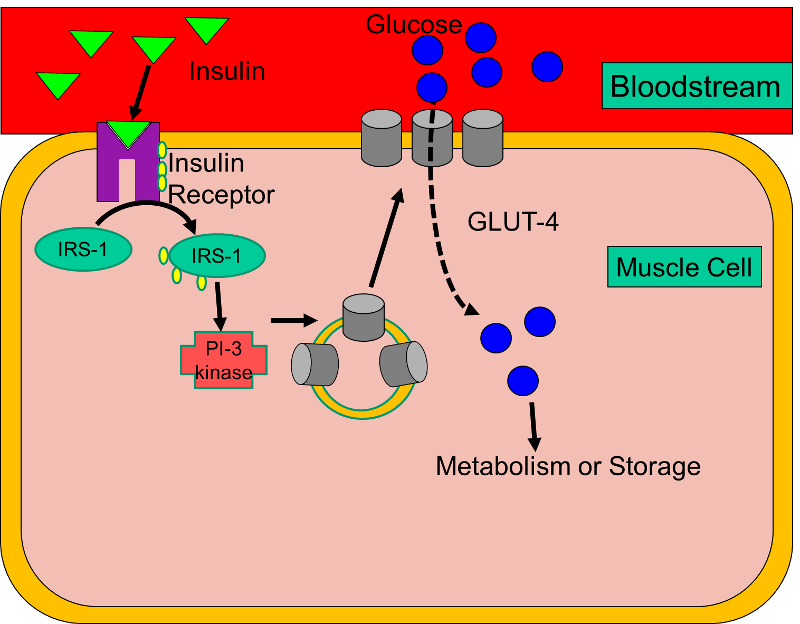
Type I Diabetes (also called insulin-dependent diabetes or juvenile diabetes) results from an autoimmune process that destroys the β-cells, causing a lack of insulin. As a result, glucose cannot enter fat or muscle cells, so blood levels of glucose rise, and there is increasingly greater reliance on breakdown of fat and protein to provide an alternate source of fuel.
In contrast, Type II Diabetes (also known as adult onset diabetes or non-insulin dependent diabetes) is primarily due to insulin resistance. Despite adequate levels of insulin, at least initially, the interaction between insulin and its receptor is dysfunctional. As a result, GLUT4 transporters are not efficiently inserted into the membranes of fat and muscle cells, and glucose concentrations in blood rise (hyperglycemia), leading to endothelial cell dysfunction.
Both type 1 diabetes and type 2 diabetes are independent risk factors for coronary artery disease, and diabetes may predispose to multiple small coronary and peripheral vessels.
Complications of Diabetes
The complications of diabetes develop gradually, but they can be disabling and can eventually be fatal. Some of the more prominent complications include:
- Coronary artery and peripheral vascular disease. The risk of stroke is two to four times higher for people with diabetes, and the death rate from heart disease is two to four times higher for people with diabetes than for people without the disease, according to the American Heart Association.
- Nerve damage (neuropathy). High concentrations of blood sugar cause endothelial dysfunction which can injure capillaries supplying peripheral nerves, especially in the legs. This may cause tingling, numbness, burning or pain that begins at the tips of the toes or fingers and gradually spreads upward. Without proper control of diabetes, the neuropathy can progress to the point of causing a complete loss of sensation in the affected limbs. Diabetic neuropathy can also cause digestive problems (nausea, vomiting, diarrhea or constipation) and can contribute to erectile dysfunction in men.
- Kidney damage (nephropathy). Damage to the blood vessels and capillaries in the kidney can lead to kidney failure or irreversible end-stage kidney disease.
- Eye damage. Diabetes can damage the blood vessels of the retina (diabetic retinopathy), potentially leading to blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Amputation of toes, feet or legs. The combination of neuropathy, endothelial cell dysfunction, and atherosclerotic disease that interferes with arterial supply to the legs can result in loss of sensation, unrecognized trauma, blisters, ulcers, and serious infections which can ultimately require amputation.
- Increased susceptibility to infection: Poorly controlled diabetes is associated with an increased risk of soft tissue infections and gum disease.
- Osteoporosis. Diabetes accelerates loss of bone mineral density.
- Alzheimer's disease. Type 2 diabetes may increase the risk of Alzheimer's disease and vascular dementia.
- Hearing problems. Diabetes can also lead to hearing impairment.
NOTE: Diabetes is the leading cause of blindness, renal failure, and amputation in the United States.
|
Type 2 Diabetes: A Great, But Unrecognized Risk The excerpts below are from R. Todd Hurst and Richard W. Lee: Increased Incidence of Coronary Atherosclerosis in Type 2 Diabetes Mellitus: Mechanisms and Management. Ann Intern Med. 2003;139:824-834.
"Type 2 diabetes mellitus is a vascular disease. More than 3 out of 4 diabetic patients die of causes related to atherosclerosis, in most cases (75%) because of coronary artery disease. Yet, 70% of diabetic persons do not believe they are at serious risk for cardiovascular disease. An increasing number of patients have diabetes and its attendant complications, and this trend is predicted to continue. In the United States, the number of diabetic patients is expected to increase from 15 million to 22 million by 2025. This increase correlates strongly with increasing obesity and is reflected in the development of diabetes at an earlier age. The younger age at onset portends an increased future prevalence of premature coronary artery disease and resource utilization that will exceed the current $100 billion annual expenditure in the United States. Type 2 diabetes increases the risk for coronary artery disease by 2 to 4 times in the overall population. Haffner and colleagues found that diabetic patients with no history of coronary artery disease have the same risk for future myocardial infarction as do nondiabetic patients with known disease. The National Cholesterol Education Program considers diabetes to be a coronary disease equivalent in their lipid guidelines. The risk is even greater in women. Diabetes eliminates the usual female advantage in risk for death from coronary artery disease; these patients have a 5-fold to 8-fold higher death rate than do nondiabetic women." --------------------------------------------------------------------- [My Comment: Type 2 diabetes represents an enormous public health challenge. It is a highly prevalent condition whose incidence continues to rise with the burgeoning problem of overweight and obesity, and it carries a substantially increased risk of complications and death from a variety of cardiovascular diseases. It presents a rapidly expanding problem that imposes a growing burden of premature disability, death, and cost. One important aspect of the challenge to public health is that it is a condition which is largely preventable by proper nutrition and physical activity. Moreover, even after it occurs, the long range complications can be greatly diminished or delayed by proper management. A second aspect of the public health challenge is that the disease is asymptomatic at first, and many afflicted individuals are unaware that they are affected. The third aspect of the public health challenge, as these authors point out, is that even when diagnosed, the majority do not believe they are at risk and are not taking adequate care to manage their disease./ Wayne LaMorte]
|
Primary Prevention of Type 2 Diabetes
Hu, FB, et al: Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001;345:790-7.
This prospective cohort study followed 84,941 female nurses from 1980 to 1996; the subjects were initially free of diagnosed cardiovascular disease, diabetes, and cancer. The investigators defined a "low risk" group based on five characteristics:
- BMI < 25
- a diet high in cereal fiber and polyunsaturated fat and low in trans fat and glycemic load
- moderate-to-vigorous physical activity for at least 30 min per day
- no current smoking
- consumption of an average of at least half a drink of an alcoholic beverage per day.
After 6 years of follow-up, the study found that overweight or obesity was the single most important predictor of type 2 diabetes. However, "... lack of exercise, a poor diet, current smoking, and abstinence from alcohol use were all associated with a significantly increased risk of diabetes, even after adjustment for the body-mass index. "
Only 3.4% of the women in the cohort met the criteria for being "low-risk." Nevertheless, compared with the rest of the cohort, these low-risk women had a risk ratio of 0.09 (95% confidence interval: 0.05 - 0.17), suggesting that 91% of the cases of type 2 diabetes in the cohort (95% confidence interval: 38-95%) could be attributed to a lifestyle that did not conform to the low-risk criteria. They concluded that the majority of cases of type 2 diabetes could be prevented by the adoption of a healthier lifestyle.
The Diabetes Prevention Trial (The Diabetes Prevention Program (DPP) Trial)
In May 2010 Dr. Francis Collins, Director of the National Institutes of Health, appeared as a witness before the Senate Subcommittee on Labor – HHS – Education Appropriations to support the NIH budget request for FY 2011. Dr. Collins testified:
"For type 2 diabetes, prevention appears to be the name of the game. This form of the disease, which accounts for more than 90% of diabetes among adults, often can be averted or delayed by lifestyle factors. The NIH-funded Diabetes Prevention Program (DPP) trial showed that one the most effective ways to lower the risk of type 2 diabetes is through regular exercise and modest weight loss. There is good reason to believe that such efforts may lead to a lifetime of health benefits. A recent follow-up study of DPP participants found the protective effects of weight loss and exercise persist for at least a decade. The United Health Group has recently announced a partnership with Walgreen's and the YMCA to implement the results of this groundbreaking NIH-funded research on a broad scale."
Tuomilehto J, et al Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 20013441343-50.
A Finnish group conducted a randomized clinical trial to test whether lifestyle changes could prevent type 2 diabetes. The investigators enrolled 522 middle-aged overweight subjects who were pre-diabetic based on glucose tolerance tests
to test whether lifestyle changes could prevent type 2 diabetes. The investigators enrolled 522 middle-aged overweight subjects who were pre-diabetic based on glucose tolerance tests .
.
- Subjects were randomly assigned to an intervention group
 receiving individualized counseling aimed at reducing weight, total intake of fat, and intake of saturated fat and increasing intake of fiber and physical activity.
receiving individualized counseling aimed at reducing weight, total intake of fat, and intake of saturated fat and increasing intake of fiber and physical activity. - Subjects "... in the control group were given general oral and written information about diet (a two-page leaflet) and exercise at base line and at subsequent annual visits, but no specific individualized programs were offered to them. They completed a three-day food diary at base line and at each annual visit, using a booklet illustrating the sizes of portions of food.An oral glucose-tolerance test was performed annually; the diagnosis of diabetes was confirmed by a second test.
Subjects in the intervention group lost an average of 4.2 kg of body weight after one year, compared to 0.8 kg in the control group. By the end of the second year average loss in the intervention group was 3.5 kg compared to 0.8 kg in the control group (P<0.001 for both). After four years of follow-up the incidence of diabetes in the intervention group was 11% (95% confidence interval:6-15%), compared to 23% (95% CI: 17-29) in the control group. Moreover, it was shown that the likelihood of prevention of diabetes was directly associated with changes in lifestyle. Consequently, this study shows that type 2 diabetes can be prevented by changes in the lifestyles of high-risk subjects.
An editorial on this report acknowledged that it convincingly showed that type 2 diabetes was delayed in the short term, but raised the question of whether the lifestyle changes could be maintained and how long the reduced incidence of diabetes would last. The editorial comment went on to say that
"... physicians and policymakers may wish to consider whether such intervention programs should be routinely covered by insurance companies and made more broadly available in primary care settings. Such decisions will probably require evidence that the complications of diabetes can be delayed or prevented. It is reasonable to expect, however, that the onset of microvascular complications will be delayed, since the frequency of these complications is closely correlated with the duration of diabetes."
The authors of the editorial concluded by saying:
"At present, the results of the Finnish Diabetes Prevention Study should encourage physicians and other health care providers to persevere in the difficult task of promoting a healthy lifestyle, since by doing so they will give patients a better chance at a life less burdened by many diseases, including type 2 diabetes."
Secondary Prevention of Type II Diabetes
The Look AHEAD Trial
The studies in the previous section focus on the efficacy of lifestyle changes in preventing the development of type II diabetes. A separate but related question is whether lifestyle changes are beneficial in preventing adverse cardiovascular events after type II diabetes has already developed. This question was addressed in a multi-center randomized clinical trial [The Look AHEAD Research Group: Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N. Engl. J. Med. 2013;369:145-54.] Study subjects were overweight or obese. The intervention promoted weight loss through decreased caloric intake and increased physical activity, while the control group received diabetes support and education. During a median follow-up of 9.6 years, the intervention group lost more body weight (8.6% vs. 0.7% after one year; 6.0% vs. 3.5% at study end) and had reductions in glycated hemoglobin levels and increase in fitness. Despite these beneficial changes, the reduction in cardiovascular events in the intervention group was not statistically significant (rate ratio: 0.83; 95% confidence interval 0.83-1.09). The intervention group experienced fewer cardiovascular deaths and fewer myocardial infarctions, but despite a study population consisting of 5,145 subjects, the differences were not statistically significant. Perhaps these findings confirm Benjamin Franklin's adage that "An ounce of prevention is worth a pound of cure."