
An Outbreak of Hepatitis A in Sparta, MA
Contributors
After successfully completing this case student, the student will be able to:
This project was supported by grant # 05-078 from Health Resources and Services Administration (HRSA). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of HRSA.

 You graduated from Boston University School of Public Health last spring and began working for the Massachusetts Department of Public Heath just two weeks ago. DPH was severely understaffed, and after a brief orientation you were given your first field assignment.
You graduated from Boston University School of Public Health last spring and began working for the Massachusetts Department of Public Heath just two weeks ago. DPH was severely understaffed, and after a brief orientation you were given your first field assignment.
Your supervisor says:
"We've been following a situation in the town of Sparta about an hour an a half west of here on the turnpike. About two weeks ago they reported a case of hepatitis A. A 31 year-old woman was seen in the emergency room of the local hospital complaining of fever, nausea, and severe fatigue. She also reported that her urine was very dark, and her stools were very light in color over the past 24 hours. She had been previously healthy and had no past history of jaundice. She had a low grade fever (100.6 ° F), mild scleral icterus (the whites of her eyes were slightly yellow), and her liver was enlarged. She had no rash. Here are the results of her blood tests."
Her Liver Function Tests:
Link to information on nterpretation of Liver Function Tests
Her Serology Tests:
Your supervisor continues:
"The hepatitis B serologic tests indicated that she had had hepatitis B in the past, but it resolved. The positive IgM anti-HAV indicates that she had an acute infection with hepatitis A. The physician reported the case to the local board of public health, and they relayed the information to us."
Your supervisor says:
"There has been a steady increase in the number of cases. They asked us to help investigate the source of the outbreak. So this will be your first assignment. I want you to be involved in all aspects of the case, including investigation of the outbreak, making recommendations regarding control and prevention (including organizing IG administration if you decide it's necessary), collection and analysis of data to determine the source, reviewing their sanitation procedures, and helping them organize training and educational to prevent future problems. Here are some quick references on hepatitis that might be useful to you. Take a look at these. The CDC Fact Sheet is particularly useful, because it gives the essential facts in a concise format. When you are finished, I'll quiz you to see if you understand the background material."
This link may also be of interest:
Note also that the incidence of hepatitis A in the United States has fallen dramatically as a result of the introduction of a vaccine for hepatitis A.
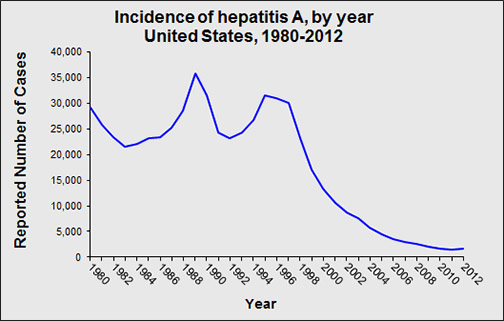
Source: http://www.cdc.gov/hepatitis/Statistics/
Your supervisor continues:
"As you know, the public health issues for hepatitis A are based on the biology of the disease. Let me ask you a few questions about the biology and epidemiology of hepatitis A."

The graph below helps in understanding the sequence of events during hepatitis A infection. After ingestion the virus is taken up by the gastrointestinal tract and travels by blood to the liver where it infects liver cells and replicates inside them, causing them to burst when new virus particles are released. Cell bursting releases enzymes normally inside the liver cells, such as ALT, AST, and alkaline phosphatase, and concentrations of these enzymes in the blood become abnormally high.
Source: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5304a1.htm
Some replicated viruses get into the blood and others are secreted into bile, which enters the intestine and deposits many virus particles into the intestine causing high concentrations of virus in stool. Infected people are most infectious during the period from two weeks before the appearance of symptoms until one week after symptoms began. The average incubation period (time period between infection and development of symptoms) is about 28 days, with a range of 15-50 days. This will be important to understanding the course of the epidemic in a population.
A positive test for anti-HAV IgM clinches the diagnosis of acute infection. After recovery, the IgM gradually declines, but anti-HAV IgG increases, which confers immunity against another hepatitis A infection. So, if someone has elevated blood levels of anti-HAV IgG, but not IgM, it indicates that they had a past infection that resolved.
The next morning you arrive in Sparta and meet with Bernard Barstow, the Director of the Sparta Health Department. He thanks you for coming out and gives a little more background regarding the outbreak. Play the video below to hear what he has to say (1:05).
Barstow continues:
"We generally see less than 5 cases of hepatitis A each year in Sparta scattered throughout the year. Whenever a case occurs, we investigate to try to ascertain the source and to prevent any additional spread. If it involves a diapered child, or a day-care attendee, or a food handler, we want to prevent further transmission. These sporadic cases tend to be the result of travel outside the US, or from household or sexual contact with an infected person; about half the time we never figure out what the source was. In this case, we were first alerted when the emergency room physician reported the occurrence of hepatitis A in the 31 year-old woman. Over the next several days three other local physicians called the board of health and reported four more cases, so we began to think that this was more than the usual sporadic cases.
"Massachusetts now uses on online reporting system for surveillance of reportable infectious diseases. It's called MAVEN, which stands for Massachusetts Virtual Epidemiologic Network. This system provides a uniform means by which hospitals, laboratories, and health departments across the state can report relevant information about anyone who has developed a reportable infectious disease. This has greatly speeded up reporting and case investigation, and it makes it possible to look for trends and epidemics across the state. Other states are beginning to use similar systems for infectious disease surveillance. However, in addition to reporting cases to the MAVEN system, we also keep our own listing of all reportable cases in our town. This comes in handy if we have reason to suspect that there may be an infectious disease outbreak."
Disease surveillance is a primary function of public health. A good way to quickly learn how disease surveillance functions is to take a look at this online module on Disease Surveillance.
"State laws require that certain diseases be reported in order to identify health problems that require attention and to monitor changes in disease frequency over time. In Massachusetts the state DPH has the authority to determine which diseases must be reported and how. State law specifically lists these diseases and stipulates that household members, physicians and other health care providers must promptly report cases to the local board of health; the local board is then required to report this information (including the case's name, date of birth, age, sex, address and disease) to the state Department of Public Health (DPH). Similarly, all laboratories, including those outside of Massachusetts, performing examinations on any specimens derived from Massachusetts residents that yield evidence of reportable infections must be reported to the Massachusetts DPH. These state laws and regulations provide the basis for an ongoing system of disease surveillance."
"Surveillance data is important for identifying sudden increases in disease occurrence, but it's also important for following secular (long-term) trends and patterns of disease. For example, it would be useful to keep tabs on the frequency of cases of West Nile virus to guide decisions about mosquito control. In addition, surveillance data for HIV would be important for following long-term trends and to anticipate the needs of the population. Surveillance data is also useful for monitoring the effectiveness of prevention programs. And finally, surveillance data sometimes generate hypotheses. For example, in 1980 it was discovered that many of the cases of toxic shock syndrome occurred in menstruating women. This led to research that demonstrated that the syndrome was associated with a particular brand of tampon, and the product was promptly removed from the market."
Take a look at this online module which has more detailed information about Infectious Disease Surveillance in Massachusetts.
Additional Resources:
One of Barstow's coworkers turns to you and says, "I don't get it. What about the regulations in the Health Insurance Portability and Accountability Act (HIPAA)? With all these HIPAA regulations on privacy of medical information, how can doctors, hospitals and labs report diseases to the local or state departments of health with personal identifiers?"

Other resources regarding confidentiality of health-related information:
Barstow summarizes the information in these documents and continues:
"When we saw the first group of cases, I sent a notice to the local hospitals, clinics, clinical laboratories, and local area physicians, indicating that a cluster of four cases of hepatitis A had been identified, and I reminded them that if they saw any evidence of new cases of hepatitis A, they were required to report them to the Department of Public Health promptly.
A separate online module provides a useful summary of how to conduct outbreak investigations. One section in particular discusses the steps that are undertaken in a typical outbreak investigation. You should review these.
Dr. Richard Dicker points out that outbreaks are identified either by regular analysis of surveillance data or, more commonly, through calls from a health care provider or citizen who knows of several cases. A small cluster of similar cases might seem unusual, although the total number of cases and the denominator for the population are frequently unknown. Consequently, it is important to verify that an apparent outbreak is real by comparing the number of cases during the current time period with what one has observed during preceding periods.
One needs to consider that an increase in the reported number of cases could also be due to:
Changes in the case definition
Improvements in diagnostic or screening procedures
Increased attention to the disease because of local or national interest
Changes in the age distribution of the population
Influx of significant numbers of new permanent or temporary residents.
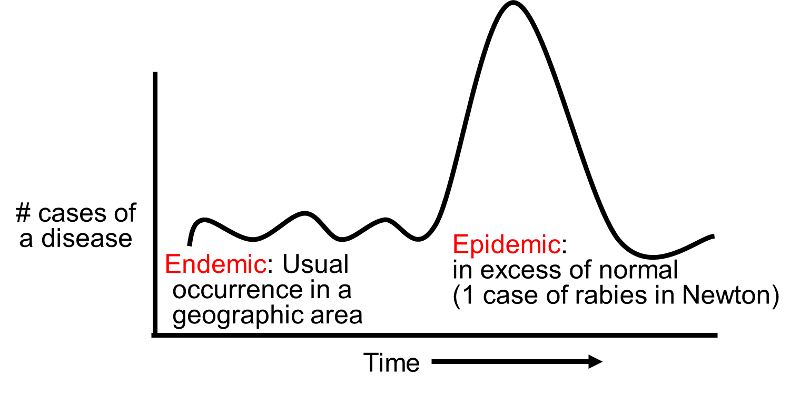
The term endemic refers to the usual frequency of a disease occurring in a particular location. An epidemic can be defined as an increase in the frequency of disease over and above the endemic rate. The terms "epidemic" and "outbreak" are synonymous. Finally, the term pandemic refers to the presence of multiple epidemics across the globe. These are relatively loose definitions, and there are no strict criteria that distinguish these terms. For example, if a community has historically been unaffected by rabies, then the occurrence of a single case might logically be classified an epidemic of sorts, particularly since its occurrence would indicate a potentially important increase in potential risk of future cases. It should also be noted that the word "pandemic" is frequently mistaken to imply an epidemic of severe disease, i.e., of particular virulence. However, this is incorrect; regardless of severity, it refers to the simultaneous occurrence of multiple epidemics across the globe.
Barstow points out,
"Of course, before we got too carried away counting cases, we had to confirm the diagnosis, confirm that there was an unusual number of cases, and then decide on a case definition. All four of the first cases had a typical clinical picture (jaundice, fever, nausea, vomiting, fatigue, loss of appetite), and they also had blood tests that showed elevated concentrations of bilirubin and liver enzymes. They also had anti-hepatitis A IgM antibodies. The symptom complex of jaundice, fever, nausea, vomiting, fatigue, loss of appetite was useful for finding potential cases, but the ultimate determination of whether someone was a 'case' or not depended on the lab test to see if they had elevated IgM for HAV."
You will find it useful to review this brief discussion on confirming the presence of an outbreak.
A case definition is a standard set of criteria used to define individuals who are cases. A specific definition helps identify and count cases consistently over time and from place to place. The components of a case definition include:
Criteria for a case definition should be simple, objective, and discriminating (i.e. able to distinguish between people with disease and those without disease.
Also, case definitions should not include risk factors that you may want to evaluate, since all of the cases would have the risk factor, and this would be misleading. A case definition is not the same as a clinical diagnosis. Case definitions are an aid to conducting an epidemiologic investigation, whereas a clinical diagnosis is used to make treatment decisions for individual patients.
How specific should the definition be? Sometimes investigators will use a loose definition early on to help them identity the extent of the problem. However, once the investigators progress to the stage of conducting analytic studies to test their hypotheses, a more specific definition should be used in order to reduce misclassification which would bias the results.
For a nice overview on how to formulate case definitions, see the page on this topic in the module on Outbreak Investigations."
Bartow continues,
"In addition to using the MAVEN system for reportable infectious diseases, we also use an Excel spreadsheet to record the data on cases with reportable diseases in our community. Each case is listed on a separate row. This is called a 'Line Listing. With the data in a line listing like this, we can also use Excel to create an epidemic curve. An epidemic curve basically summarizes the onset of new cases of disease over time, and it can be very useful in giving you some important clues about the source of an outbreak. Here is a link to our current spreadsheet with our line listing.
Link to initial line listing
If you aren't familiar with Excel or if you don't know how to create an epidemic curve, you can go to the module on Descriptive Epidemiology, which has two short videos that illustrate simple methods for creating an epidemic curve in Excel. The Excel file called Epi_Tools.XLSX also has two worksheet that illustrate how to do this quite easily. Check these out, and then see if you can use the information in the Initial Line Listing to create an epidemic curve from the Initial Line Listing file."
Did your epidemic curve look something like this? If not, you better go back and try again. The ability to create these graphs accurately is an important skill for you to develop. It will come in handy in a variety of circumstances

Epidemic curves tell you more than just whether or not there is an outbreak. Take another look at our epidemic curve. Note that the number of cases rises very quickly, peaks, and then begins to fall off. Also, so far all of the cases are contained within a single incubation period. Also bear in mind that the average incubation period is about 28 days, with a range of 15-50 days.
Take a quick look at this link to a concise description of the three main types of epidemic curves.

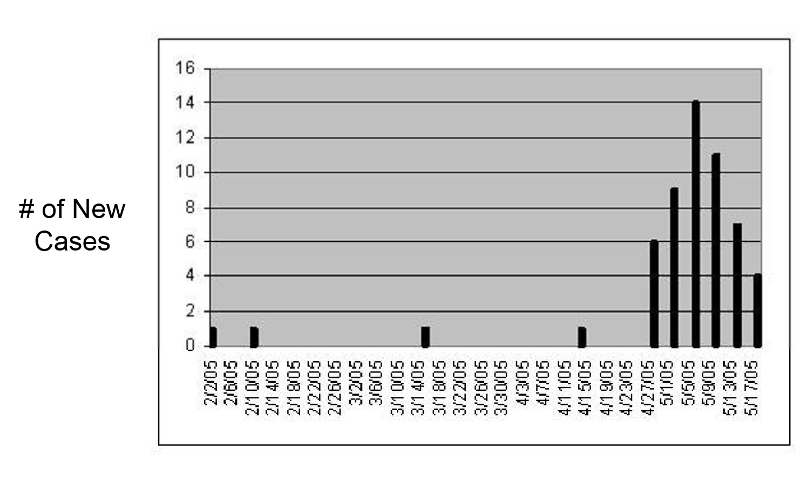
Person, place, and time are the three characteristics one focuses on in descriptive epidemiology. The line listing gives us some information about person, and the epidemic curve gives us a visual sense of how the outbreak evolved over time. Given what we know about the biology and epidemiology of hepatitis A, the information suggests a point source, possibly contaminated food or an infected food handler.
The spot map below focuses on "place" by showing where each of the known cases lives. The cases are clustered somewhat more densely in the center of Sparta, but they are fairly scattered and do not suggest a specific location. So, in this case, the spot map by itself does not help pin down the source. These cases could have been exposed to a common source, such as an infected food handler, but they also could have been infected during foreign travel. For example, they might have been a group of residents from a church or school recently returned from a trip to South America.

Hypothesis-generating interviews are preliminary interviews conducted with a limited number of cases (perhaps 8-10) in order to identify possible sources of exposure to the infectious agent. The cases should be typical cases drawn from a representative sample of the population (e.g. not all one race, gender, or age group), and the interviews should ideally be conducted by a single investigator. Before conducting interviews, the investigator should review the features of the disease and consider likely sources based on the biology of the disease (e.g. known modes of transmission) and information from past outbreaks. The interview should explore exposures during a specific time period, based on the onset of disease and the know incubation period; this focuses the interview on the period during which exposure was likely to have occurred. The information gathered usually includes basic demographic information (age, gender, residence, occupation), clinical details (date of onset, duration of disease), and many questions regarding possible exposures (contact with other ill persons, food history, water exposures, exposure to animals, travel, occupational exposures, hobbies, etc.). The conversation should be open-ended and wide-ranging and not strictly confined to well-established sources of disease or modes of transmission. In difficult investigations with few clues investigators have sometimes gathered several cases together to discuss possible common exposures. In other cases investigators have found it useful to visit the homes of the cases and look through their refrigerators and food shelves for clues.
After reviewing these brief interviews, indicate what hypothesis you have come up with regarding the source of the outbreak
|
Jillian Grey, Elementary School Teacher (1:33) |
Richard Martin, Father of 8 Children, (5 with hepatitis) (2:50) |
|
Peter Drew, Beer Distributor (2:05) |
Emily Shultz, Student (and aspiring epidemiologist) (1:44) |
Helpful Resources for developing a questionnaire, conducting an interview, and formulating a hypothesis:
 In reality one begins to form hypotheses as soon as information about the outbreak begins to emerge. If you know what the disease is, your hypotheses will take into account its biology, what the reservoirs of disease are, how it is usually transmitted, its known risk factors, and its incubation period. In addition, descriptive epidemiology attempts to identify similarities in person, time, or place that may suggest hypotheses regarding the cause of the outbreak. For example, an epidemic curve illustrates the number of cases that occurred over time; it helps establish that there is an outbreak, and the shape of the curve may also suggest the nature of the source (e.g. isolated point source versus continuous common source).
In reality one begins to form hypotheses as soon as information about the outbreak begins to emerge. If you know what the disease is, your hypotheses will take into account its biology, what the reservoirs of disease are, how it is usually transmitted, its known risk factors, and its incubation period. In addition, descriptive epidemiology attempts to identify similarities in person, time, or place that may suggest hypotheses regarding the cause of the outbreak. For example, an epidemic curve illustrates the number of cases that occurred over time; it helps establish that there is an outbreak, and the shape of the curve may also suggest the nature of the source (e.g. isolated point source versus continuous common source).
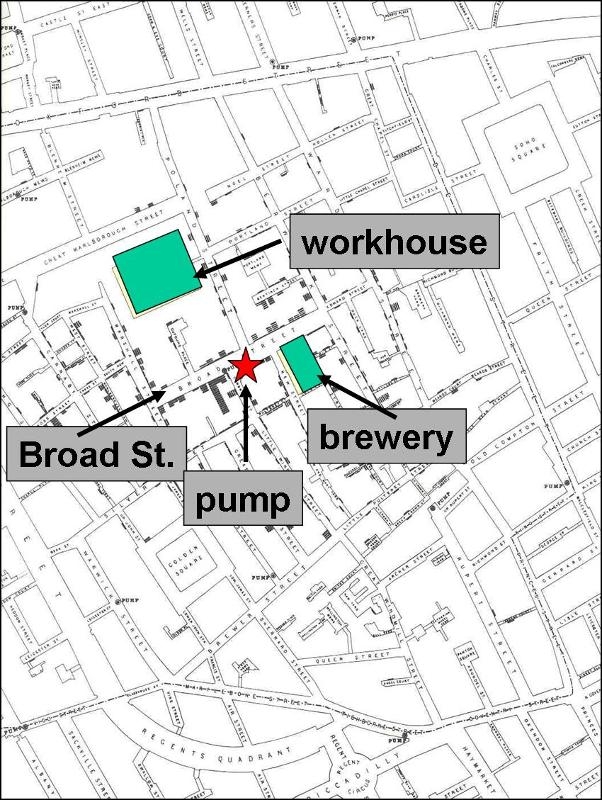
Spot maps can be used to illustrate the residence or work place of each of the cases that may suggest the source, such as John Snow's map (shown on the right) of cholera cases in London in 1852 clustered around the Broad St. pump.
Similarities in personal characteristics may also suggest the cause (e.g. common occupations, age, school attended, etc). Descriptive epidemiology focuses entirely on similarities among the cases and does not establish the cause. Hypotheses that are generated need to be tested by analytic studies that compare two or more groups of people (e.g. cases and controls who did not get the disease).
Putting It All Together
Now let's put the information we have so far together. The epidemic curve for the Sparta rises very quickly, peaks, and then begins to fall off. Also bear in mind that the average incubation period for hepatitis A is about 28 days, with a range of 15 to 50 days. So far all of the cases are contained within a single incubation period. Also, consider the preliminary information in the line listing, specifically the ages of the cases. We know that hepatitis A is transmitted via the fecal-oral route, that is, virus particles in the stool of an infected person somehow get ingested. This can occur as a result of travel to a developing country with suboptimal sanitation, sexual contact (especially MSM), in a child day-care setting where fecal contamination and children putting things into their mouths are common elements, or when food is contaminated, e.g., by an infected food handler.

After you return from conducting these interviews, you tell Barstow that your working hypothesis is that the epidemic was probably initiated by a single person, most likely a food handler working in the Dairy Queen, or the Sparta Bakery (also known as "Lenny's" Bakery), or Chi Chi's. Now you need to decide how you will go about conducting an analytical study in order to test these hypotheses in order to establish the source of the outbreak. You may find the following article helpful.

The next series of questions deals with potential biases that might affect the results of our analytical study. You may want to review our online module on Bias from the core course.

You and Barstow and his staff have collected data from all of the available cases and from a comparison group of non-diseased subjects matched by age and by neighborhood. A portion of the collected data is provided in the accompanying file:
Analyze these data to test the hypothesis that hepatitis was transmitted as the result of exposure from the Dairy Queen, Chi Chi's, or the Sparta (Lenny's) Bakery. You will have to test each of these hypotheses separately.
[Hint: Organize the counts of exposed & unexposed cases & controls into a 2x2 table. The Epi_Tools.XLS Excel spreadsheet may also be useful for computing the confidence intervals for the measures of association that you need to compute. (See Other Resources on the right side of the page.)]
Sparta Analytical Data

The next morning you accompany Barstow and one of his inspectors, Christine, to Lenny's bakery. Lenny Sampson is the owner and manager of The Sparta Bakery (1:58)
Barstow says this has never happened to him before. Food establishment owners are often anxious and defensive about inspections, but he is usually able to quickly convince them that it is in their best interest to cooperate. He says, "Maybe we should check the state laws on this. Let's look in the Law Library."
After reviewing the regulations in the Law Library, answer the following questions:

Comments from Two Health Department Directors
Barstow makes a phone call to the local police chief and explains the situation; he also faxes a copy of the Code of Massachusetts Regulations to him and to Leonard. The police chief calls Leonard, who has already spoken to his lawyer. Leonard concedes to the chief that he was hasty and overreacted, and his lawyer advised him to comply. Several hours later you, Barstow, and Christine are back at Lenny's. Lenny again meets you at the door and says, "Well, I checked with my lawyer, and I read the regulations. You can go ahead and inspect. It's just that I run this place the best I can, and I don't want any trouble." (2:52)
Obviously, Lenny is not a stickler for details. It appears that his employees do a lot of "hands on" food preparation, but there is little evidence that handwashing is stressed, and they don't appear to wear gloves, either.
After the inspection, Barstow gets a phone call from the Department of Public Health in Mansfield, one of the adjacent towns. He learns that a physician reported a case of hepatitis A in a patient, James R., who had become ill on April 14, 2005. The patient told the physician that he went to the emergency room at the Sparta Hospital on April 14, because of nausea, vomiting and diarrhea, but they made him wait a long time to be seen. He had been drinking and was impatient. He was eventually seen by a physician, who wanted to order blood tests, but the patient became agitated and didn't want to wait , so he signed himself out of the emergency room. He continued to be ill, however, and eventually went to a physician in Mansfield, where he lives; blood tests were now done and showed a positive IgM anti-HAV. The board of health in Mansfield notified the Sparta board of health because the patient admitted to his physician that he had worked at Lenny's Bakery.
Go back and re-examine the initial line listing and locate James R. based on the date of onset of his symptoms.
Link to initial Line Testing

That afternoon you and Barstow return to Lenny's to ask about James R.
Lenny admits that James had worked the night shift intermittently, but that he hadn't seen him for a while, and he had forgotten about James. When you interview the bakery workers, one of James's co-workers on the night shift says that James R. used to do a lot of icing and glazing of pastries, and he frequently did this with his bare hands. Later that afternoon you interview James R., who admits that, "Sometimes I was a little careless about following the proper procedures."
You explain that you are giving immune globulin to contacts of all the cases.

As the image below indicates, once an individual becomes infected with hepatitis A, they begin shedding the virus into their stool 1 to 2 weeks before the onset of symptoms and for at least a week after the onset of illness.
This means that there is about a three week period during which an infected person may transmit the virus to others if proper precautions are not followed.

James says that he lives alone, but indicates that he had sexual contact with Anna B. during that period of time. James also tells you that Anna works in the kitchen at Murphy's Restaurant.

Source: https://whatnowatlanta.com/murphys-peasant-bistro-and-other-restaurants-that-failed-june-health-inspections/
Your team decides to go to Murphy's first thing in the morning to conduct an inspection and talk with Anna B.
The next morning you and Christine go to Murphy's and meet with Denise, the manager. Christine explains that there is a possibility that a food handler had been infected with Hepatitis A and subsequently contaminated some food product that made customers ill.
Christine Meets the Manager (0:23)
The Inspection (6:03)
Summary for the Manager (2:20)
Important Points for Inspection
Christine emphasized that the purpose of the inspection was to assess recent employee health, food storage and handling, and employee hand-washing practices and other related items on the inspection checklist. She made a point of assuring the manager that this was part of an on-going investigation and that no statements were being made to the press or the general public about the inspection at this time. The manager was willing to answer the inspector's questions and show her the facility.
MA Inspection Report and Checklist
MA Sanitary Code for Food Establishments

MA Inspection Report and Checklist

When you interviewed Anna B., she admitted that she had had mild diarrhea for a couple of days last week and had felt a little more tired than usual, but she didn't have any nausea, vomiting, or fever. She only gets paid for the hours she works, so she didn't report her illness to her supervisor.
You now have the results of Anna's blood tests. Her liver function tests are somewhat elevated, and she tested positive for IgM anti-HAV, indicating that she has newly acquired hepatitis A, although she had minimal symptoms.
Anna was also the foodhandler who you found preparing a sandwich with her bare hands, and she admits, "I don't always wash my hands real well if we get busy." Today is May 20. The epidemic has been dwindling, but Anna appears to be one of the last cases to have acquired hepatitis from James R.

This new information raises the question of what to do about people who may have been recently exposed to hepatitis A but do not yet have symptoms. In order to make a decisions about this, you should first review this module page on active and passive immunity. Pay particular attention to the CDC guidelines for post-exposure prophylaxis for hepatitis A.
The Decision to Give Immune Globulin
The decision to give immune globulin to all of the personal contacts and all of the patrons who may have been exposed to an infected food handler should not be taken lightly. Organizing an IG clinic is difficult, time consuming, very costly, and consumes large quantities of immune globulin, which is a precious resource. The decision depends on a judgment regarding the likelihood of exposure to patrons.
If you were convinced that Anna B. followed proper food handling and hygienic procedures, an IG clinic would not be justified, even if she were infected. However, since Anna B. did not follow procedures, the results of her blood tests are important in decision making. Since she was positive for IgM anti-HAV (indicating that she had hepatitis), an IG clinic is clearly warranted, but if her blood tests had been negative, an Ig clinic would not be necessary.
The results of her blood tests are important to decision making here, but what if she had refused give a blood sample? She can't be forced to provide a blood specimen, but she can be excluded from work. The course of action is critically dependent on an assessment of whether the situation presents an "imminent health hazard."
Alfred DeMaria, Jr., MD
Chief Medical Officer and State Epidemiologist,
Massachusetts Department of Public Health
(1:12)
Christine Connolly's comments. (1:50)
News clip on a local IG clinic. (1:24)
Al DeMaria's comments. (1:02)
Alan Balsam's thoughts. (3:47)
The CDC has clear cut guidelines on post-exposure prophylaxis in people who may have been exposed to hepatitis A.
So, who makes the decision about whether to conduct an Ig clinic or not? Is the local board, the state DPH, or the CDC? Listen to these two short clips in which Dr. DeMaria discusses the relationship between the state and local departments of public health. (1:23, 0:41)
Congratulations on successfully concluding the Sparta outbreak. This module was based on a real outbreak of hepatitis A, although details were changed to focus on specific learning objectives.
One of the important aspects of this case is that it illustrates that solving public health problems requires skills from multiple disciplines.
In summary, dealing with this problem required skills and concepts from multiple disciplines. (2:10)