A Brief History of Public Health
Note: We are continually trying to improve the accessibility and usability of our learning modules. Please forward comments and suggestions to wlamorte@bu.edu.
Link to Contents
After completing this module, the student will be able to:
Note: words in bold can be scrolled over to provide a definition.
Ten thousand years ago humans were hunter-gatherers. They had a short life span, but not because of epidemics; their primary problem was just finding enough food to eat. They lived and traveled in small groups and hunted and foraged for food. Their mixed diet was probably fairly balanced and nutritionally complete. Since they lived in small groups and moved frequently, they had few problems with accumulating waste or contaminated water or food.
Early explanations for the occurrence of disease focused on superstition, myths, and religion. Primitive peoples believed in natural spirits that were sometimes mischievous or vengeful. The Greeks believed that the god Jupiter was angry about man accepting the gift of fire. The story is long and complicated, but Zeus crammed all the diseases, sorrows, vices, and crimes that afflict humanity into a box and gave it to Epimetheus, the husband of Pandora. Mercury was very tired from carrying his burden and gave it to Epimetheus for safe keeping. Pandora wanted desperately to know what was in the box. She waited until Epimetheus was gone. She opened the box, and all of the ills of the world flew out and spread throughout the human world.
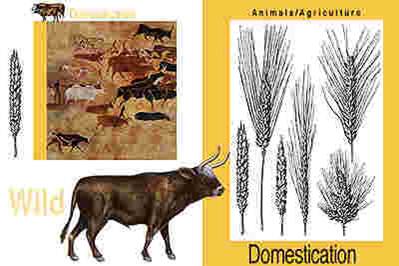
The shift from the hunter-gather mode of living to an agricultural model provided a more secure supply of food and enabled expansion of the population. However, domesticated animals provided not only food and labor; they also carried diseases that could be transmitted to humans. People also began to rely heavily on one or two crops, so their diets were often lacking in protein, minerals, and vitamins. People began living in larger groups and staying in the same place, so there was more opportunity for transmission of diseases.
Garbage and waste accumulated, and rodents and insect vectors were attracted to human settlements, providing sources of disease. The engraving above on the right above shows a woman emptying her bedpan into the street of a medieval village.
For many centuries explanations for disease were based not on science, but on religion, superstition, and myth.
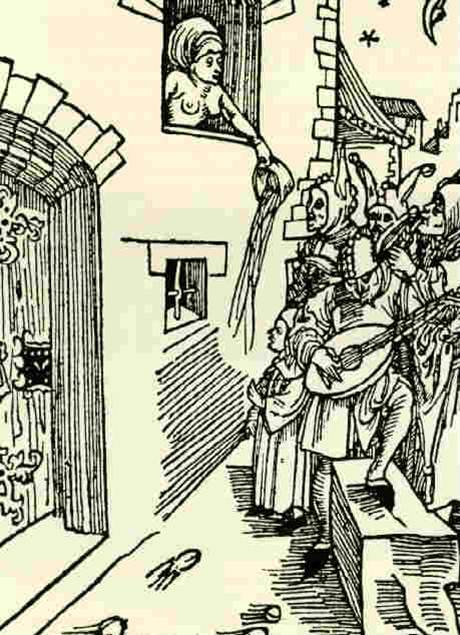
The Hippocratic Corpus was an early attempt to think about diseases, not as punishment from the gods, but as an imbalance of man with the environment. Although it was unsophisticated by today's standards, it was an important step forward. By considering the possibility that disease was associated with environmental factors or imbalances in diet or personal behaviors, the Corpus also opened up the possibility of intervening to prevent disease or treat it.
The Corpus looked at disease as an imbalance in natural forces or an imbalance in humours (or fluids): melancholy, phlegm, bile, and blood. Health depended on a proper balance of these humours. While crude, this concept of humours provided some sort of rationale for understanding health and disease. Greek physicians prescribed changes in diet or lifestyle and sometimes concocted drugs or performed surgery. An excess of the humour blood, for example, became the rationale for bloodletting, a practice that was followed for centuries (without any evidence of its efficacy).
Despite the contributions of the Corpus, medical and scientific progress in Europe was arrested for several centuries. The population grew, and cities became densely populated, but there was little attention to waste disposal and sanitation. These factors set the stage for endemic disease and periodic epidemics.
Bubonic plague is an acute infectious disease caused by the bacterium Yersinia pestis. The bacteria live in the intestines of fleas and are transmitted to rats by flea bites. The rats, therefore, serve as a natural reservoir for the disease, and fleas are the vectors. Occasionally, an infected flea would jump to a human and introduce the bacteria when a blood meal was taken. The bacteria would then spread to the regional lymph nodes and multiply, causing dark, tender, swollen nodules (buboes), as shown below in a boy a walnut-sized swelling in the inner aspect of his upper thigh. As the infection spread, the victim would experience headache, high fever, delirium, and finally death in about 60% of cases.

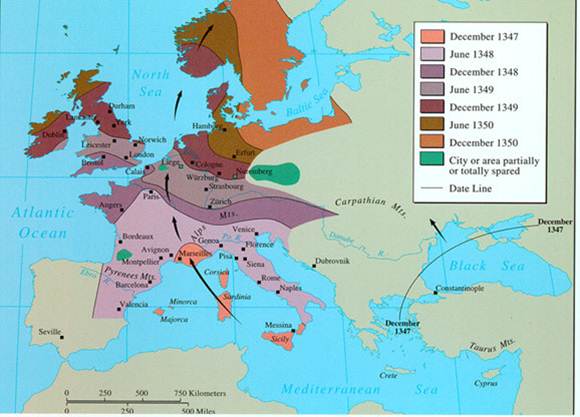
Starting in 1347, Europe experienced multiple waves of bubonic plague epidemics that lasted until the late 1700s. It is believed that the bubonic plague originated in Asia and traveled along trade routes into the Black Sea and then into the Mediterranean Sea. From there, it swept through Sicily and Italy and then up through France and the northern European countries all the way up into Scandinavia. There were many subsequent waves of plague that swept through Europe until the late 1700s. The map below shows the spread of plague over a three year period from Asia across the Black Sea into the Mediterranean and then through Italy, France, England, Northern Europe, and into Scandanavia.
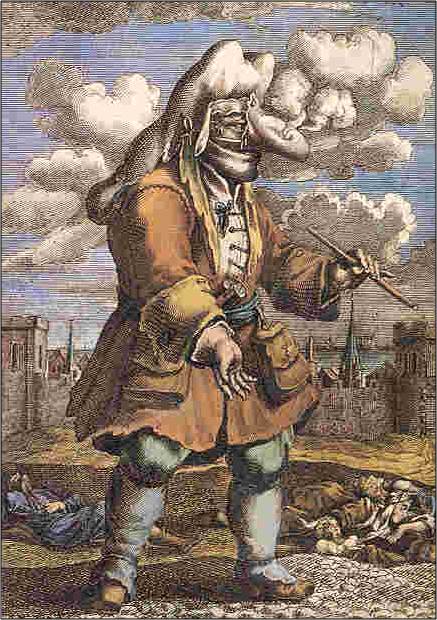
The cause of the plague was not known, but there were many theories. The most popular explanation was that it was caused by "miasmas," invisible vapors that emanated from swamps or cesspools and floated around in the air, where they could be inhaled. Others thought it was spread by person to person contact, or perhaps by too much sun exposure, or by intentional poisoning. The miasma theory was the most popular, however. One of the popes kept large fires burning at both ends of the room he worked in order to counteract the miasmas. The illustration on the left shows a "plague doctor," who is covered from head to toe, including a hood, a mask, gloves, and a beak-like sack on his nose. The covering on the nose contained aromatic herbs, which were believed to neutralize miasmas.
There were also crude medicines that were concocted to prevent or cure the bubonic plague; one of them was known as theriac. Of course, smoke and aromatic herbs and theriac were ineffective, because the plague was primarily spread by flea bites (although sometimes victims developed a plague pneumonia that caused them to cough up a bloody, plague-filled aerosol that could be transmitted to others by inhalation; this was the 'pneumonic' form of the plague). The below shows one of the "plague doctors" who were clothed from head to toe (including hood and mask) in order to protect themselves from the miasmas that spread plague.
While most believed that plague was caused by miasmas, the primary mode of transmission was actually via flea bites, and, in a sense, the real causes were increased population density and failure to dispose of garbage. Accumulations of garbage attracted rats and enabled the rat population to explode. Rats had harbored fleas and Yersinia pestis for many years without major difficulty, and plague epidemics in humans didn't occur until human behaviors created environments that brought people into proximity with rats, fleas, and Yersina pestis. These were the real causes of the plague epidemics.
At first glance one might blame the lack of understanding about transmission and the ineffective preventive measures on the primitive level of scientific understanding. However, the inability to identify the cause and the inability to identify effective control measures was not due to a lack of sophisticated technology. Instead, it was primarily due to the fact that humans had not yet developed a structured way to think about the determinants of disease. There were certainly theories of how the plague spread and these led to preventive strategies, but none of the theories or preventive strategies or treatments were ever tested by collecting observations in groups of people. The idea of studying groups of people to test associations between "risk factors" and disease outcomes had not yet evolved.
|
Key Concept: The lack of a systematic way of testing possible associations between exposures and outcomes ("risk factors" and disease) was the major factor that prevented advances in understanding the causes of disease and the development of effective strategies to prevent or treat disease. |
The use of quarantine as a public health measure dates back to the 14th century when the Black Death ravaged Italy and the rest of Europe. Quarantine comes from the Italian quarantena, meaning forty-day period. Travelers and merchandise that had potentially been exposed to disease were isolated for a period of time to ensure that they weren't infected. Some cities and towns would create a "cordon sanitaire,' a physical barrier that could only be crossed with permission. This practice persisted into the late 19th century and early 20th century. When plague threatened San Francisco, the Chinese section was quarantined by encircling it with a rope with armed guards to ensure that unauthorized individuals did not pass through. a "cordon sanitaire" was also used during an outbreak of bubonic plague in 1899-1900 in Honolulu's Chinatown. Fourteen blocks of the city were literally cordoned off, isolation 10,000 people..

While quarantine is one of the oldest public health measures, it is still useful today. During the SARS epidemic, Toronto quarantined individuals who had potentially been exposed by confining them to their homes until it was certain that they weren't infected. This measure was effective in controlling SARS because individuals infected with SARS were not infectious until they began to exhibit symptoms. Consequently, if an individual was possibly exposed, but did not yet show symptoms, quarantine prevented them from infecting others. However, quarantine is less useful for diseases like influenza, when an infected person can spread the disease even before they begin having symptoms. Quarantine is different from isolation, which is separation of a person who has the disease; quarantine refers to the separation of an individual who has possibly been exposed to disease.
Video: The Past, Present and Future of the Bubonic Plague - Sharon N. DeWitte (from www.TED.com)
Systematic thinking about how to establish the determinants of health and disease was not suddenly invented by a single individual. It evolved over centuries. One can see sparks of insight intermittently over time. In the 1700s and 1800s one can see attempts to examine the causes of disease and the effectiveness of prevention and treatment in a systematic way. This page provides an interesting, but incomplete assortment of examples illustrating some of the major ideas that emerged and contributed to the evolution of how we investigate the factors associated with health and disease and establish the determinants.
Girolamo Fracastoro (shown below) was an Italian physician, poet, astronomer, and geologist, who wrote about 'disease seeds' carried by wind or direct contact. In essence, he was proposing the germ theory of disease more than 300 years before its formal articulation by Louis Pasteur and Robert Koch.

In 1546, Fracastoro outlined his concept of epidemic diseases in "De contagione et contagiosis morbis" and speculated that each disease was caused by a different type of rapidly multiplying 'seed' and that these could be transmitted by direct contact, through the air, or on contaminated clothing and linens. Similar speculation had been mentioned as a possible cause of disease by the Roman scholar Marcus Varro in the 1st century BC.
It was once believed that life forms could arise spontaneously. Maggots, worms, & bacterial and fungal growth could be found "arising" from food that was left to stand. In 1699 Francesco Redi boiled broth and sealed it; no growth occurred, suggesting that Fracastoro was correct.
Beginning around 1592 the parish clerks in London began recording deaths. In 1662 John Graunt, a founding member of the Royal Society of London, summarized the data from these "Bills of Mortality" in a publication entitled "Natural and Political Observations Mentioned in a Following Index, and Made Upon the Bills of Mortality."
Graunt analyzed the data extensively and made a number of observations regarding common causes of death, higher death rates in men, seasonal variation in death rates, and the fact that some diseases had relatively constant death rates, while others varied considerably. Graunt also estimated population size and rates of population growth, and he was the first to construct a "life table" in order to address the issue of survival from the time of birth.
Van Leeuwenhouk's accomplishments were preceded by those of Robert Hooke, who had published "Micrographia" in 1665. Hooke devised a compound microscope and used it to examine and describe the structure of nature on a microscopic level, including insects, feathers, and plants. In fact, it was Hooke who discovered plant cells and coined the term "cells".
Anton van Leeuwenhoek of Holland was "the father of microscopy." He began as an apprentice in a dry goods store where magnifying glasses were used to inspect the quality of cloth. Van Leeuwenhoek was fascinated by the lenses and experimented with new methods for grinding and polishing more powerful lenses.

He was able to achieve magnifications up to 270x diameters. He used these to create the first useful microscopes. Using his inventions, he was the first to see bacteria (1674), yeast, protozoa, sperm cells, and red blood cells.
John Pringle was a Scot who served as physician general to the British forces during the War of the Austrian Succession (1740–48). In London he became physician to the Duke of Cumberland and to King George III. Pringle published "Observations on the Diseases of the Army" in 1752, in which he proposed a number of measures aimed at improving the health of soldiers including improvements in hospital ventilation and camp sanitation, proper drainage, adequate latrines, and the avoidance of marshes.
He wrote expensively on the importance of hygiene to prevent typhus or "jail fever," which was a common malady among soldiers and prisoners in jails. Pringle incorrectly believed that typhus was caused by filth. In fact, it is caused by a small bacterium (a rickettsia). Lice are vectors for the disease; when infected lice defecate on the skin of lice-infested soldiers or prisoners, the bacteria can gain entry through small scratches or abrasions in the skin. The bacteria then multiply and cause a severe febrile illness which is often fatal if not treated. Pringle also coined the term 'influenza'.
Scurvy is due to a deficiency in vitamin C that results in weak connective tissue and abnormally fragile capillaries that rupture easily, causing bleeding, anemia, edema, jaundice, heart failure, and death. Scurvy was a huge problem in sailors several centuries ago, because of the chronic lack of fresh fruit and vegetables during long sea voyages. James Lind, a Scottish naval surgeon, suspected that citrus fruits could prevent it based on some anecdotal observations. In 1754 Lind conducted what may be the world's first controlled clinical trial on 12 sailors with scurvy.
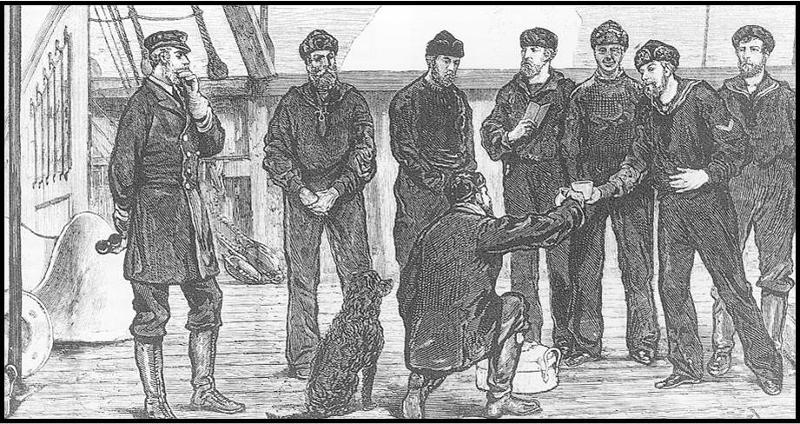
Lind divided the 12 sailors into pairs, and each group received a different treatment (sea water, various other concoctions, and lemons and oranges. The two who received lemons and organs were cured, but the others were not. Lind concluded that his hypothesis was correct, reported his findings, and recommended that sailors receive a ration of lime or lemon juice.
Unfortunately, 50 years passed before the British navy acted on Lind's recommendations and began to provide lime juice to sailors at sea. (This led to the nickname "Limeys" for British sailors.) It is also noteworthy that Lind was able to correctly identify a means of preventing scurvy even though he misunderstood the cause. He believed toxins within the body were normally released through pores in the skin and that scurvy was the result of damp sea air causing pores to close, thus trapping toxins within the body.
Bloodletting to Treat Cholera
Francois Broussais was a prominent Parisian physician and a strong proponent of bloodletting with leeches. He used bloodletting to treat many diseases, including cholera. In the engraving below Broussais can be seen instructing a nursing sister to continue to apply leeches to his patient (who is already quite pale from loss of blood). It is believed that his vigorous use of bloodletting to treat victims of a cholera epidemic in Paris substantially contributed to the mortality rate. The image below on the left is an engraving showing Broussais telling a nursing sister to continue bleeding has patient.
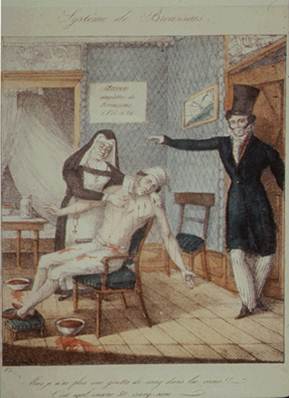
Pierre Louis was a contemporary of Broussais's who believed in using numerical methods to evaluate treatment. Louis studied bloodletting and found it ineffective, but many dismissed his conclusions. Bloodletting was a therapy that had been practiced for centuries, although it had never been tested for efficacy. It had become embedded in medical practice.
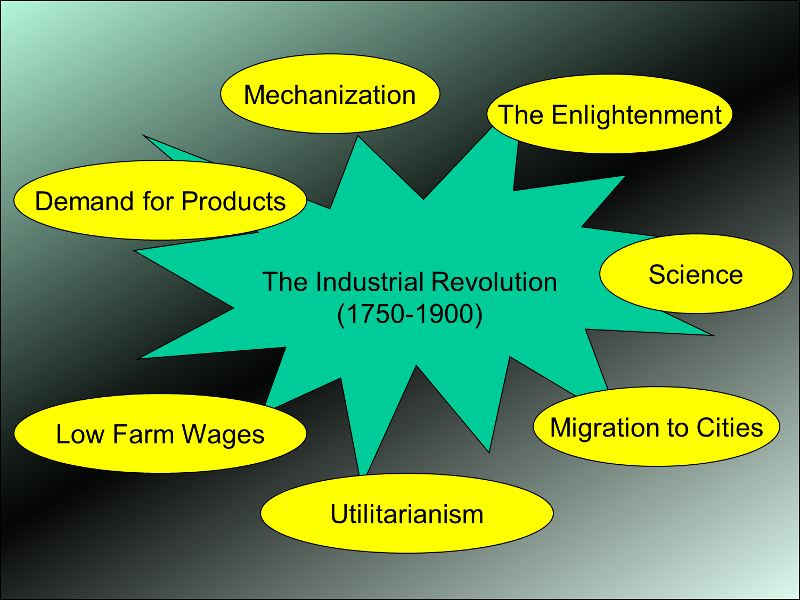
The Industrial Revolution brought an explosion of development. There were new jobs, (particularly in the cities), new goods, and increased trade. However, it also brought new problems to Europe.
Further expansion of the population and mass migration caused explosive growth of cities. The maps to the right illustrate the concentration of population into the cities of England that occurred over 200 years beginning in 1700 as shown in these maps of population density in 1701 and 1911.
Poor workers were often housed in cramped, grossly inadequate quarters. Working conditions were difficult and exposed employees to many risks and dangers, including cramped work areas with poor ventilation, trauma from machinery, toxic exposures to heavy metals, dust, and solvents. Consequently, progress brought a whole new set of health problems that were widespread in Europe and in America.
Click on the"Photo Album" below to see a brief summary of living conditions in England during the 1800s.
The Enlightenment was a period that saw an embrace of democracy, citizenship, reason, rationality, and the social value of intelligence (the value of information gathering). These ideas provided important underpinnings for public health. In the early 1800s Jeremy Bentham (pictured on the right) and his disciples (the theoretical radicals) developed the philosophy of utilitarianism which provided a theoretic underpinning for health policy and wider social policies.
One theme was that the reduction of mortality and improvements in health had an economic value to society. Healthy workers were more able to contribute to the economy of the state. Implicit in utilitarianism was the notion that one could measure 'evil' by the degree of misery that was created (or relieved) by a particular action. To Bentham the welfare of both the wealthy and the poor could be achieved most efficiently with good governmen
Ignaz Semmelweis was a Hungarian physician who practiced in the maternity department of the Vienna General Hospital in the 1840s. Postpartum sepsis (puerperal fever) was a common occurrence and was almost invariably fatal. There were two maternity wards in the hospital, one where births were attended by medical students, and another where births were attended by midwives. The students often came directly from the dissecting rooms where they had been working with corpses with their bare hands. Puerperal fever was much more common in the ward tended by the medical students, but no one knew why.
A colleague of Semmelweis cut his hand while performing an autopsy and developed a similar clinical picture of overwhelming sepsis and died. Semmelweis began to wonder whether contagion could be carried on the hands and transferred to the women during childbirth.
He decided to require all attendants to wash their hands in chlorinated lime water before attending to a birth, and the rate of infection plummeted. Some were impressed by these findings, but others, including Semmelweis's superior, ignored them.
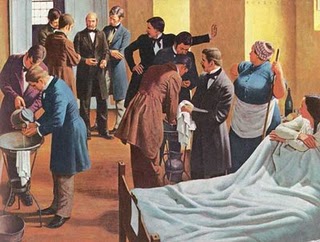
Oliver Wendell Holmes, Sr. was an American physician, professor, lecturer, and respected literary author. He received his M.D. from Harvard Medical School in 1836 and served as professor and chairman of anatomy and physiology at Dartmouth Medical School and later at Harvard Medical School. He advocated for medical reforms and was a strong proponent of the idea that doctors and nurses could carry puerperal fever from patient to patient. In 1843 he presented a paper entitled "The Contagiousness Of Puerperal Fever" at the Boston Society for Medical Improvement (see engraving below).
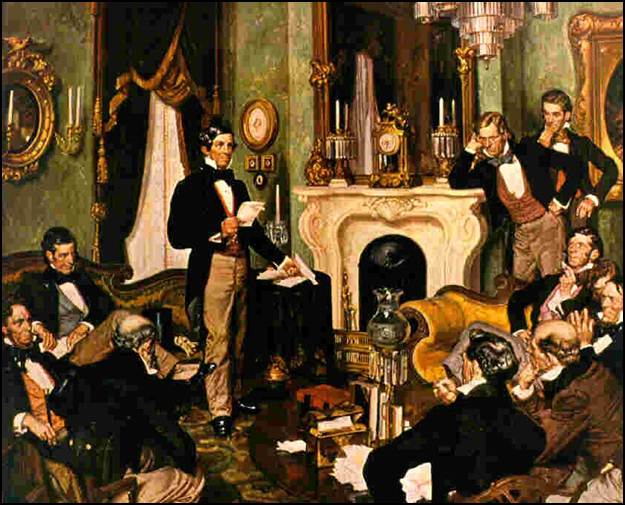
This was a controversial position. Holmes was opposed by a number of members of the society, including Dr. Charles Meigs, a prominent obstetrician. With regard to puerperal fever, Meigs's position was:
"I prefer to attribute them to accident, or Providence, of which I can form a conception, rather than to a contagion of which I cannot form any clear idea, at least as to this particular malady." (Quote from Professor Charles D. Meigs)
Cholera is an infectious disease that became a major threat to health during the 1800s. The story has been elegantly told in The Ghost Map by Steven Johnson, who describes the conditions in London in the 1800s situation in the brief video below.
Cholera continues to be a problem throughout the world today (see Cholera in Haiti). The next video describes the cholera epidemic in Haiti in 2010.
In the 1800s there were large epidemics of cholera in Europe and America that killed thousands of people. John Snow (shown below) was a physician in London who spent several decades studying cholera in a systematic way. He is most often credited with solving an outbreak of cholera that occurred in London in 1854 (the outbreak is described below), but his studies of cholera were much more extensive than that. The first cholera epidemic in London struck in 1831, when Snow was still an apprentice. Another large epidemic occurred in 1848 and lasted through 1849.
The prevailing opinion was that cholera was spread either by miasmas or by person-to-person contact, Snow began examining the victims and found that their initial symptoms were always related to the gastrointestinal tract. Snow reasoned that, if cholera was spread by bad air, it should cause pulmonary symptoms, but since the symptoms were gastrointestinal, perhaps it was transmitted by water or food consumption. In fact, cholera is caused by the bacterium, Vibrio cholera, which is transmitted by the fecal-oral route, that is by ingestion of water or food that is contaminated with sewage.
In August 1849 Snow published a paper entitled "On the Mode of Communication of Cholera" in which he presented his theory that the disease was acquired by ingestion of contaminated water, but his theory did not get much traction with the medical establishment. The epidemic ended in 1849, but Snow continued to collect data on the pattern of of disease and began finding evidence that linked cholera to specific sources of water.
Many Londoners received their water from hand pump wells (below) that were located throughout the city.

However, increasing numbers of businesses and homes had water piped from the Thames River by private companies. Snow learned from municipal records that two private companies supplied piped in water to the areas that were primarily affected by cholera. Some consumers were supplied by the Lambeth Company, while others were supplied by Southwark & Vauxhall. The map of London below shows the areas of London supplied by these two water companies.
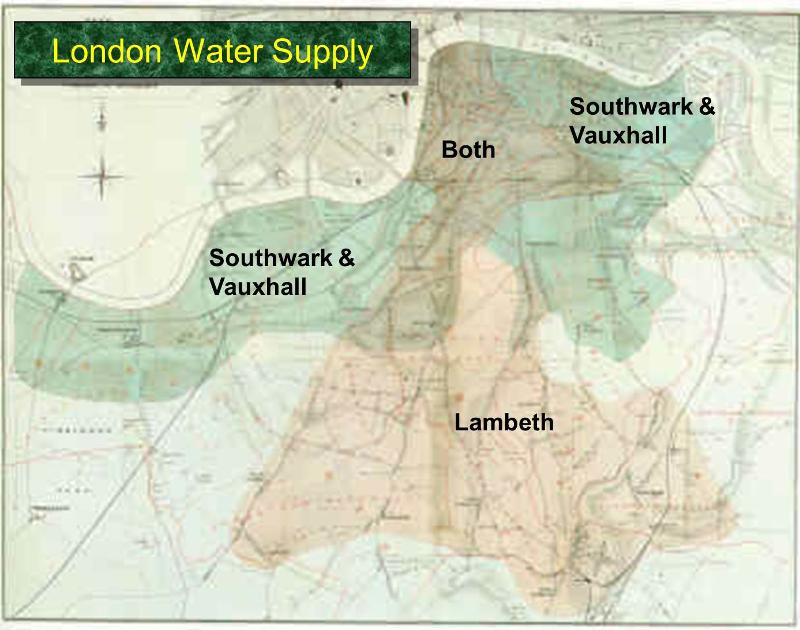
Southwark & Vauxhall pumped water from a more downstream location that was clearly contaminated, and the rates of cholera were clearly higher in their customers compared to those supplied by the Lambeth Company. Nevertheless, many were unconvinced by his findings, since Snow had not actually demonstrated that the water contained something that could cause cholera.
|
Water Company |
# Houses Served |
# Cholera Deaths |
Death Rate per10,000 Houses |
|---|---|---|---|
|
Southwark & Vauxhal |
40,046 |
1,263 |
315 |
|
Lambeth |
28,107 |
98 |
37 |
|
The rest of London |
256,423 |
1,422 |
59 |
In late August of 1853, cholera broke out in the Broad Street area, and the residents panicked and many began to flee. A hand pump was located right on Broad Street, and Snow was immediately suspicious. Water samples did not reveal gross contamination, but Snow persisted and began to collect detailed information on where the victims had gotten their drinking water. He obtained the names and the addresses of the first 83 victims who had died by the end of the first week. He went to their homes and learned from relatives that the vast majority of them had obtained their water from the Broad St. pump.
On Sept. 6 Snow appeared at the meeting of the local Board of Guardians and presented his evidence that the pump was the source of the outbreak. He argued that the pump handle should be removed in order to prevent further contamination. The board was not convinced, but agreed to remove the pump handle as a precaution. The epidemic quickly subsided.
The investigation continued. Ultimately, Snow was able to track down 197 victims, the vast majority of whom lived within walking distance of the pump. It was also noted that there was an extremely low incidence of cholera at a nearby work house and also at the Lion Brewery, and both of these businesses had their own water supply. The workers at another large business used water from the Broad St. pump, and their workers had a substantial incidence of cholera.
The map below shows the location of the pump, and the home or business location of the victims is shown by stacks of small dark marks that are clearly clustered around the pump. This type of map, which marks the location of disease cases, is now referred to as a "spot map."
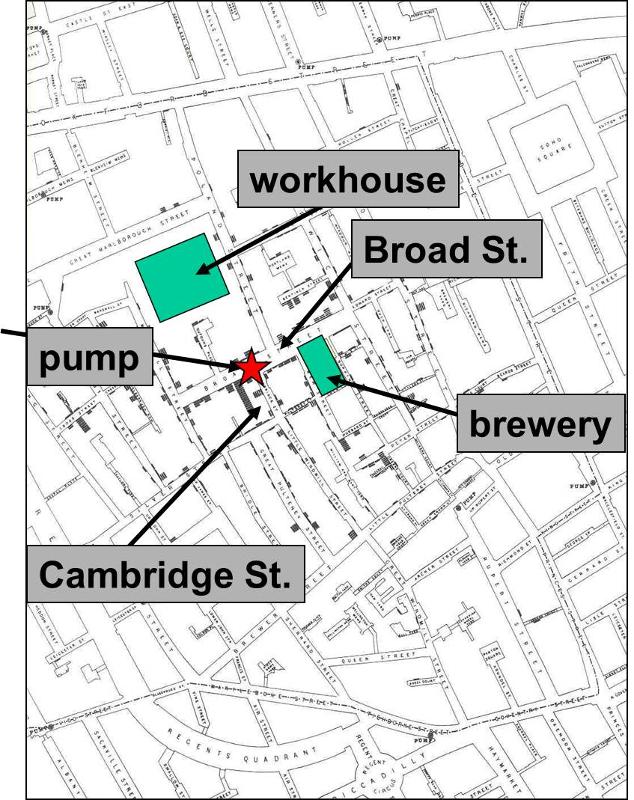
An initial examination of the well failed to show any problems, casting doubt on Snow's conclusions, and the pump was reopened without incident. However, some months later an associate of Snow's stumbled upon the records of an infant who had died of diarrhea at the very beginning of the outbreak. The timing of her death indicated that she had been the first cholera case. Upon questioning, the mother said that she had emptied a pail of the infant's diarrhea into a cesspool in front of their house immediately adjacent to the water pump. The cesspool and the pump well were than excavated, revealing that the cesspool, which was within three feet of the well, was leaking, and the wall of the well was decayed, allowing the contamination from the cesspool to seep in. In retrospect, it appeared that once the child died, there was no further contamination of the well, and the epidemic ended.
This graph shows the number of cholera deaths over time. There is an abrupt increase in cholera deaths at the very end of August. Deaths peak on September 2, when there were about 130 deaths, and the cholera death rate gradually declines to near zero over the next three weeks.
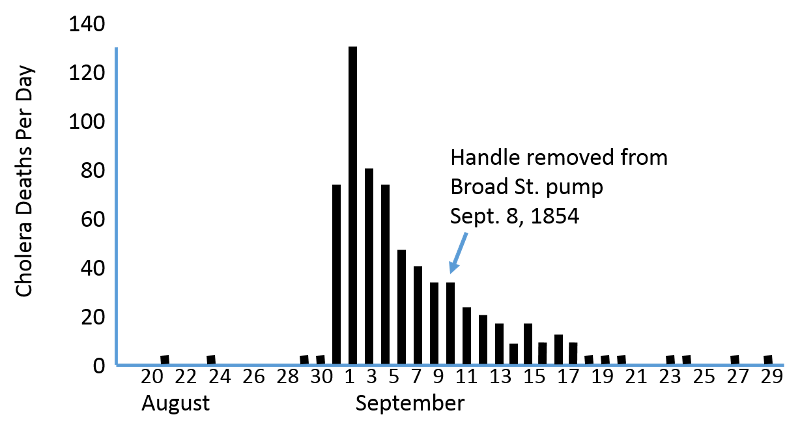
With knowledge of the incubation period for the disease, the shape of an epidemic curve can sometimes provide clues regarding the source of the epidemic. Cholera has an incubation period of only 1-3 days, and this graph indicates that new cases occurred over a period of about 10 days. This suggests a "continuous source" epidemic, because new cases continue to occur for more than one incubation period, suggesting an ongoing source of contamination.. period.
In retrospect, Snow made several important contributions to the development of epidemiologic thinking:
In many respects, public health as we think of it today (i.e., as a function of good government) took shape in London and Paris in the wake of the devastating health consequences of the Industrial Revolution. However, the circumstances that propelled the development of public health as a discipline are more complex with many contributing factors. First, there was the notion of the importance of the monarchy and the power of the state. The influence and power of the state could be assessed in many ways including commerce and trade, but also by the size of the population and the health and fitness of the working population.
This crude notion made the work of John Graunt quite compelling, and the importance attached to "numbering the people" grew. Not surprisingly, the General Registrar's Office was established in 1837 to record compulsory registration of births, deaths, and marriages in England and Wales. Dr. William Farr (below) was appointed Chief Statistician; Farr had trained at the Royal Academy of Medicine in Paris. The General Registrar's Office established the importance of surveillance with respect to health.

A second factor was the emergence of the Enlightenment in the 18th century, which embraced democracy, citizenship, reason, rationality, and the social value of intelligence (the value of information gathering). These ideas provided important underpinnings for public health. In the early 1800s, Jeremy Bentham and his disciples (the theoretical radicals) developed the philosophy of utilitarianism which provided a theoretic underpinning for health policy and wider social policies. One theme was that the reduction of mortality and improvements in health had an economic value to society. Healthy workers were more able to contribute to the economy of the state. Implicit in utilitarianism was the notion that one could measure 'evil' by the degree of misery that was created (or relieved) by a particular action. To Bentham the welfare of both the wealthy and the poor could be achieved most efficiently with good government.
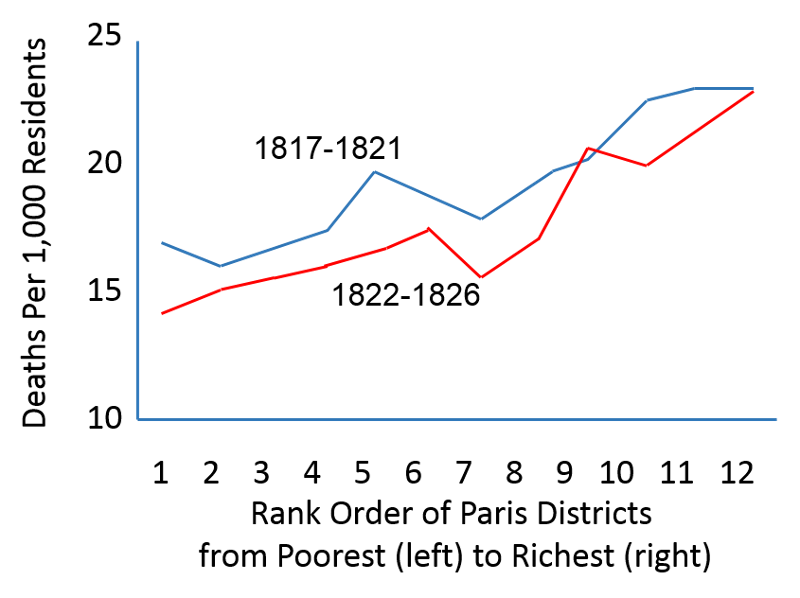
Yet another factor was the recognition that poor health was a burden that fell disproportionately on the poor. Villerme, a physician in Paris had noticed that mortality rates varied widely among the districts (arrondissement) of Paris. He tried to correlate mortality with the distance of the arrondissement from the Seine River, the relationship of the streets to the prevailing winds, the arrondissement's source of water and local climatological factors such as soil type, exposure to the sun, elevation and inclination of the arrondissement. None of these things correlated. However, when he used tax rates as an indicator of wealth, Villerme found a striking correlation with mortality rates.
The graph below shows the correlation between poverty and mortality rates among different districts (arrondissements) in Paris found by Villerme. This relationship has persisted for centuries, and it is a powerful predictor of health.
In 1842 Sir Edwin Chadwick, a social reformer, published a report entitled the 'Report into the Sanitary Conditions of the Labouring Population of Great Britain' proving that life expectancy was much lower in towns than in the countryside.

Chadwick argued that it was possible for the government to improve people's lives through reform; he believed that a healthier population would be able to work harder and would cost less to support. He concluded that what was really needed was not more physicians, but civil engineers to provide drainage of streets and to devise more efficient ways of delivering clean water and removing sewage and other noxious substances. These social, economic, political, and philosophical developments all contributed to the emerging idea that the public's health was a legitimate interest of government.
It is interesting to note that many of the proponents of the "Sanitary Idea," including Edwin Chadwick (shown on the right), were "miasmatists" who clung to the belief that disease was caused by breathing foul vapors. Since sewage and garbage smelled bad, they were associated with disease, so the miasmatists pushed to clean up the environment. And despite the fact that their belief in miasmas would prove to be incorrect, the end result was that many of the sources of infectious disease were removed. Chadwick was instrumental in creating a central public health administration that paved the way for drainage, sewers, garbage disposal, regulation of housing, and regulations regarding nuisances and offensive trades. This "sanitary idea" resulted in remarkable improvements in health and well-being, as illustrated in the graph below, which shows a remarkable decline in mortality from tuberculosis from the mid-19th century until the mid-20th century.
Chadwick's report provided momentum for the establishment of a number of societies and pressure groups consisting of politicians, civil servants, & social reformers lobbied parliament. Among others, these included:
Through their efforts landmark legislation was passed including:
These efforts had an enormous impact. The graph below shows the remarkable decline in mortality from tuberculosis in the United Kingdom from 1850 to 1960.The remarkable decline in mortality from TB and other infectious diseases is believed to have been the result of the many environmental improvements that occurred as a result of the implementation of the "Sanitary Idea." Note the temporary up-surge in TB death rates during the World Wars I & II, when nutrition suffered and many were forced to live in cramped, poorly ventilated quarters.
Louis Pasteur was a French biologist and chemist who made enormous contributions to germ theory, to prevention of food spoilage, and to the control of disease. In 1853 Pasteur began studying fermentation in wine and beer and rapidly concluded that microorganisms were responsible. He also discovered that microbes in milk could be killed by heating to about 130 degrees Fahrenheit, a process which is now known as 'pasteurization'. He discovered that some microorganisms require oxygen (aerobic organisms), while others reproduce in the absence of oxygen (anaerobic).
Pasteur pioneered the idea of artificially generating weakened microorganisms as vaccines. Edward Jenner's work had demonstrated the principle with the naturally occurring cowpox, which could be used to vaccinate against smallpox. Pasteur was able to artificially weaken strains of anthrax and cholera in order to generate vaccines. It was, in fact, Pasteur who coined the term 'vaccine' in honor of Jenner's discovery. Pasteur developed vaccines against anthrax in sheep and cholera in chickens. In 1885 he developed a vaccine for rabies by growing it in rabbits and then drying the nerve tissue that had been infected with the virus. This vaccine was successfully used to save the life of a boy who had been bitten by a rabid dog.
Events in the US paralleled those in the United Kingdom. The US also underwent a rapid transition from a rural, agricultural society to one that was intensely urban and industrial. Inventions such as the cotton gin that promoted agricultural production, but also decreased the need for farm workers, driving many to the cities for work. Economic growth and inventions spawned factories and textile mills in US cities.
[Note: Many of the facts and images below were gleaned from the US National Library of Medicine's web pages on The History of the Public Health Service.]

From from the US National Library of Medicine's web pages on The History of the Public Health Service:
"The 1870 reorganization [of the Marine Hospital Service] also changed the general character of the Service. It became national in scope and military in outlook and organization. Medical officers, called surgeons, were required to pass entrance examinations and wear uniforms. In 1889, when the Commissioned Corps was formally recognized by legislative action, the medical officers were given titles and pay corresponding to Army and Navy grades. Physicians who passed the examinations were appointed to the general service, rather than to a particular hospital, and were assigned wherever needed. The goal was to create a professional, mobile, health corps, free as possible from political favoritism and patronage, and able to deal with the new health needs of a rapidly growing and industrializing nation."
Epidemics of contagious diseases, such as small pox, yellow fever, and cholera, had devastating effects throughout the 19th century. They killed many people, spread panic and fear, disrupted government, and caused Congress to enact laws to stop their importation and spread. As a result of these new laws, the functions of the MHS were expanded greatly beyond the medical relief of the sick seamen to include the supervision of national quarantine (ship inspection and disinfection), the medical inspection of immigrants, the prevention of interstate spread of disease, and general investigations in the field of public health, such as that of yellow fever epidemics."
The video below is a segment from a PBS documentary on public health. This particular segment focuses on events at the dawn of the 20th century when bubonic plague threatened San Francisco. Note the futile and inappropriate use of quarantine to deal with the threat of plague. The last section of the clip describes a broad array of public health interventions that eventually emerged.
Link to transcript of the video

From from the US National Library of Medicine's web pages on The History of the Public Health Service:
"The working environment and its effect on worker's health became a major area of study for the Public Health Service starting in 1910. Investigations in the garment making industry, as illustrated by these women making flowers, revealed unsanitary conditions and an excessive rate of tuberculosis. Other studies were done of silicosis among miners, sanitation and working conditions in the steel industry, lead poisoning in the pottery industry, and radiation hazards in the radium dial painting industry."
In the video below Sir Richard Doll briefly describes the study that he and Bradford Hill conducted in 1948. (R. Doll and A. B. Hill, 'Smoking and carcinoma of the lung: preliminary report', BMJ, 1950, 2.746). The video is a segment of a PBS video on public health.
Link to transcript of the video
From from the US National Library of Medicine's web pages on The History of the Public Health Service:
"Medical discoveries and public health campaigns have almost eliminated deaths from the common diseases of childhood such as measles, diphtheria, scarlet fever, and whooping cough. As a result of these successes nearly 20 years were added to the average life expectancy at birth between 1900 and 1950-from 47 to 67 years."
"As epidemic diseases were brought under control the Public Health Service began to shift its attention to other areas such as cancer, heart disease, health in the workplace, and the impact of environmental problems, such as toxic waste disposal, on health. But the Public Health Service is still called upon to investigate outbreaks of disease such as Legionnaire's, toxic shock syndrome, and now the deadliest epidemic of our age -- AIDS. Much of the work of the early plague fighters and sanitarians is now carried out by the scientists at the Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia."
Image of small boy with polio standing with crutches
In 1920 Charles-Edward A. Winslow defined public health as "the science and art of preventing disease, prolonging life, and promoting physical health and efficiency through organized community efforts for the sanitation of the environment, the control of community infections, the education of the individual in principles of personal hygiene, the organization of medical and nursing service for the early diagnosis and preventive treatment of disease, and the development of the social machinery which will ensure to every individual in the community a standard of living adequate for the maintenance of health." While most would include mental health as an important aspect of public health today, Winslow's definition is still relevant.
Health is dependent on a complex interplay among an array of genetic, environmental, and lifestyle factors. As a result, public health is built on expertise and skills from many areas, including biology, environmental and earth science, sociology, psychology, government, medicine, statistics, communication, and many others. This complexity makes it difficult for the general public to understand exactly what public health is and what it does. In addition, public health has been so successful that some in the general population may not be aware of the expertise and hard work that is required to ensure the health and safety of their community. The life of a person who develops severe heart disease might be prolonged by a dramatic and very expensive medical procedure such as heart surgery. However, public health is about interventions that prevent disease from occurring, so the benefits tend to be less obvious. In addition, prevention of disease both prolongs life and improves the quality of life. In a sense, public health is the heart disease that never developed, the epidemic that didn't happen, the outbreak of foodborne illness that never occurred, the child that would have developed asthma, but didn't. Public health is the disaster that didn't happen.
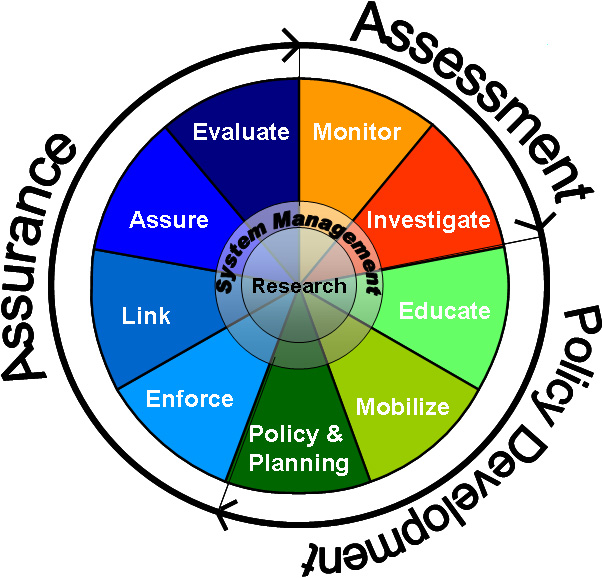
The strategy employed by public health is to:
Centers for Disease Control and Prevention History
Core Functions of Public Health
Public Health Museum in Massachusetts