
Lyme Disease
Contributors
Lyme disease was first discovered in 1975 in Lyme, Connecticut when an increased number of individuals were diagnosed with juvenile rheumatoid arthritis. Samples of their blood, cerebral spinal fluid, and other tissues were evaluated in the lab, and the causal agent was found to be the Borrelia burgdorferi, the causative agent of Lyme disease.
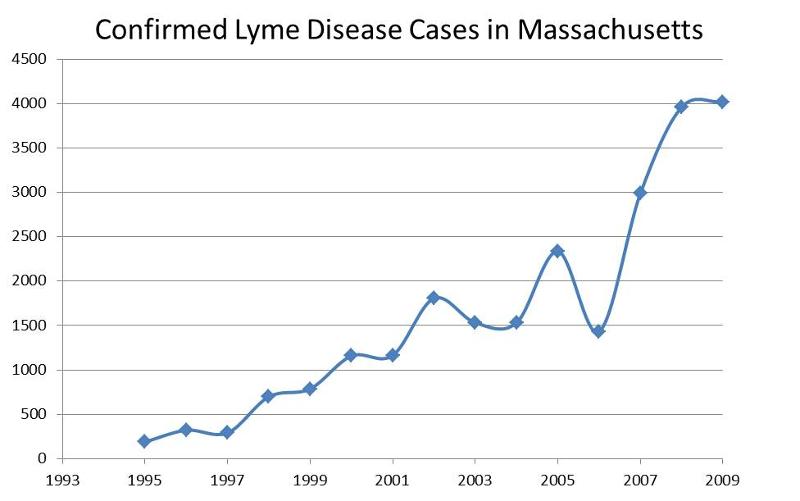
Since then, our understanding of the disease has expanded. It has become an even greater concern over the past few years due to the drastic increase in incidence of the disease. In 2009, CDC estimated over 37,000 probable cases nationwide. In 2009, CDC confirmed over 4,000 cases in Massachusetts alone. The rise in incident cases can be attributed to five main causes:
These high incidence rates are of great concern, and should lead to increased efforts from public health professionals to address the problem. This module serves as a tool in an effort to disseminate knowledge to public health officials regarding Lyme disease in an attempt to counter the problem in our nearby communities.
After successfully completing this module, you will be able to:

Lyme disease is a vector-borne disease caused by transmission of bacteria through a tick bite. Lyme disease is caused by a gram-negative bacterium of the spirochete phylum called Borrelia burgdorferi (see photo to the left below). If a tick bite deposits a sufficient number of the bacteria into a human host's skin, the bacteria replicate in the dermis layer of the host's skin at the site of the tick bite, often causing the appearance of a characteristic "bull's eye rash," also known as erythema migrans (see photo to the right below). If it is not treated promptly, the bacteria can spread to the bloodstream and infect the joints, heart, and central nervous system causing a variety of symptoms and manifestations.
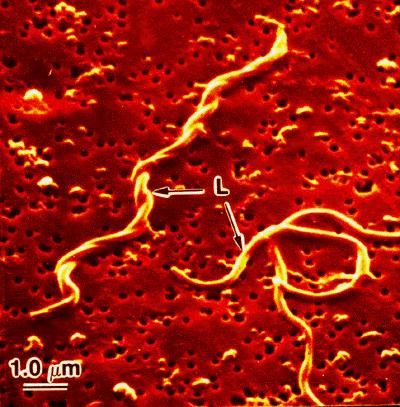
Borrelia burgdorferi
Source: http://borrelia.mlst.net/

Erythema migrans or "bull's eye rash")
Source: http://hardinmd.lib.uiowa.edu/CDC/lymedisease7.html
In 2009 there were 29,959 confirmed and 8,509 probable cases of Lyme disease reported to CDC, for an incidence of 13.4 cases per 100,000 population. During the same year, Massachusetts had 4,019 confirmed and 1,237 probable cases, an incidence of 61.0 per 100,000 population. The annual number of confirmed cases has been rising steadily over the past 15 years.
The incidence of LD is associated with the density of infected tick vectors. Most cases in the U.S. have been reported in the Northeast, the western states, and the upper Midwest, but nearly all states have reported Lyme disease. The US map below is from CDC and based on 2009 data. The Massachusetts map shows Lyme disease incidence rates per 100,000 by town in 2005. Darker shading indicates higher incidence. Lyme disease is considered endemic in the entire state of Massachusetts. Areas of highest incidence include Cape Cod and southeastern Massachusetts, the islands of Nantucket and Martha's Vineyard, areas north of Boston in Essex county, towns along the upper Middlesex and Worcester county border, along the Quabbin Reservoir watershed, and in southern Berkshire county.
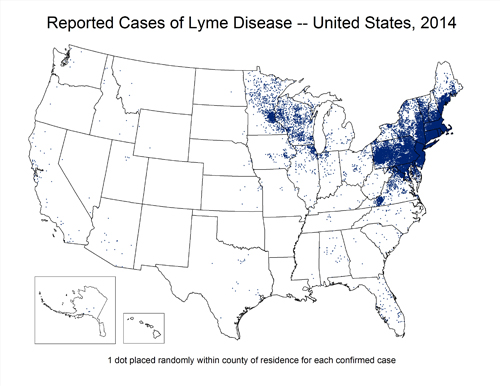
Source: http://www.cdc.gov/lyme/stats/maps.html
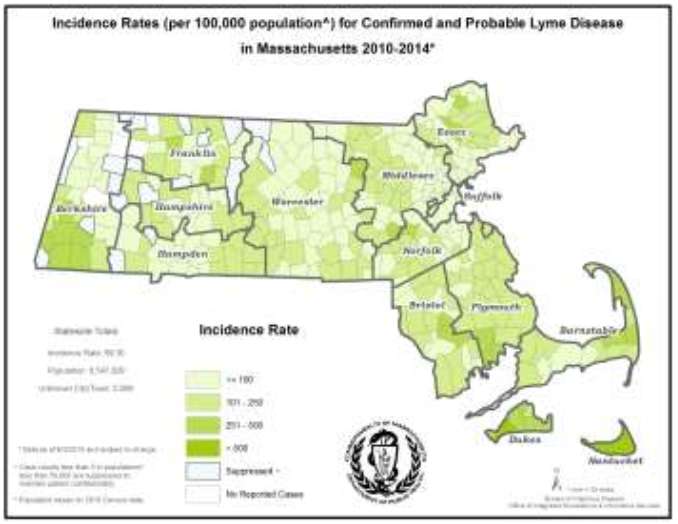
Source: http://www.westfordma.gov/pages/government/towndepartments/westfordma_healthcare/tick
Table - 2013 Confirmed and Probable Cases of Lyme Disease by County
|
County |
2013 Confirmed Cases |
2013 Probable Cases |
Incidence of Confirmed + Probable per 100,000 |
|---|---|---|---|
|
Barnstable |
186 |
88 |
127 |
|
Berkshire |
84 |
46 |
99 |
|
Bristol |
413 |
162 |
105 |
|
Dukes |
32 |
38 |
423 |
|
Essex |
405 |
154 |
75 |
|
Franklin |
51 |
20 |
100 |
|
Hampden |
167 |
57 |
48 |
|
Hampshire |
112 |
35 |
93 |
|
Middlesex |
720 |
267 |
66 |
|
Nantucket |
47 |
16 |
619 |
|
Norfolk |
460 |
150 |
91 |
|
Plymouth |
631 |
231 |
175 |
|
Suffolk |
81 |
49 |
18 |
|
Worcester |
480 |
194 |
84 |
|
Unknown |
211 |
76 |
- |
|
State Total |
4,080 |
1,585 |
65.1 |
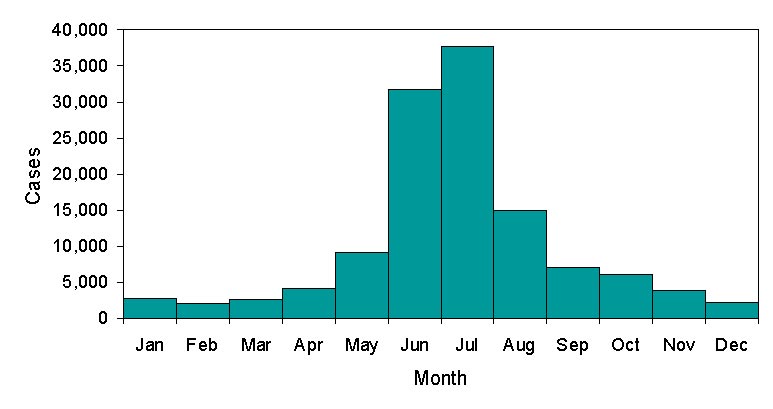
In Massachusetts, the highest risk of exposure to nymphs occurs during the spring and early summer, and the highest risk of exposure to adult ticks occurs during later summer into fall. Most cases have their onset between April and October, when the risk of contact with infected nymphal ticks is greatest. The graph below is from CDC.
Unlike most reportable diseases in Massachusetts which rely on follow-up of laboratory case reports by the local Board of Health, Lyme disease utilizes a physician-based reporting system. The Massachusetts Department of Public Health receives notification about most suspect cases of Lyme disease through receipt of positive laboratory tests which are submitted directly to the DPH Integrated Surveillance and Informatics System (ISIS) by laboratories. Receipt of a positive laboratory report generates a letter from ISIS to the physician with a teleform case report form for them to provide clinical information on. Local Boards of Health receive notification of positive laboratory results about residents as well but are not required to follow-up although they may choose to do so. Boards of Health that are trained on MAVEN are notified through that route; Boards of Health not on MAVEN receive a linelist of reports monthly.
Physicians are legally required to submit clinical information on any case of Lyme disease that they diagnose although this is an unreliable reporting method due to the heavy burden it places upon healthcare providers. However, some of the notification DPH receives about cases does originate from physicians reporting cases they have seen.
After clinical information is received by ISIS, the completed case report is reviewed by an epidemiologist at DPH and the standardized, national case definition is applied. The case definition separates cases into confirmed, probable and suspect cases based on consensus guidelines developed by the State Epidemiologists from all 50 states. The case definition can be viewed at: http://www.cdc.gov/osels/ph_surveillance/nndss/phs/infdis2011.htm. A large proportion of Massachusetts cases fall into the suspect disease category simply because DPH never receives any clinical information regarding a patient with a positive laboratory test. Because laboratory testing alone is not sufficient to identify cases of disease, these cases cannot be included in Massachusetts case counts of confirmed and probable cases which are the numbers that are reported to CDC and available for public release.
The local Board of Health also receives notification of the positive lab reports but is not expected to do any case investigation.
Note that there is controversy regarding reporting of Lyme disease discovered in its later stages. The CDC case definition is restricted to early cases of Lyme disease, while Massachusetts uses a broader definition that includes both early and late states.
lLink to a discussion of the controversy.
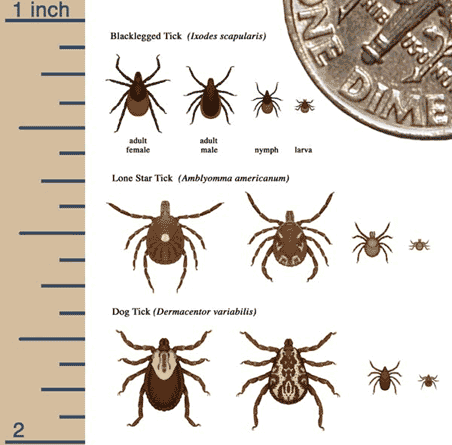
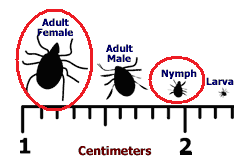
Borrelia burgdorferi is predominantly found in a species of hard ticks known as Ixodes scapularis, more commonly known as the "deer tick" or the "blacklegged tick." Female I. scapularis have a red-orange body with a black dorsal plate behind the mouthparts, and are about 3-3.7 mm long (about the size of a sesame seed).

The illustrations below indicate the relative sizes of the male and female adults and the nymph and larva stage.
Source: http://www.cdc.gov/ticks/life_cycle_and_hosts.html
The males are slightly smaller than the females and mostly black. Only nymph-stage and adult female deer ticks transmit the causative agent of Lyme disease to humans. An unfed adult female Ixodes scapularis is shown above to the left. (Source: Multipleorganisms.net). Female deer ticks become much larger when engorged with blood and can be confused with American dog ticks.
Only deer ticks (blacklegged ticks) carry the bacteria responsible for Lyme disease. Other tick species (e.g., American Dog ticks, Brown Dog ticks, and Lone-Star ticks) do not carry Borrellia burgdorferi, although they can transmit other diseases. Dog ticks carry the ricketsiae responsible for Rocky-Mountain Spotted Fever, which exists primarily in the Southwestern US and occasionally in Massachusetts. It is also important to note that the bite of a deer tick does not always result in Lyme disease. The probability of disease depends on how long the tick is attached, since longer attachment provides more opportunity to disgorge a sufficient number of bacteria. An infected tick must be attached for about 24-48 hours for the host to become infected. Consequently, ticks should be removed as soon as possible when they are found to be attached.
The life cycle of the deer tick in the northeastern United States is usually around two years, and consists of four stages:
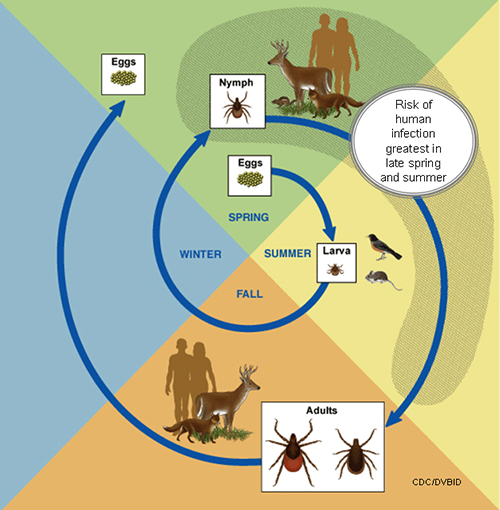
Source: http://www.cdc.gov/ticks/life_cycle_and_hosts.html
"Blacklegged ticks live for two years and have three feeding stages: larvae, nymph, and adult. Tick eggs are laid in the spring and hatch as larvae in the summer. Larvae feed on mice, birds, and other small animals in the summer and early fall. When a young tick feeds on an infected animal, the tick takes bacteria into its body along with the blood meal, and it remains infected for the rest of its life. After this initial feeding, the larvae become inactive as they grow into nymphs. The following spring, nymphs seek blood meals in order to fuel their growth into adults. When the tick feeds again, it can transmit the bacterium to its new host. Usually the new host is another small rodent, but sometimes the new host is a human. Most cases of human illness occur in the late spring and summer when the tiny nymphs are most active and human outdoor activity is greatest. Adult ticks feed on large animals, and sometimes on humans. In the spring, adult female ticks lay their eggs on the ground, completing the life cycle. Although adult ticks often feed on deer, these animals do not become infected. Deer are nevertheless important in transporting ticks and maintaining tick populations."
Relative abundance of the three major tick stages during the year.
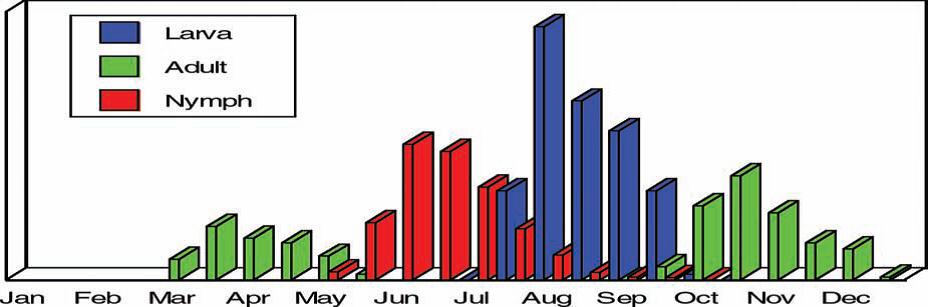
Source: Connecticut Tick Management Handbook)
Ticks become infected with the bacterium while feeding on an infected reservoir host. The most common hosts for larvae and nymphs are the white-footed mouse and birds. White tailed deer are the principal host for the adult ticks, but they do not become infected with Lyme disease. Rather, they are responsible for transporting ticks and maintaining tick populations in the wild. The white-footed mouse is the reservoir for the infection, and the tick is the vector.
This short video summarizes the key steps in transmission of Lyme disease.
Humans get Lyme disease after being bitten by an infected tick. Since ticks are obligate feeders, they need to attach to a host and take a blood meal in order to survive. Adult ticks climb to the tops of grasses and shrubs, where they wait for a large mammal host by "questing", i.e., perching on the ends of blades or grass or twigs, as illustrated below. When an unsuspecting human brushes against tall grass or leaves, the tick latches on and begins to bite the host. The image below shows a tick questing on the tip of a plant.

Source: http://www.foogle.biz/ticks/ticks_tix.htm
Mosquitoes land on a host and quickly bite and feed, but ticks are much slower. Ticks grasp the skin surface and cut into it over a period of 10-60 minutes. Once the skin is penetrated, the tick flues itself in place by secreting a sticky substance to hold its mouth in place. This allows the tick to feed gradually over a period of days. The smaller mouthparts on larval and nymphal ticks penetrate less deeply and evoke a smaller host reaction. Adults, however, can penetrate into the subdermal layer of skin making tick removal more difficult. The image below iis a diagram showing insertion of a tick during feeding.
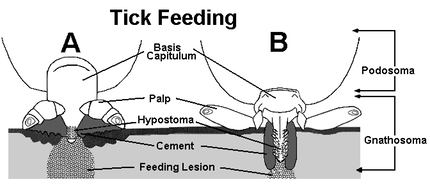
Source: https://identify.us.com/idmybug/ticks/tick-FAQS/do-ticks-really-cause-harm.html
It usually takes about 48 hours for the pathogen to be transmitted, so it is important to remove the tick properly as soon as it is found.
Link to more information on tick biology.
Ticks can attach themselves to any part of the body. While moist and warm areas (such as the armpits, bellybutton, back of the knees, ears, neck, groin area, etc.) tend to attract more ticks, a tick can attach itself anywhere on the skin and transmit the disease. A tick bite is not necessarily painful, which is why it is important to check for ticks everyday.
Tick Removal
When a tick is found to be attached, it should be removed promptly with thin-tipped tweezers at a 90 degree angle, making sure to grasp the tick as close to the skin as possible and pull upward with steady pressure, as illustrated in the image below.
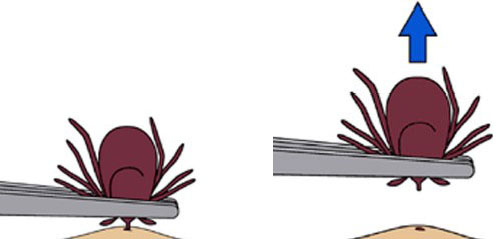
Source: http://www.cdc.gov/ticks/images/removal-ab.jpg
It is important to remove the entire tick in one piece. The area where the tick was attached should be disinfected with rubbing alcohol or other disinfectant. The individual should retain the tick in a small plastic vial and take it to a health care provider as soon as possible.
The video below shows the correct method for removing a tick.
If an individual is bitten by a tick, a physician should be consulted if the answers to the following questions are "yes."
Prophylactic Antibiotics
Many tick bites do not result in infection, and when infection does occur, most patients will manifest the characteristic skin rash. At present there is no evidence to support the use of prophylactic antibiotics after a tick bite in the absence of symptoms (see IDSA Guidelines). However, the treating physician may recommend a single dose of doxycycline to adults or children when all of the following conditions are met:
According to the CDC, there is no evidence that Lyme disease can be transmitted from person-to-person by touching, kissing or having sex with a person who has Lyme disease.
Lyme disease acquired during pregnancy may lead to infection of the placenta and possible stillbirth, however, no negative effects on the fetus have been found when the mother receives appropriate antibiotic treatment. There are no reports of Lyme disease transmission from breast milk.
Borrelia can live in blood stored for donation, and individuals being treated for Lyme disease with antibiotics should not donate blood. However, there are no reported cases of transmission of Lyme disease from blood donors.
Dogs and cats can get Lyme disease, but there is no evidence that they can transmit Lyme disease to humans. Nevertheless, pets can bring infected ticks into your home or yard. Owners should discuss the use of tick control products for their pets with a veterinarian.

Initial Signs and Symptoms
It takes about 48 hours for the bacterium to establish itself in the host. Usually, symptoms start to appear between 3 and 30 days after being bitten. The best clinical indication of the disease is the initial bull's eye rash, but the rash only occurs in 60-80% of patients. The concentric rash formed represents the spreading of the infection past the dermal layer and into other areas of the body. It is usually 5 centimeters (2 inches) or more in diameter, expanding about ½ to ¾ inch per day. It can last about three to five weeks, and it is generally not itchy. The bull's eye rash is usually accompanied by other symptoms, such as fatigue, fever, headache, mildly stiff neck, arthralgia, or myagia.
Late Signs and Symptoms
Without treatment, the infection may spread to other parts of the body within a few days to weeks and may produce the following problems:
Table of Early and Late Symptoms of Lyme Disease
|
Early Symptoms (3-30 days) |
Late Symptoms (1-4 months) |
|---|---|
|
|
The course and severity of Lyme disease are variable with each individual. Some individuals develop mild symptoms or may be asymptomatic for some time, while others can experience chronic and debilitating symptoms if left untreated. However, many of these symptoms will resolve, even without treatment.
Most cases of Lyme disease are associated with known exposure to a nymph or adult female deer tick bite and the appearance of the erythema migrans rash. Many physicians will diagnose patients on these criteria alone. Lyme disease is a reportable disease to local and state health departments, so laboratory confirmation of cases is important. There are three tests available to diagnose the disease:
CDC recommends a two-step process when testing blood for evidence of Lyme disease. Both steps can be done using the same blood sample, but CDC does not recommend testing blood by immunoblot without first testing it by ELISA (see below).
Some laboratories offer Lyme disease testing using assays whose accuracy and clinical usefulness have not been adequately established. Click here for more information. Patients should be encouraged to ask their physicians whether their testing for Lyme disease was performed using validated methods and whether results were interpreted using appropriate guidelines.

In the early stages of infection Lyme disease is completely curable with antibiotics such as:
The treatment during later stages of Lyme disease is more difficult, and some patients may still experience symptoms up to three months
after treatment. An intravenous drug, such as Ceftriaxone (Rocephin), is recommended for the later stages. Pain killers, such as Ibuprofen, can also be prescribed along with antibiotics to relieve joint pain.
Link to guidelines for treatment of Lyme disease
Individuals who spend a lot of time outdoors should be more careful about following precautionary measures. An individual doesn't necessarily have to be hiking or live in an extremely wooded area to contract the disease, since deer and mice have brought the disease to residential neighborhoods. Children under the age of 10 and adults over age 50 are at highest risk of contracting the disease, but anyone living in an area with infected deer ticks is at risk of contracting the illness. Individuals traveling to other endemic areas of the country are also at risk of infection.
Risk of Lyme Disease by Age and Gender (2001-2011)
Source: http://www.cdc.gov/lyme/stats/graphs.html
The single most effective method for preventing Lyme disease is personal protection:
This short video summarizes personal protective measures.
Since personal protection is the most effective method of preventing Lyme disease, strategies aimed at promoting awareness and adoption of personal protection measures are the most important intervention that a community health department can pursue.
Personal prevention measures are the most effective. Environmental approaches have also been suggested, but their effectiveness is controversial. This short video summarizes environmental approaches that may supplement personal protective measures.
Ticks are more likely to establish a habitat in close proximity to wooded areas as well as in areas with an abundance of groundcover vegetation, including leaf litter. They prefer dark, damp, and cool areas, especially in so called "transition areas" between the woods and the lawn. Keeping grass short and free of debris will make the environment less suitable for ticks to survive on.
Link to more information
Some authors have recommended the use of pesticides and acaricides for control. MDPH does not strongly encourage this as a prevention strategy, because of concerns related to pesticide exposures. While this can decrease the abundance of ticks in an area, pesticide application can have adverse consequences for the macro-environment.
Deer do not get infected with the bacterium that causes Lyme disease. However, deer are a main source of the blood adult ticks need to reproduce. Some have proposed that culling deer populations through increased hunting will reduce the incidence of Lyme disease.The impact of deer reduction on tick abundance or Lyme disease has been examined in several studies with mixed results. Studies on islands indicate that culling deer populations reduces the tick population, but this approach is not practical or realistic in the contiguous United States, since deer are constantly migrating. Even if one town in Massachusetts were to increase hunting of deer, it would prevent immigration of deer from adjacent towns, and the impact of this strategy in decreasing human disease remains unproven. For more information on deer management strategies see MassWildlife.
Another approach is to reduce tick populations by passive application of chemicals to deer and mice, although there is little evidence for the effectiveness of this approach. At present, these approaches are only experimental. For example, a 4-poster bait station can be used to passively apply insecticide to the neck and head of the deer in order to decrease the number of ticks attached to the deer as shown in the photograph below.
Source: http://www.deerfriendly.com/lyme-disease/4-poster-system-for-tick-control
While this may be a very effective method, the display can be expensive and a licensed insecticide applicator needs to replenish the display frequently, making it a less popular option. For more information about four posters, follow this link: American Lyme Disease Foundation.htm.
Another method is to use "tick tubes," shown below, which contain cotton treated with Permethrin, which kills ticks. Mice will enter the tube to retrieve cotton for their nests, and the Permethrin will adhere to the mice. For more information see the Damminix Tick Tube Fact Sheet.

Use of fungal pathogens and plants as biological control agents have been proposed to control tick populations. One area of research has focused on using the natural enemies of ticks native to the same areas. By increasing the numbers of these fungi found in the area, tick abundance would decrease through the process of "augmentative bio control." The use of natural enemies could potentially provide a more environmentally friendly and effective way to control the spread of pathogens. Further research on this and other methods of biological control are currently in progress.