Depression
Major depression is defined as persistent (months long), profound blues or irritable mood, and loss of interest interfering with normal functioning. A person may have one or repeated episodes over a lifetime. Over an individual's lifetime, one may experience depressive symptoms without having a major depressive episode. According to the Center for Disease Control and Prevention, depression affects 1 in 10 American adults.
|
The National Institute of Mental Health describes the signs and symptoms of depression as:
|
There is compelling evidence that physical activity is beneficial in preventing and treating depression.
- Many studies have shown that aerobic activity improves the response to pharmaceutical treatment in clinical depression.
- Physical activity can reduce depressive symptoms in persons without a clinical diagnosis of depression.
Exercise as Prevention of Depression
One of the most powerful components in the development of depression is stress. When the body is stressed, neurons release corticotrophin releasing factor (not corticotropin factor), which stimulates release of adrenocorticotropic hormone from the pituitary gland. This hormone causes the adrenal glands to secrete cortisol. Normally, there is a feedback inhibition by which increased cortisol levels in blood reduces secretion of additional corticotropin releasing factor. One theory is that continual stress can lead to dysfunction of this feedback mechanism, resulting in sustained elevations in cortisol that decreased secretion of brain-derived neurotrophic factor (NBDNF), which causes further damage to hippocampal neurons, thereby contributing to some of the cognitive abnormalities seen with depression.
|
|
|
A review by Farmer et al. [Farmer ME, Locker BZ, et al.: Physical activity and depressive symptoms: The NHANESI epidemiologic follow-up study. Am. J. Epidemiol. 1998;128:340-1351] examined the association between physical activity as it relates to the prevalence and incidence of depression and anxiety disorders. The authors cite several cross- sectional studies that report a high association between regular physical activity and low depression incidence in adolescents and the elderly. Once such study of 5,061 individuals by Steptoe and Butler [Sports participation and emotional wellbeing in adolescents. Lancet 1996;347:1789-1792] suggestted that vigorous physical activity was associated with reduced emotional distress. However, in cross-sectional studies it is not necessarily clear whether reduced emotional stress is a result of activity; an alternative explanation is that those with low stress levels are more inclined to exercise. Therefore, the authors concluded that randomized control trials are needed before concluding that exercise is an effective means of preventing depression.
Exercise as a Therapeutic Adjunct in Treating Depression
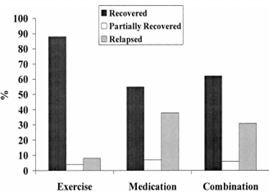
Depression is historically treated with antidepressants and psychotherapy . The study below showed a significant therapeutic benefit of exercise in individuals with major depression disorder. [Babyak M, Blumenthal JA, et al.: Exercise treatment for major depression:maintenance of therapeutic benefit at 10 months: Psychosom Med. 2000;62(5):633-8.] This randomized control trial was designed to assess the efficacy of physical activity in improving recovery from major depression disorder (MDD). They followed 156 adult individuals over the age of 50 with MDD for 4 months and assessed recovery at 10 months. Three interventions were compared: 1) aerobic exercise, 2) sertraline therapy
. The study below showed a significant therapeutic benefit of exercise in individuals with major depression disorder. [Babyak M, Blumenthal JA, et al.: Exercise treatment for major depression:maintenance of therapeutic benefit at 10 months: Psychosom Med. 2000;62(5):633-8.] This randomized control trial was designed to assess the efficacy of physical activity in improving recovery from major depression disorder (MDD). They followed 156 adult individuals over the age of 50 with MDD for 4 months and assessed recovery at 10 months. Three interventions were compared: 1) aerobic exercise, 2) sertraline therapy , or 3) a combination of exercise and sertraline. The study participants were given the Hamilton Rating Scale for Depression (HRSD) in order to determine the severity of MDD at baseline and at follow up of 4, 6 and 10 months. Subjects assigned to the exercise intervention attended three supervised 45 minute exercise classes a week, for 16 weeks. Subjects assigned to the medication group were initially prescribed 50 mg of sertraline and were titrated to a well-tolerated dosage of 200 mg. Subjects assigned to the combination group, received the same dosage of medication and exercise as other two intervention groups.
, or 3) a combination of exercise and sertraline. The study participants were given the Hamilton Rating Scale for Depression (HRSD) in order to determine the severity of MDD at baseline and at follow up of 4, 6 and 10 months. Subjects assigned to the exercise intervention attended three supervised 45 minute exercise classes a week, for 16 weeks. Subjects assigned to the medication group were initially prescribed 50 mg of sertraline and were titrated to a well-tolerated dosage of 200 mg. Subjects assigned to the combination group, received the same dosage of medication and exercise as other two intervention groups.
The analysis of the intervention included 133 subjects, as 23 subjects were lost to follow-up. The results as shown in the graph below show lower HRSD score in subjects who received the exercise only intervention (?? I don't think the graph shows this) (30%) compared to participants receiving just medication (52%) or those received combined therapy (55%) (p = .028). The investigators concluded that moderate exercise of at least 30 min, three times a week can be considered at least as effective as standard pharmacotherapy.
More research is needed in order to determine the best method of delivery and maintenance of physical activity in depressed individuals. In the systematic review Physical activity in the prevention and treatment of anxiety and depression (http://informa healthcare.com.ezproxy.bu.edu/doi/pdf/10.1080/08039480802315640 by EW Martinsen , Martinsen discusses the challenges of setting an appropriate minimum amount of exercise to improve depression. He also highlights the importance of continued research in behavior change models to encourage compliance in physical activity for depressed patients.
The Antidepressant Effects of Exercise
Though the exact physiological or biological mechanism remains inconclusive, there are several prevailing hypotheses on exercise's antidepressant effect. There are many regions of the brain that regulate our emotions, yet no single region has be recognized as responsible for depression. In a meta-analysis by Lynette L. Craft and Frank M. Perna on the The Benefits of Exercise for the Clinically Depressed,(http://www.ncbi.nlm.nih.gov/pmc/articles/PMC474733/) the authors outline the following prevailing hypotheses on the biological and physiological relationship between exercise and depression.
Monoamine Hypothesis
Craft and Perna acknowledge that this is the most promising of the prevailing hypotheses. This hypothesis asserts that physical activity increases in the availability of brain neurotransmitters [(insert hidden definition: a chemical substance that is released at the end of a nerve fiber by the arrival of a nerve impulse and, by diffusing across the synapse or junction, causes the transfer of the impulse to another nerve fiber, a muscle fiber, or some other structure).] such as serotonin, dopamine and norepinephrine. A clinically depressed individual exhibits depleted levels of such neurotransmitters. However, studies have only been conducted on animals, and it is still unknown if exercise leads to an increase in neurotransmitters in the human brain.
Photo from slide from class
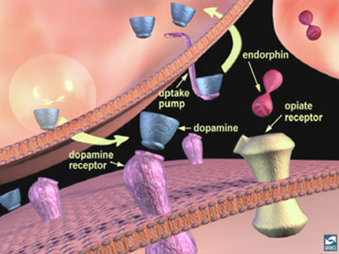
This image demonstrates how dopamine works to enhance or diminish excitability of regions of neurons
Endorphin Hypothesis
This hypothesis asserts that the increase of beta-endorphins ( insert hidden definition: Endorphins are endogenous opioid polypeptide compounds produced by the pituitary gland and the hypothalamus in vertebrates during strenuous exercise, excitement, pain, and they resemble the opiates in their abilities to produce analgesia and a sense of well-being) during exercise have a beneficial effect on depression. Beta-endorphins create an overall sense of well-being and can even induce a feeling of euphoria, often referred to as "runner's-high". Proponents of this hypothesis state that increases in plasma endorphins during exercise contribute to a reduction in depression symptoms. Critics debate if there is enough evidence to link increased levels of plasma endorphins to changes in brain chemistry exhibited in depressed individuals.
Distraction Hypothesis
Unlike the other hypotheses, the distraction hypothesis is based on psychology and suggests that physical activity provides a distraction from anxieties and depressing thoughts. However critics suggest that although exercise may cause a distraction for depressed individuals, exercise can also "increase positive affect, which is diminished in depressed patients and is not augmented by distraction activities."
The Link Between Depression and Exercise in the News
In this link Gretchen Reynolds of the NY times blog Well discusses walking as a treatment for depression. Reynolds examines the currents on exercise vs. pharmaceutical medication (SSRI's).
Stephen Ilardi is a clinical psychologist and associate professor at the University of Kansas who has spent his career investigating the cause and treatment of depression. The video below is a 22 minute TEDx Emory in which Dr. Ilardi discusses the "Depression Epidemic" in our civilization and proscribes exercise and omega-3 fatty acids as the cure to depression.
Quiz Question
True or False
Exercise alone can cure major depression disorder
False: Exercise is a supplemental treatment that should be combined with psychotherapy and/or prescribed medication.