The Quality of Health Care
Introduction
 Over the course of this semester, you have repeatedly heard the terms cost, access, and quality. That's because these are the major cornerstones of health care delivery, and essentially the crux of the debate that is going on in America's current health care reform discussion. As you read Chapter 12, you can see that attempts to control the growing costs of health care expenditures through cost containment initiatives by the government, third-party payers, and employers, and to expand access to services, have been an ongoing effort. However, today, especially with an alarming rise in medical errors, the focus is also shifting toward quality improvement and safety issues, as well as public expectations and demands for quality health care services.
Over the course of this semester, you have repeatedly heard the terms cost, access, and quality. That's because these are the major cornerstones of health care delivery, and essentially the crux of the debate that is going on in America's current health care reform discussion. As you read Chapter 12, you can see that attempts to control the growing costs of health care expenditures through cost containment initiatives by the government, third-party payers, and employers, and to expand access to services, have been an ongoing effort. However, today, especially with an alarming rise in medical errors, the focus is also shifting toward quality improvement and safety issues, as well as public expectations and demands for quality health care services.
Learning Objectives
After successfully completing this unit, the student will be able to:
- Describe the existence, nature, and consequences of quality-related problems in the United States health care system.
- Describe alternative approaches to assessing quality through performance, process, and/or outcome measures. Define performance, process, and outcome measures.
- Utilize specific quality measures to describe the performance of a health care facility.
- Describe current management approaches to quality improvement within health care institutions, specifically the Lean Management (e.g., TPS from Virginia Mason Medical Center) and Six Sigma systems.
- Describe the current policy approaches to improving the quality of care within health care
- Discuss the magnitude of the problem of medical errors and the challenges to reducing them. Discuss the importance of clear communication between patient and provider.
 ;
;
We said in the beginning that the United States has some of the highest costs and unequal access, with only average health outcomes. The figure below (which figure???) presents data from OECD (The Organization for Economic Co-operation and Development). OECD collects data on economics and policy for the 34 member nations. Health is one of the many topic areas. The figure below presents results from the 2011 report of health indicators.
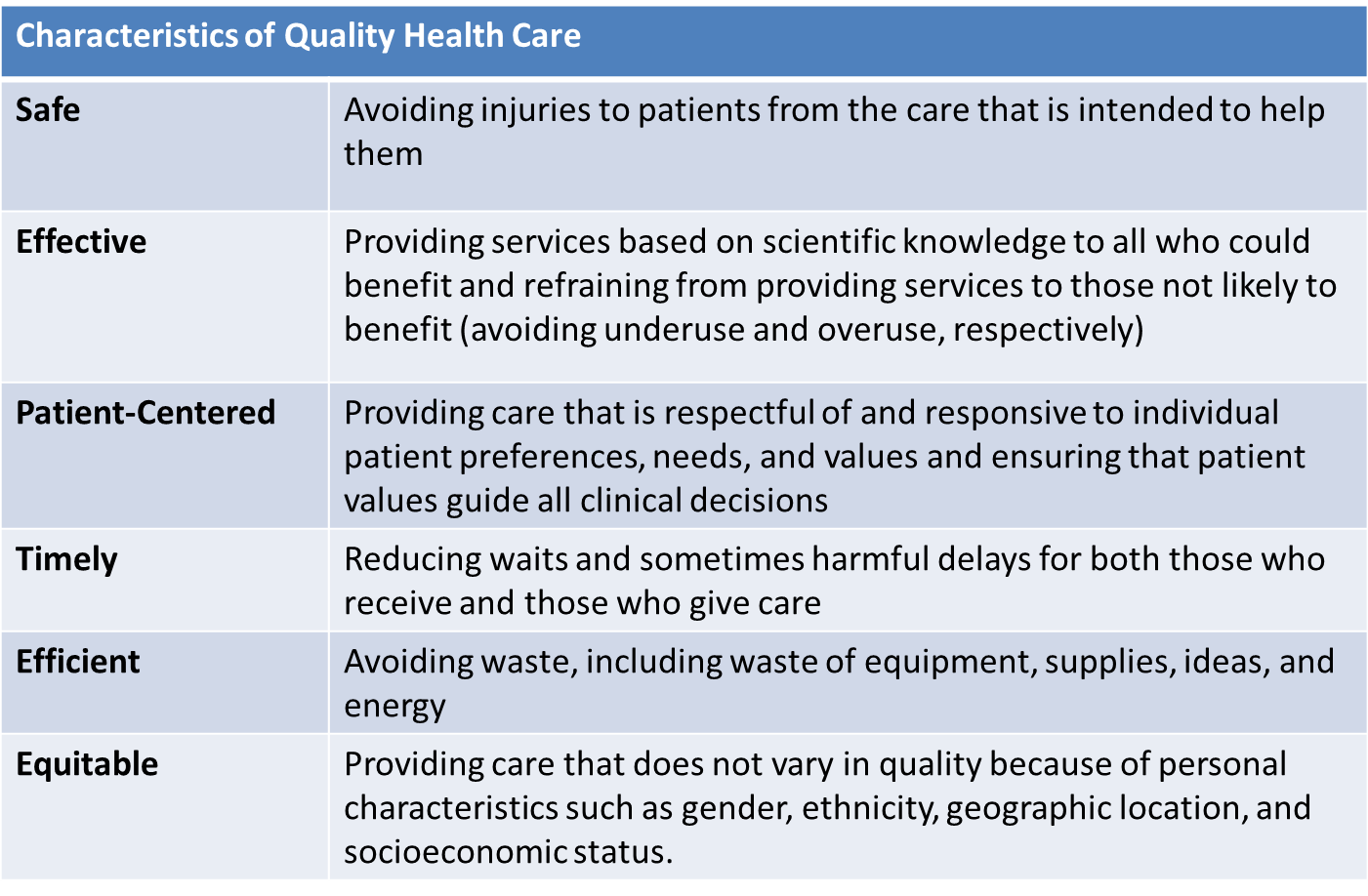
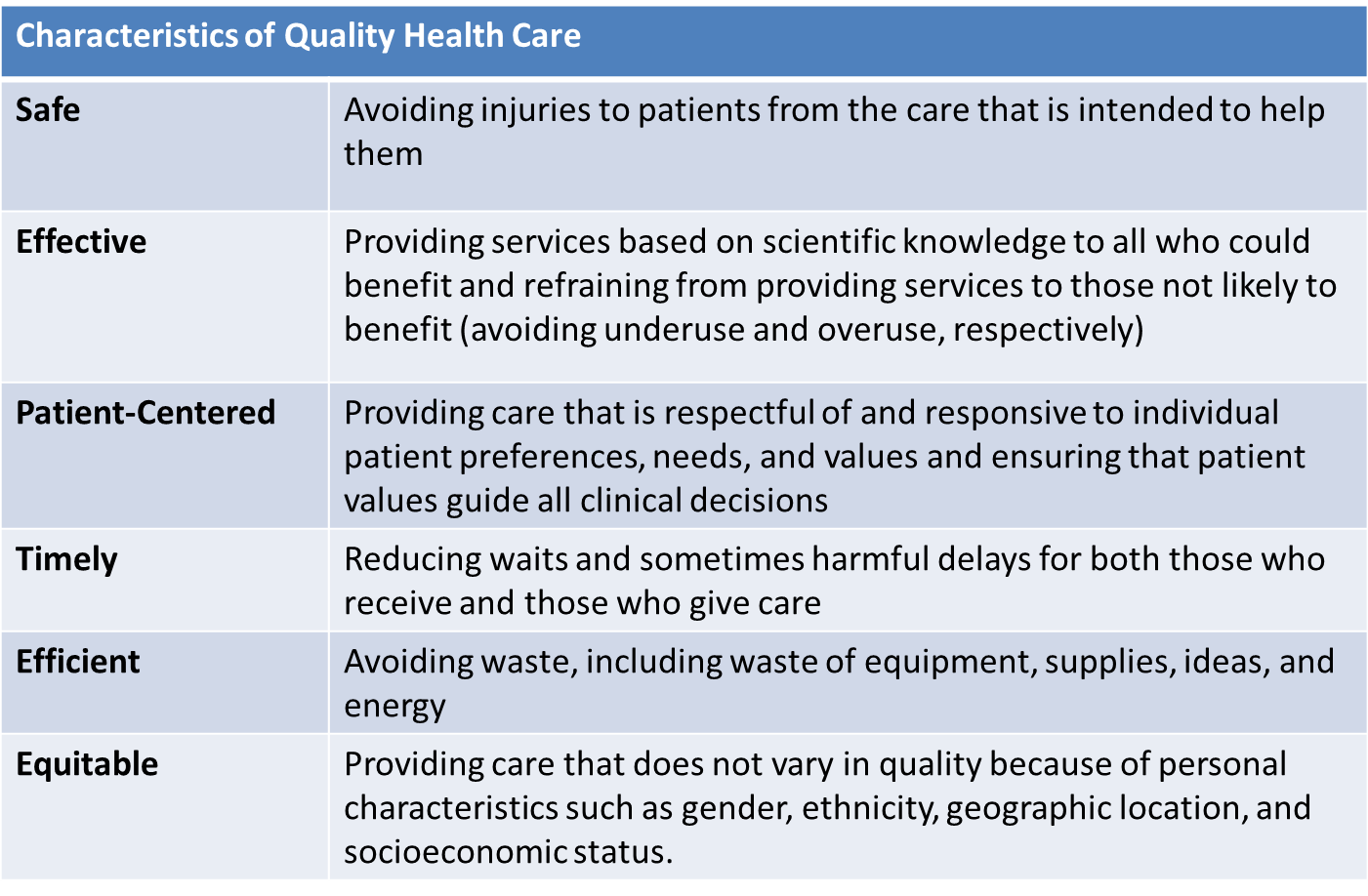
The Definition of Quality
"Quality is the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge."
Institute of Medicine , McGlynn, 1997, as quoted in Shi & Singh, 2008
According to Shi and Singh (2013), both micro- and macro-perspectives determine quality. For example, some micro quality indicators might be small area variations, medical errors, patient satisfaction, quality of life, and health outcomes. Macro quality indicators would be cost, access, and population health.
|
Micro Quality Indicators
|
Macro Quality Indicators
|
- Small area variations
- Medical errors
- Patient satisfaction
- Quality of life
- Health outcomes
|
- Cost
- Access
- Population health
|
Structure, process, and outcomes in determining quality are closely linked, as shown below. Here are some simple definitions:
- Structure
- Process
- Outcomes
Ideally these are linked horizontally. The structural characteristics impact or inform the processes. The processes then impact or inform the outcomes.
In quality improvement it is said that you can't improve what you can't measure. Is that true? Maybe. Or maybe you can't track improvement. What if your efforts to make things better really makes them worse?
More Process and Outcome Measures
What do or should we care about the most if we take the patient-centered perspective? Outcomes. We want to know how things turn out for the patient. What do we tend to measure? Processes. Why? Because that is what we control (can improve) and it is what we can most easily measure. We hope that what we do truly makes a difference in the patient's outcome.
Think about this example. We want to decrease mortality from cardiovascular disease in a cohort of patients being followed at a medical practice. That can be hard to measure. Unless your cohort is pretty old you may have to wait a long time to see the outcome, or you may not even be able to. People move, change insurance, or change primary care.
Then add another layer. How much of health is attributable to medical care? We saw that race/ethnicity, income and education make a difference. Can a PMD change those patient characteristics? From the biophysical perspective, what do we believe impacts cardiovascular disease: genetics, diet, diabetes, age (although we can age-adjust the results), obesity, smoking, the list goes on.
What might the practice decide to measure? Cholesterol levels of patients - patient outcome. Again though, how much does the doctor impact that? You are looking at an absolute measure. What if a patient came in with cholesterol of 350 (high) and working with the PMD got it down to 200 (still elevated). The PMD gets no credit.
What might get measured, especially in a practice with an electronic record, are: what percent of patients had cholesterol checked (process) what percent of patients with elevated cholesterol are on an appropriate medication regimen; and what percent of patients with an elevated cholesterol had documentation of counseling regarding diet and exercise.
Do these process measures actually matter to what happens to the patient in term of cardiovascular mortality? Answer: unclear.
Institute of Medicine Report on Quality of Care
Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academic Press; 2001.
Webinar
The following tutorial from the Agency for Healthcare Research and Quality discusses how we measure health care quality.
Tutorials & Presentations: Measuring Health Care Quality. KaiserEDU.
The Agency for Healthcare Research and Quality's (AHRQ) specific mission is to act as a problem solver and to improve the quality, safety, and effectiveness of health care for all Americans. Some major aspects of the AHRQ's work include research to support evidence-based decision-making, by developing and synthesizing scientific evidence regarding the effectiveness and quality of clinical services.
Other work is done in the area of patient safety, and how to improve the quality and safety of health care, addressing questions related to medical errors and how scientific information can make
the whole system safer. Go to http://www.ahrq.gov for more information on this and how the AHRQ uses research data to improve quality through evidence-based decision-making or on its quality indicators for hospitals, physicians, and other health providers, as well as its investment in information technology (IT), reporting systems, human capital, and other initiatives.
Medical Errors and Patient Safety
|
"Health care in the United States is not as safe as it should be - and can be. At least 44,000 people, and perhaps as many as 98,000 people, die in hospitals each year as a result of medical errors that could have been prevented, according to estimates from two major studies. Even using the lower estimate, preventable medical errors in hospitals exceed attributable deaths to such feared threats as motor-vehicle wrecks, breast cancer, and AIDS.
Medical errors can be defined as the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim. Among the problems that commonly occur during the course of providing health care are adverse drug events and improper transfusions, surgical injuries and wrong-site surgery, suicides, restraint-related injuries or death, falls, burns, pressure ulcers, and mistaken patient identities. High error rates with serious consequences are most likely to occur in intensive care units, operating rooms, and emergency departments.
Beyond their cost in human lives, preventable medical errors exact other significant tolls. They have been estimated to result in total costs (including the expense of additional care necessitated by the errors, lost income and household productivity, and disability) of between $17 billion and $29 billion per year in hospitals nationwide."
"A variety of factors have contributed to the nation's epidemic of medical errors. One oft-cited problem arises from the decentralized and fragmented nature of the health care delivery system - or "nonsystem," to some observers. When patients see multiple providers in different settings, none of whom has access to complete information, it becomes easier for things to go wrong.
From 1999 Institute of Medicine report "To Err is Human - Building a Safer Health System"
|
Medical information is becoming increasingly complex and for various reasons (time constraints, stress of multitasking, too many patients, not enough staff, learning curve with health IT, lack of awareness, etc.), health care professionals do not always explain information in a way that patients can understand. Health care professionals may not even know when patients do not understand, nor do patients ask their providers to explain complicated information (perhaps due to embarrassment or fear of questioning the "experts").
Types of Medical Errors
|
Diagnostic
- Error or delay in diagnosis
- Failure to employ indicated tests
- Use of outmoded tests or therapy
- Failure to act on results of monitoring or testing
Treatment
- Error in the performance of an operation, procedure, or test
- Error in administering the treatment
- Error in the dose or method of using a drug
- Avoidable delay in treatment or in responding to an abnormal test
- Inappropriate (not indicated) care
Preventive
- Failure to provide prophylactic treatment
- Inadequate monitoring or follow-up of treatment
Other
- Failure of communication
- Equipment failure
- Other system failure
SOURCE: Leape, Lucian; Lawthers, Ann G.; Brennan, Troyen A., et al. Preventing Medical Injury. Qual Rev Bull. 19(5):144–149, 1993.
|
A few Developments in Process Improvement: (Shi & Singh, 2013)
- Clinical Practice Guidelines :In response to findings of small area variations, various professional groups, MCOs, and the government have embarked on the development of standardized practice guidelines
- Cost-Efficiency : This occurs when the benefit received is greater than the cost incurred in providing the service
- Critical Pathways: These are outcome-based and patient-centered case management tools that are interdisciplinary and that facilitate coordination of care among multiple clinical departments and caregivers
- Risk Management: This is a proactive effort to prevent adverse events related to clinical care and facilities operations, and is frequently focused on avoiding medical malpractice.
Practitioners predict that quality will "trump finances" in communities throughout the US.
97 percent believe that all hospitals will have governing boards with special committees on hospital quality and patient safety by 2014. Many believe that "zero tolerance" will be used instead of basing goals on average industry standards. Many also expect that hospitals will adopt programs developed by the aviation and manufacturing industries to improve communication and reduce medical errors, and that senior management bonuses will be determined by achievement of quality outcomes over achievement of financial goals. The pay-for-performance model of reimbursement will make patient care safer.
Accountability
Watch the following video on patient safety to put human faces into the maze of technology, critical pathways, clinical guidelines, and cost efficiency initiatives. Consider where carefully framed theories, rules, and regulations wane and reality takes over.
Joint Commission Speak Up: Prevent errors in your care, Monday, March 07, 2011
Speak Up: Prevent errors in your care
Improving Health Care Together
"Learn about Joint Commission Resources (JCR) and its work with the Partnership for Patients initiative. Launched in December 2011, the initiative brings together leaders of major hospitals, employers, physicians, nurses, and patient advocates along with state and federal governments in a shared effort to make hospital care safer, more reliable, and less costly."
~ www.jointcommission.org/multimedia/default.aspx
Podcast: on Medical Errors
Health care providers are people. Human error is bound to happen. We have systems in place to minimize error, but they are not enough to prevent all mistakes. No one goes to work wanting to harm a patient. There is increasing recognition that a health care provider involved in a serious medical error is a 'second victim.' For more information on this topic visit the Institute for Healthcare Improvement (IHI) web site: www.ihi.org
Danielle Ofri is a writer and a practicing physician at Bellevue Medical Center in New York City. In this installment of the Narrative Matters series from Health Affairs she presents her experience with a medical error and related this to disclosure, apology and the role of shame. Click the source link below to view the links to the podcasts.
To listen to the podcast click: https://itunes.apple.com/us/podcast/danielle-ofri-ashamed-to-admit/id407251174?i=89380209&mt=2
Health Literacy
A discussion of the American health care system also needs to consider access and quality issues, and it stands to reason that the health and health care of a person with low health literacy (who is unable to understand health information or medical instructions about medications or diet) will be compromised as a result. And—after seeing the impact of time and staff shortages, cost reductions, tougher regulations, etc., on our health providers—is it any wonder that they may not even be aware their patients don't understand the materials and handouts they are being given?
Consider the connection between health literacy, patient safety, and medical errors. Patients who know how to ask questions of providers, and providers who know how to answer patients in plain language, can go a very long way to improving the health care of our population.
Some excellent web sites that provide comprehensive information on health literacy include the US Department of Health and Human Resources (HRSA) site:
- HRSA on Health Literacy
- Quick Guide to Health Literacy
Comparative Effectiveness Research (CER)
Comparative effectiveness research (CER) compares two or more treatments on the basis of effectiveness, benefit and risk. Treatments include more than medications. Treatments compared may be devices, tests, procedures, or other intervention designed to improve health.
The ACA provides funding for CER through the Patient Centered Outcomes Research Institute (PCORI). PCORI studies can be original research or the analysis of existing data. The ACA contains language restricting the use of data regarding cost, specifically use of QALYs. PCORI research cannot use cost per QALY to make decisions on coverage for Federal programs. Why? Because of the concern that the quality adjustment used to determine a QALY discounts the lives of the old and ill. Thus, CER (comparative effectiveness research) has not been universally embraced (think death panels). As you can tell, the issues are complicated and it remains unclear how this will be fully resolved.
FAQ: Comparative Effectiveness Research
Why is comparative effectiveness research needed? What problem is it trying to solve?
- If you don't get the best possible information about your treatment choices, you might not make an informed decision on what treatment is best for you.
- When you shop for a new car, phone or camera, you have lots of information about your choices. But when it comes to choosing the right medicine or the best health-care treatment, clear and dependable information can be very hard to find.
- It's true that some treatments may not work for everyone, and that some treatments may work better for some people than others. This research can help identify the treatments that may work best for you.
What are the practical benefits of comparative effectiveness research?
- You deserve the best and most objective information about treating your sickness or condition. With this research in hand, you and your doctor can work together to make the best possible treatment choices.
- For example, someone with high blood pressure might have more than a dozen medicines to choose from. Someone with heart disease might need to choose between having heart surgery or taking medicine to open a clogged artery. Reports on these topics and others include the pros and cons of all the options so that you and your doctor can make the best possible treatment decision for you or someone in your family.
- Every patient is different — different circumstances, different medical history, different values. These reports don't tell you and your doctor which treatment to choose. Instead, they offer an important tool to help you and your doctor understand the facts about different treatments.
Source: http://effectivehealthcare.ahrq.gov/index.cfm/what-is-comparative-effectiveness-research1/
QALY Quiz
Patient A has a common and life threatening condition. The current treatment provides a life expectancy of 2 years at a quality level of 0.3.A radical new treatment recently approved by the FDA gives a life expectancy of 2 years and 3 months at a quality level of 0.4. Costs of the current treatment is $5000 per year, while the costs of the new treatment is $25000 per year.
1) Compute the current and new QALYs. What is the difference in QALY between the current and new treatments?
Answer
2) What is the incremental cost of the new drug for an added QALY?
Answer
3) Should payers pay for the new drug? (Use a standard of $100,000 per QALY as the upper limit for payment.)
Answer
4) Suppose that 250,000 people have the condition described above. Given the information provided above for this scenario, what is the cost of the current treatment to the total health care system?
Answer
5) Suppose again that 250,000 people have the condition described above. What will be the cost of the new treatment to the total health care system?
Answer
Policy and Management Approaches to Quality
Hospital Readmissions
Here was the problem: High (1 in 5) readmission rates for Medicare patients admitted to hospitals with heart attacks, heart failure, and pneumonia. The primary concern was cost to the Medicare program.
There have been several health policy attempts to remedy the situation. Remember Medicare is a federal program and so this is federal policy.
If you have never visited the CMS web site Hospital Compare you should do so now. Hospital Compare gives transparency to the performance of hospitals. Hospital readmission rates are a quality measure to capture a patient outcome. There are two intended effects. Consumers may be able to make more informed decisions and thereby receive a higher quality of care. Also hospitals will be able to see their relative performance and this could incentivize efforts to decrease readmission rates.
What Is Hospital Compare?
Hospital Compare has information about the quality of care at over 4,000 Medicare-certified hospitals across the country. You can use Hospital Compare to find hospitals and compare the quality of their care.
The information on Hospital Compare:
- Can help you make decisions about where you get your health care;
- Encourages hospitals to improve the quality of care they provide.
Remember, in an emergency, you should go to the nearest hospital. When you can plan ahead, discuss the information you find here with your health care provider to decide which hospital will best meet your health care needs.
Learn more in the Guide to Choosing a Hospital.
Hospital Compare was created through the efforts of the Centers for Medicare & Medicaid Services (CMS), in collaboration with organizations representing consumers, hospitals, doctors, employers, accrediting organizations, and other Federal agencies.
For more information on Hospital Compare, check out the CMS web cast at http://www.youtube.com/watch?v=-IeW0Zjyhrs
In fall of 2012 CMS began to financially penalize hospitals for higher than expected readmission rates for Medicare patients with these three conditions.
This is a result of the ACA, and part of value-based purchasing as we discussed in Week 3. The goals are to create a financial incentive for hospitals to give better care; to not send home patients who are not ready to leave, to do a better job transitioning patients home to PCP follow-up. It is too soon to know if there are unintended consequences. It is very possible that this could discourage hospitals from caring for high-risk patients. Remember the social determinants of health. Hospitals caring for disproportionate shares of disadvantaged patients may be unfairly penalized.
ACOs may reduce readmission rates. If an ACO has primary care and hospital components, that group is at financial risk when patients are readmitted. It costs more to care for a patient in the hospital than in the community. This story will continue to evolve, stay tuned.
Management Approached to Quality: Readmissions
Health policy has created incentives for hospitals to reduce readmission rates. What are the management initiatives to reduce readmissions?
The video below is from the New England Healthcare Institute (NEHI). NEHI is a non-profit organization for health policy research. Watch this and learn about the scope of the problem and some possible solutions.
Bend the Curve: Preventing Hospital Readmissions
Source: www.youtube.com/watch?v=dRUvsv5V1Pg&feature=youtu.be
For more information about health care quality, visit the Agency for Health Care Research and Quality (AHRQ) and check out their state dashboard. You can compare state health care quality performance indicators on specified measures. http://statesnapshots.ahrq.gov/snaps09/dashboard.jsp?menuId=4&state=&level=0
 Over the course of this semester, you have repeatedly heard the terms cost, access, and quality. That's because these are the major cornerstones of health care delivery, and essentially the crux of the debate that is going on in America's current health care reform discussion. As you read Chapter 12, you can see that attempts to control the growing costs of health care expenditures through cost containment initiatives by the government, third-party payers, and employers, and to expand access to services, have been an ongoing effort. However, today, especially with an alarming rise in medical errors, the focus is also shifting toward quality improvement and safety issues, as well as public expectations and demands for quality health care services.
Over the course of this semester, you have repeatedly heard the terms cost, access, and quality. That's because these are the major cornerstones of health care delivery, and essentially the crux of the debate that is going on in America's current health care reform discussion. As you read Chapter 12, you can see that attempts to control the growing costs of health care expenditures through cost containment initiatives by the government, third-party payers, and employers, and to expand access to services, have been an ongoing effort. However, today, especially with an alarming rise in medical errors, the focus is also shifting toward quality improvement and safety issues, as well as public expectations and demands for quality health care services. ;
;