
Linking Quality, Cost, and Outcomes

Cost, access, and quality are the cornerstones of health care delivery, and these issues are the focus of the ongoing debate regarding health care in the United States. We continue to try to find ways to control costs of health care through cost containment initiatives by the government, third-party payers, and employers, and we continue to try to expand access to services. In addition, an alarming rise in medical errors, there is also aa growing focus on quality improvement and safety.
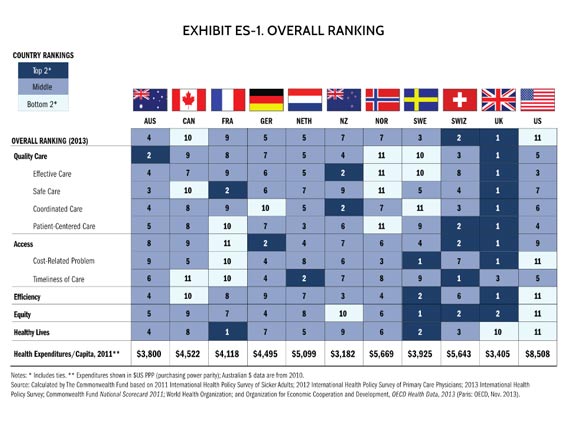
How do we compare to other countries? The United States has some of the highest costs and unequal access, with only average health outcomes. The graphic below is from The Commonwealth Fund's 2014 report on comparative performance of international health systems.
After successfully completing this module, you will be able to:

A goal of health reform is to increase access. A major goal of the ACA are to Increase insurance coverage through Medicaid expansion, state health exchanges, and the individual mandate.. However, a possible unintended consequence of expanding coverage is that the shortage of primary care physicians will worsen as a result of an increase in the number of individuals trying to obtain care (demand) without increasing the already inadequate number of PCPs (supply). In addition, by providing more people with coverage, there will be an increase in care-seeking behavior and an increase of total health care costs.
The hope is that increased coverage will improve the health of the population, but will this save money in the long run? This is unclear.Massachusetts began a process of health reform several years ahead of the ACA. The first phase focused on increasing access (health insurance coverage). More people are covered now, and it is costing more. The next phase in Massachusetts is to contain cost, but it is too early to know if this will succeed.
"Cost" in the health care arena has different meanings depending on one's perspective, specialty, and environment.
|
Some Observations About the Cost of Health Care "Perhaps the most difficult long-term challenge facing Obamacare is cost control. The ACA does contain substantial savings in Medicare, but limits on other spending are less robust. The law initiates a broad array of experiments in medical care delivery and payment reform whose success is highly uncertain."
"The costs of the system's current inefficiency underscore the urgent need for a system wide transformation. The committee calculated that about 30 percent of health spending in 2009 -- roughly $750 billion -- was wasted on unnecessary services, excessive administrative costs, fraud, and other problems. Moreover, inefficiencies cause needless suffering. By one estimate, roughly 75,000 deaths might have been averted in 2005 if every state had delivered care at the quality level of the best performing state." Institute of Medicine, Transformation of Health System Needed to Improve Care and Reduce Costs Press release, 9/6/2012
"62.1% of all bankruptcies have a medical cause. Most medical debtors were well educated and middle class; three quarters had health insurance. The share of bankruptcies attributable to medical problems rose by 50% between 2001 and 2007." Himmelstein, David U., et al. "Medical bankruptcy in the United States, 2007: results of a national study", The American Journal of Medicine 122.8 (2009): 741-746.
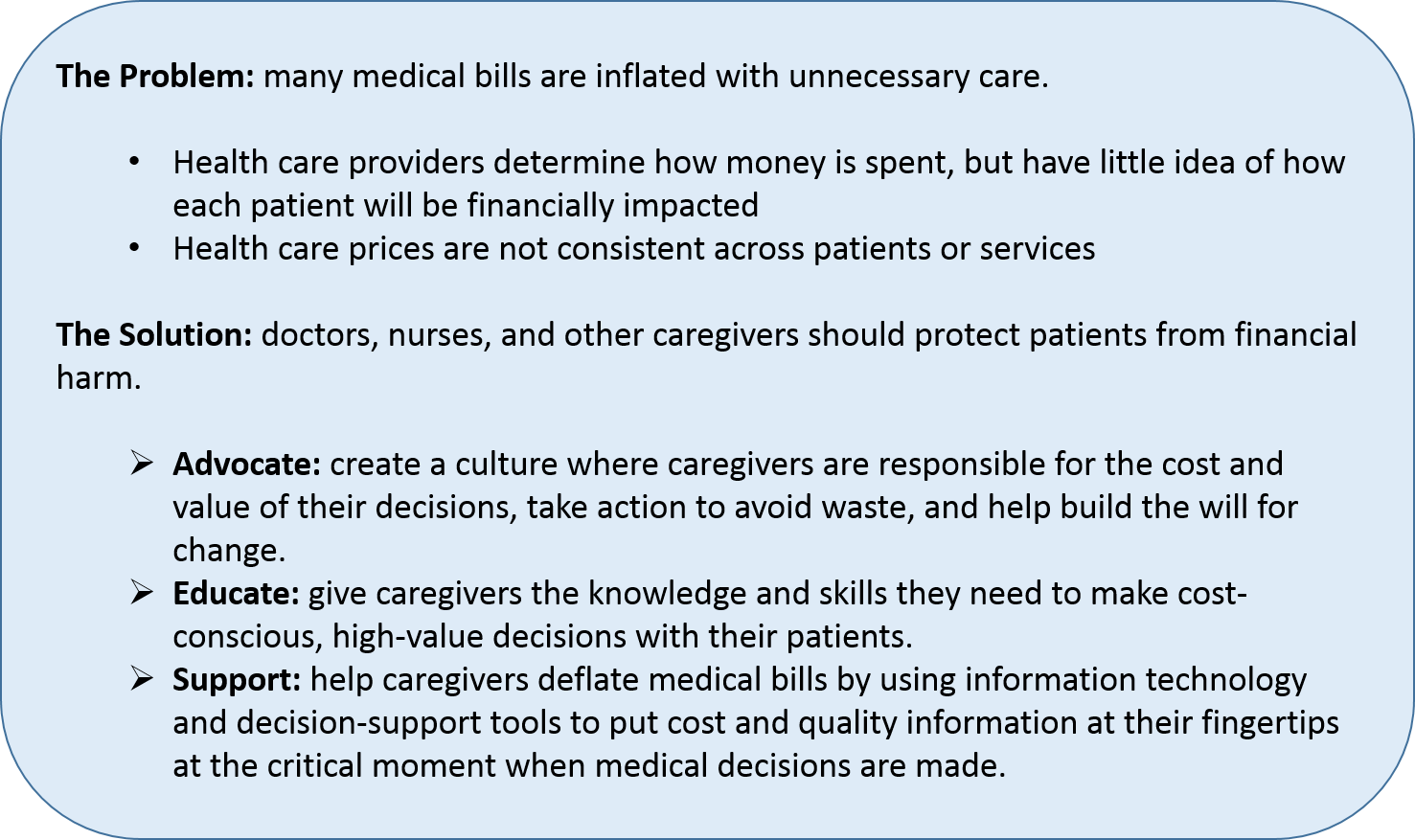
"Just as the patient safety movement helped caregivers think about how to prevent unintended harm, a new movement is needed to help caregivers think about unintended financial harms as well." Mission statement, Costs of Care organization |
|
Paying Till It Hurts: Why American Health Care Is So Pricey
Listen to the following piece on the cost of medical care in the US (from NPR) http://www.npr.org/2013/08/07/209585018/paying-till-it-hurts-why-american-health-care-is-so-pricey |
Costs of Care is a non-profit group dedicated to "transforming American healthcare delivery by empowering patients and their caregivers to deflate medical bills." High-value medical decisions should benefit patients' health, their finances, and decreases costs to the system.
According to the Researchers:
Health economist Ewe E. Reinhardt writes in the Journal of the American Medical Association (2013) that "the often advanced idea that American patients should have "more skin in the game" through higher cost sharing, inducing them to shop around for cost-effective health care, so far has been about as sensible as blindfolding shoppers entering a department store in the hope that inside they can and will then shop smartly for the merchandise they seek."
There are two basic problems with expecting consumers to choose high quality care at a reasonable cost.
Would any other business survive if it behaved like a hospital? Watch this video for an example of a customer service model that would not survive in a competitive hotel environment.
|
What if Hotels Billed Like Hospitals?
|
The model in health care is unacceptable, but provisions of the ACA do require increased uniformity and transparency of information on out of pocket costs for consumers.
|
"Quality is the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge." Institute of Medicine, McGlynn, 1997 |
Crossing the Quality Chasm
|
"In 2002, the Institute of Medicine published Crossing the Quality Chasm, an influential book that framed all future discussions of quality health care. Crossing came on the heels of the IOM publication To Err Is Human (2000) and a Journal of the American Medical Association report (1998) that warned of "serious and widespread quality problems...throughout American medicine." The report called attention to three broad categories of quality defects:
To Err Is Human estimated that as many as 98,000 people dies each year in hospitals from injuries or illness contracted during care.
In Crossing, the IOM outlined six specific aims (explained by Dr. Donald Berwick in the video above) that a health care system system must fulfill to deliver quality care:
Recognizing that aims must be accompanied by observable metrics, the IOM defined sets of measurements for each aim. For example:
Of course, this is all easier said than done. Hospitals could more easily follow evidence-based practices were there a national outcomes data base that provided population-based information. Effecting efficiency programs can mean a complete redesign of institutional culture, as in Virginia Mason's (Seattle) 20-year commitment to Lean management principles. Equitable care is unlikely without a sea change in national health policy (not that there is one) that extends well beyond the limitations of the Affordable Care Act.
The most encouraging developments in the industry-wide reassessment of quality are the recognition that safety and efficiency need not be mutually exclusive, an increased capacity for the practice of evidence-based medicine, and a new emphasis on patients when it comes to setting goals and measuring results."
Source: The Healthcare Quality Book (2nd edition), edited by Elizabeth R. Ransom, Maulik S. Joshi, David B. Nash, and Scott B. Ransom. |
In health services we often use the model of Avis Donabedian to conceptualiz and evaluate quality in health care. The model proposes that structure, process, and outcomes are closely linked and determine outcome.

Comparative effectiveness research (CER) compares two or more treatments on the basis of effectiveness, benefit and risk. Treatments include more than medications. Treatment is compared may be devices, tests, procedures, or other intervention designed to improve health. The ACA provides funding for CER through the Patient Centered Outcomes Research Institute (PCORI). PCORI studies can be original research or the analysis of existing data. The ACA contains language restricting the use of data regarding cost, specifically use of QALYs. A QALY is a quality adjusted life year. PCORI research cannot use cost per QALY to make decisions on coverage for Federal programs. Why? Because of the concern that the quality adjustment used to determine a QALY discounts the lives of the old and ill. Thus, CER (comparative effectiveness research) has not been universally embraced (think death panels). As you can tell, the issues are complicated and it remains unclear how this will be fully resolved.
FAQ on Comparative Effeciveness Research
Q: Why is comparative effectiveness research needed? What problem is it trying to solve?
Q: What are the practical benefits of comparative effectiveness research?
Source: What Is Comparative Effectiveness?
|
"The nation has been having the wrong conversation about healthcare. The wrong conversation focuses almost exclusively on the uninsured, offers the false promise of 'free' universal healthcare, and does not require individuals to assume responsibility for their own well-being. ~ Thomas J. Donohue, president and CEO of the US Chamber of Commerce, 2009 |
Many employers are unaware of the linkages between health and productivity. While employers understand that investing in human capital improves the company bottom line, they are only beginning to understand the impact health has on worker productivity.
These indirect costs affect all employers, even those who avoid direct medical costs by not funding health insurance.
From the Centers for Disease Control and Prevention, Workplace Health Promotion
|
Potential Benefits of Workplace Health Programs For Employers:
For Employees:
Source: Benefits of Health Promotion Promotions from the Centers for Disease Control and Prevention |
Examples of employer-sponsored health promotion/wellness programs:
Federalism is the distribution or balance of power between the central authority and constituent units. The same geographic area is covered by two levels of government: federal and state. The US Constitution gives the federal government power over what would be considered "natural considerations," such as declaring war, printing money, establishing a postal service, taxation, and interstate commerce (regulating what happens between states, but not within a single state). Federal powers are limited to those listed in the 10th amendment, but the interpretation of the Constitution is sometimes controversial. States have the authority to enact laws regarding public schools, child protection, licensure, elections, etc. Finally, there are also areas where there is overlap between federal state authority, e.g., taxation.
The challenge of the ACA by the states was based on whether the federal government had the authority to regulate health care. However, on June 28, 2012 the U.S. Supreme Court upheld the constitutionality of the ACA.
Health policy includes decisions by the legislature, the executive branch, and the courts in federal, state or local governments. Below is a table giving health care examples of four health policy tools for the state and federal governments.
|
|
State |
Federal |
|---|---|---|
|
Funding |
Medicaid (administered by state, funding is a split) |
Medicare (Medicaid), USDA farm subsidies, school lunch program, federally funded community health centers |
|
Provision of Services |
State hospitals, direct services by state health departments |
Veterans Administration (VA), Indian Health Service (HIS) |
|
Regulation |
Soda ban, seat belts, medical professional licensing, medical marijuana, MD assisted suicide |
ACA, HIPAA , FDA |
|
Taxation |
Cigarette taxes |
Cigarette taxes |
Medicare pays hospitals through DRGs. Hospitals are paid a lump sum for the admission. If the hospital is able to spend less money than the DRG then the hospital can keep the change. If the hospital over spends, Medicare does not give extra funds and the hospital takes a loss on that admission. Nevertheless, there is concern and evidence that if patients do not receive quality care at a hospital admission that Medicare will incur downstream costs.
Medicare has two strategies to motivate the hospital to provide high-quality care at each admission. The intent is to control Medicare spending.
|
Public Reporting: "Hospital Compare"
Hospital Compare has information about the quality of care at over 4,000 Medicare-certified hospitals across the country. You can use Hospital Compare to find hospitals and compare the quality of their care. The information on Hospital Compare:
Learn more in the Guide to Choosing a Hospital. Hospital Compare was created through the efforts of the Centers for Medicare & Medicaid Services (CMS), in collaboration with organizations representing consumers, hospitals, doctors, employers, accrediting organizations, and other Federal agencies. Source: Medicare.gov/Hospital Compare
In theory, transparency will allow for consumers to make choices based comparing quality; hospitals will be able to compare themselves against other institutions and this could motivate quality improvement. In reality, it is unclear how much consumers know about, understand, and use this information. |
|
Financial Incentives for Quality
Since 2008 Medicare has refused to pay for certain conditions not present when the patient at admission if these developed during the admission. These include leaving an object in the person during surgery, becoming injured in the hospital, developing a bedsore in the hospital, getting the wrong type of blood (can be fatal), and certain infections. In 2010, the ACA created three programs designed to improve both quality and efficiency using financial penalties and rewards, each of which was phased in over time.
There are criticisms of all three programs, especially from hospitals and other medical organizations. There is some overlap in HVBP and HAC. Safety-net hospitals have been getting penalized more than non-safety net hospitals. A safety-net hospital often has the most vulnerable patients with multiple chronic conditions and social stressors outside of the hospital. Supporters of the penalties believe that these measures are under the control of the hospitals and providers, and that vulnerable patients should be receiving the same quality of care as the rest of the population. Others would say these hospitals need extra funding because of the challenges posed by vulnerable populations. |
Hospitals have been trying a wide array of interventions to decrease readmission rates in order to avoid financial penalties from Medicare. Many of the programs in place are working. A recent study from Yale University surveyed 600 hospitals about their readmissions prevention practices. The study identified six elements associated with reduced readmission rates. The most successful hospitals utilized more than one strategy.
Factors Leading to Reduced Admission Rates
The video below from the Robert Wood Johnson highlights successful care transitions programs.
|
Solutions: Stopping the Revolving Door of Avoidable Readmissions Source:The Robert Wood Johnson Foundation
|
|
AAMC: American Association of Medical Colleges |
Abbreciations from "Essentials of the US Health Care System" book ACA of 2010 – Patient Protection and Affordable Care Act of 2010 |