Examples
Impetus to Transform
Example 1 The Pursuing Perfection (P2) grant was a major driving force behind Site X’s improvement efforts. While most systems had well-defined improvement programs in place by the time that P2 began, the program brought renewed focus. For systems with serious financial challenges, P2 funding contributed importantly to their improvement efforts. For all P2 systems, however, the prestige and visibility engendered by P2 seemed more important than the financial gain. As one senior manager in Site F said, “Pursuing Perfection gives legitimacy to the [clinical improvement] efforts… by building a coalition of people… and hopefully having a lasting impact. It provides a focus and gives a framework for changing culture in different parts of the organization… P2 challenges us to think about the next level. We are better thinkers than before…”
Example 2 In Site I, the impetus was the recognition by system leaders that organizational performance had plateaued and that the Baldrige Award criteria provided a framework for linking clinical improvement efforts with the organization’s business strategy. The Baldrige application process, with its deadlines and feedback opportunities, also created a powerful urgency to change.
Example 3 In Site J, medical errors created urgency. The institution was stunned when one of its own physicians suffered a medication error while undergoing treatment. This sentinel event spurred the leadership to action.
Leadership
Example 1 At Site D the CEO spoke of engendering an “edgy, impatient culture” around patient care quality. Although QI operations were led by a highly effective physician leader, the CEO remained personally involved, both as a champion for a clinical improvement team (despite not being a clinician) and as a member of the quality integrating committee. The CEO also worked actively behind the scenes to clarify expectations and to resolve problems.
Example 2 At Site F, the full senior leadership team (including the CEO) began each day with patient rounding in which team members asked patients and frontline staff specific questions about their experiences and then engaged in a debriefing session to resolve identified issues. Senior leaders also were required to serve as champions for improvement projects, with responsibility for linking the team to other senior managers who could help to resolve barriers.
Improvement Initiatives
Example 1 Leaders in Site F, for example, found that improvement changes did not stick once special project resources were removed unless the system itself changed. In a surgical infection project, the site initially improved prophylactic antibiotic use through the use of guideline-based reminders and education, but changed its approach after performance plateaued. To reach a zero-defect level, the site re-engineered its practices to provide patients with antibiotics at a specific moment in the preoperative process signaled by explicit physical cues. As a result, the site attained consistently high performance without additional resources.
Example 2 One person in Site F said regarding staff engagement through improvement initiatives, “It was very rewarding to see how excited staff and physicians were about making these changes. It became a competition; it was fun and we celebrated successes, in part by posting the successes… It is part of the ‘pull.’ Doctors, respiratory therapists, etc. travel to all units and communicate ‘what’s doing’ to other units. If it is good, people say ‘why can’t we have that?’”
Alignment
Example 1 The leadership at Site D identified 18 corporate strategies that defined the organization's direction and priorities. Staff members throughout the organization became familiar with these strategies and their meaning.
Example 2 Site I cascaded its organizational objectives to the front line through individual employee goals, with each employee expected to maintain a document containing position-specific goals that were measurable, time-dependent, and aligned with department and organizational goals. To illustrate, a nurse on a patient unit might have an individual goal of responding to patient call requests within y minutes to support the unit goal of improving patient satisfaction scores by x percent to support the organization’s overall patient satisfaction goal.
Integration
Example 1 Some organizations/systems working on medication errors are unable to acquire resources to implement new technologies, such as bar coding, which result in less than fully effective workarounds.
Example 2 Site D redesigned its horizontal management structures to create multidisciplinary groups responsible for care processes defined by patients’ experiences (e.g., inpatient, outpatient, and emergency care teams). In addition, an integration committee staffed by senior leaders, including the CEO, addressed redundancy, conflicts, and the spread of best practices across groups. Site D saw these structures as transitional, recognizing inconsistencies with other structures in the medical center.
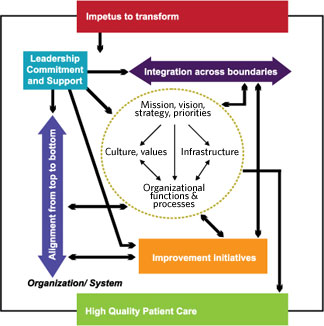
Interaction between Leadership and Impetus
Example 1 In organization J, when there was an error in administration of medication to a member of the medical staff who at the time was an inpatient, leadership organized a task force on patient safety. They developed a videotape describing the error and its consequences, contributing to a climate of transparency and helping to engage leadership and staff in patient safety improvement efforts,
Interaction between Leadership and Improvement Initiatives
Example 1 To maintain leadership involvement in improvement initiatives, senior leaders in Site X participated on every improvement team. This allowed them to remain highly knowledgeable about each team’s work, hold the team accountable, and access resources needed by the team.
Example 2 In site Y, participation in improvement teams was part of each manager’s annual goals and was included in his/her performance evaluation.
Interaction between Improvement Initiatives and Organization/System
Example 1 In Site B, the medication reconciliation project stimulated the development of an online, interactive tool for patient use, and in Site G, work on patient flow triggered the design of an automated bed availability board to facilitate patient movement from the ED to the floor.
Example 2 Site F’s first project involved work with county ambulance staff to improve triage of AMI patients entering the hospital ED. These changes stimulated broader redesign of ED processes for AMI patients, which led, in turn, to redesigned processes for patients coming to the ED with other conditions.
Interaction between Alignment and Improvement Initiatives
Example 1 In site I, the senior leadership recognized that the over one thousand improvement projects that the system had engaged in had not yielded the overall return to the organization commeasurate with resources and effort committed. Upon review they saw that many of the projects were not aligned with the system’s strategy and goals. Some did not get the resources they needed to complete their work, and others were not sustained. Leadership altered its approach to both alignment and improving patient care quality by engaging in a process to clarify its mission, strategy and goals and then strictly selected improvement initiatives that were aligned with its strategy and goals.
Interaction between Alignment and Integration
Example 1 Alignment and integration also interacted with each other. For example, Site D integrated its horizontal management structures around care processes, and defined key priorities that cut across the horizontal management groups. To create alignment, each horizontal group was expected to address for each key priority how the group would contribute to meeting organizational goals and would collaborate with other groups. In our view, study systems that addressed alignment and integration at this level of the organization had a more advanced understanding of the need for consistency and interconnectedness throughout the organization. Even so, these organizations had not perfected an integrative approach. While Site D had been developing its approach for almost two years, it still believed it was a work-in-progress. The evolving integration structures sometimes conflicted or were redundant with traditional structures that remained in place. Patient safety, for instance, was a priority addressed by the horizontal integrating groups, but there was tension with the Patient Safety Committee’s plans.
