
Atherosclerosis
People often think of atherosclerotic disease as a problem that primarily afflicts developed Western countries, but it is a global health problem. It is estimated that 80% of deaths from cardiovascular disease worldwide occur in low-income and middle-income countries. Cardiovascular disease is the number one cause of death worldwide, and it has become the leading cause of death in many developing countries. Cardiovascular disease in developing countries currently claims an estimated 12 billion lives annually, and the toll that it takes continues to climb. The high mortality is partly due to lack of access to care in many areas, but the problem will not be solved by better medical care. In the United States cardiovascular disease continues to claim about 800,000 deaths per year, despite the widespread use of statins to lower cholesterol and angioplasty to open blocked blood vessel.
Atherosclerosis is a complex process by which arteries become progressively narrowed, impairing the supply of oxygen and nutrients to tissues. Impaired blood flow can result in ischemia and cause symptoms such as angina or intermittent claudication. Atherosclerotic plaques can also rupture, triggering acute formation of a clot and an abrupt loss of blood supply to tissues that results in infarction. Eventually, progression of atherosclerosis can manifest itself clinically in three general ways:
After successfully completing this section, the student will be able to:
> The response to injury theory.
> The role of inflammation.
> The role of lipoproteins (LDL).
> The role of smooth muscle cell proliferation.
> The role of clotting of blood.
> The importance of "plaque stability".

The primary function of the heart and blood vessels is to transport oxygen, nutrients, and byproducts of metabolism. Oxygenated and nutrient rich blood is distributed to tissues via the arterial system, which branches into smaller and smaller blood vessels from arteries to arterioles to capillaries (where most exchange occurs). Deoxygenated blood and metabolic byproducts are returned from capillaries via venules and then vein. The heart functions as a pump to maintain circulation. The heart is a discrete organ, which in humans has four distinct chambers. Conceptually, there is the right side of the heart (right atrium and right ventricle) which receive blood returning from the periphery and send it to the lungs (via the pulmonary artery) for re-oxygenation. Once blood is re-oxygenated in the lungs it is returned to the left side of the heart via the pulmonary veins. After entering the left atrium, blood enters the left ventricle and is pumped into the aortic arch for distribution to the entire body. The illustration below provides a schematic representation.
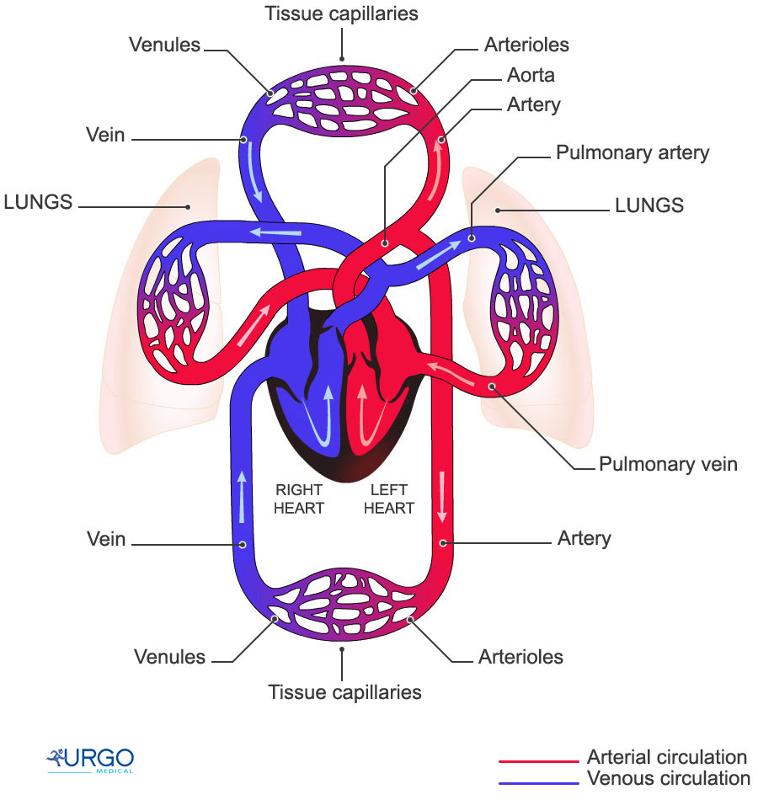
Source: http://humananatomybody.info/neck-arteries-model-labeled/
Note also the the heart is just like any other tissue in that it needs a continuous supply of oxygen and nutrients. The receives its blood supply from coronary arteries, which arise from the root of the aorta. The right and left coronary arteries are shown in the illustration below.
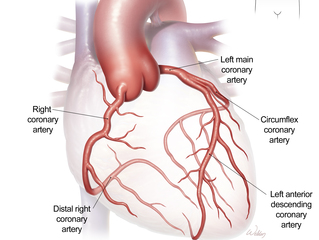
Source: https://www.bcm.edu/healthcare/care-centers/cardiothoracic/procedures/coronary-artery-disease-coronary-bypass
All blood vessels (arteries and veins) have three primary layers: the intima, media, and adventitia. Normally, the walls of an artery are smooth, allowing unobstructed blood flow. The innermost layer of a blood vessel (the intima) is lined with endothelial cells, which are in direct contact with blood. This is shown at the top of the schematic cut-away diagram below.
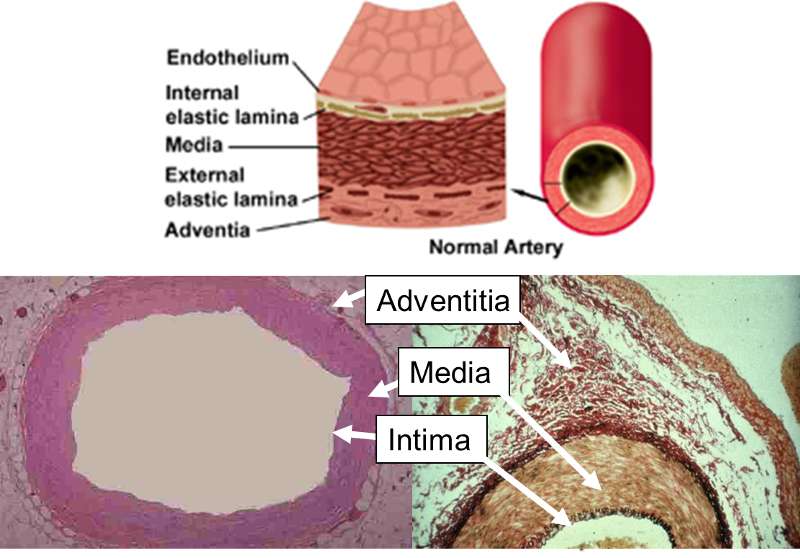
The internal elastic lamina is the barrier between the intima and the underlying media or "tunica media." The media media consists of multiple layers of smooth muscle cells which control the diameter of the blood vessel by contracting or relaxing in response to neural and chemical signals. The outermost layer is the adventia, which consists of connective tissue and also contains nerves and small blood vessels supplying the artery itself.
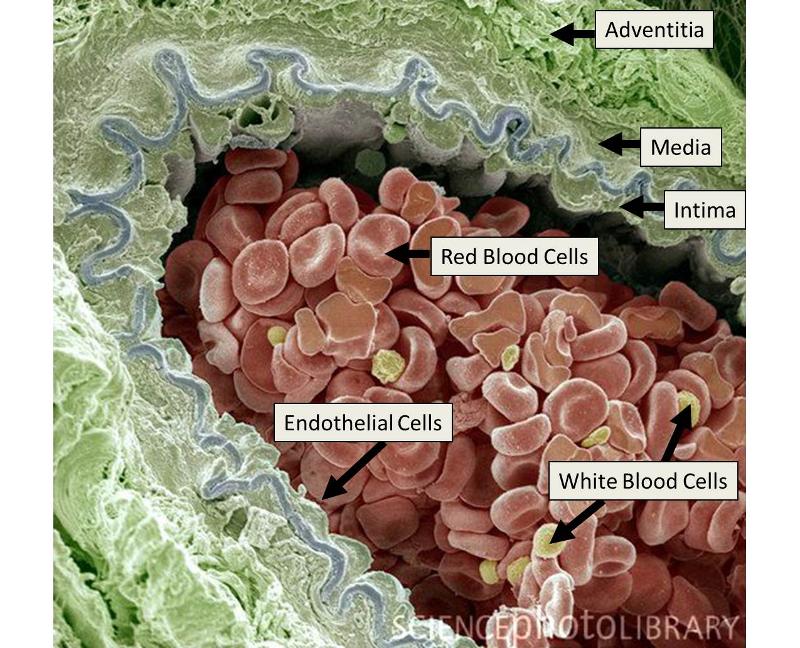
The next image is a scanning electron micrograph of an arteriole showing the layers of the artery and blood cells criculation within the lumen adjacent to the endothelium.
Source: Illustration adapted from: http://www.divingfollonica.com/large-elastic-arteries&page=5
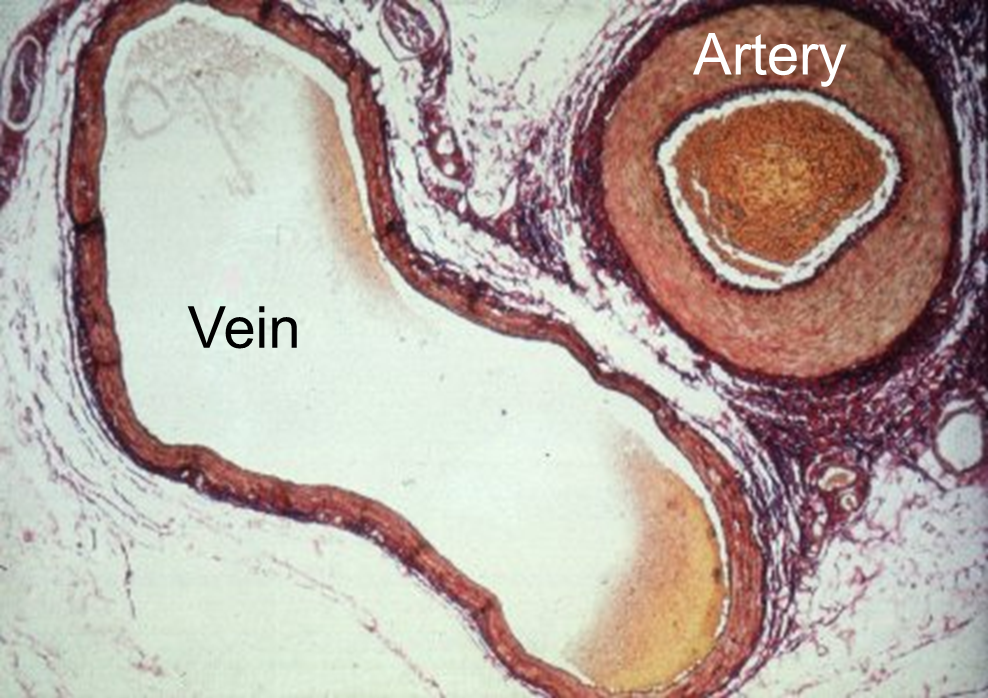
This three layered structure is characteristic of both veins and arteries, but veins have thinner walls, because the media is less developed. The image below provides a comparison of a vein and an artery.
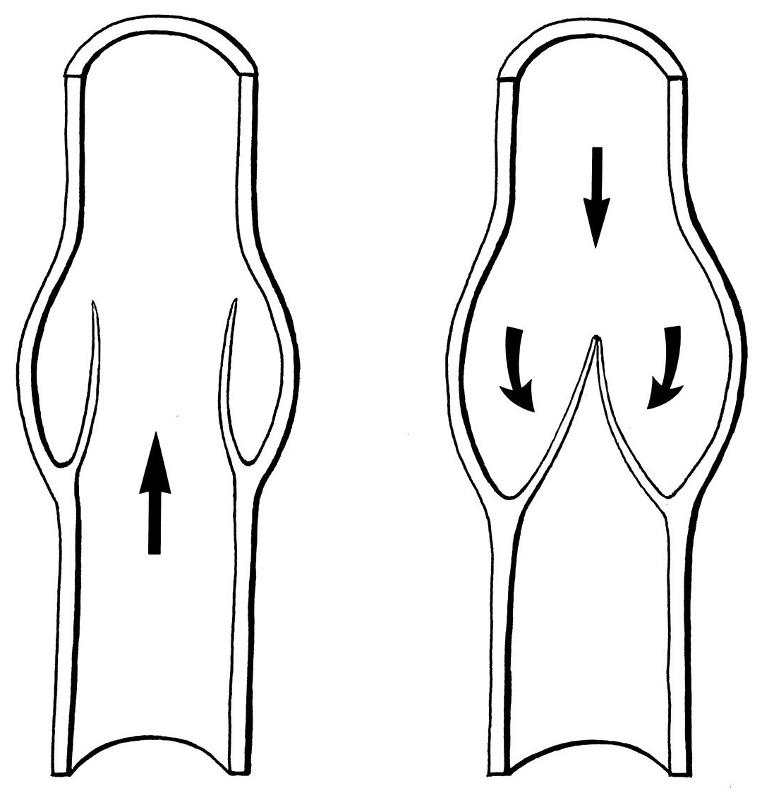
Another difference between arteries and veins is that veins can have internal valves, which help in maintain blood flow back to the heart. Without valves in the veins of the leg, venous blood would tend to pool in the lower leg when standing or sitting. The uni-directional valves (see the drawing on the right) prevent blood from flowing back down.
The endothelial cells that line blood vessels provide an active, dynamic interface between the blood stream and the arterial wall. Their most obvious function is to provide a semi-permeable barrier that regulates the exchange of fluid, nutrients, gases, and waste between the blood and tissues. In addition, endothelial cells regulate a number of other less obvious processes. They provide a unique surface that generally allows the cellular elements of blood to flow without adhering to the vessel lining unless some insult has perturbed the cells. When perturbation occurs, endothelial cells secrete cytokines that trigger and maintain an inflammatory response. Endothelial cells also regulate constriction and relaxation of vessels by releasing vasodilatory molecules (e.g., nitric oxide (NO) and prostacyclin (PGI2) and vasoconstrictive molecules (endothelin and angiotensin-II). [For an excellent review, see Russell Ross: Cell biology of atherosclerosis. Annu. Rev. Physiol. 1995. 57791-804).
Atherosclerosis is a disease process which is triggered by sometimes subtle physical or chemical insults to the endothelial cell layer of arteries. The "Response to Injury Theory" now has widespread acceptance among scientific and medical scholars. This theory holds that the earliest event in atherogenesis is injury to the endothelium, which can be triggered by any number of insults, either alone or in combination. These include:
Under normal conditions, leukocytes in the blood do not adhere to the endothelial cells that line all blood vessels. However, injury to endothelial cells provokes an inflammatory response as illustratedbelow.
Adapted from http://www.nature.com/nature/journal/v420/n6917/fig_tab/nature01323_F1.html
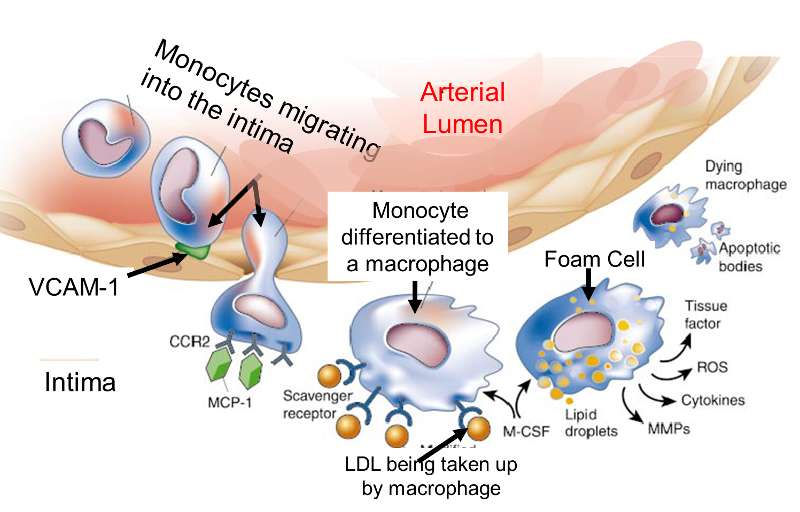
The endothelial cells begin to produce cell surface adhesion molecules such as VCAM-1, causing monocytes and T-lymphocytes to adhere to the endothelium and then migrate beneath it by squeezing between the endothelial cells. Circulating monocytes and T-lymphocytes are attracted to the sites of injury by chemoattractant cytokines (chemokines).
The endothelial cells also change shape, and the tight junctions between endothelial cells loosen, increasing the permeability to fluid, lipids, and leukocytes. Lipoprotein particles, and especially low-density lipoprotein (LDL), enter the arterial wall and undergo oxidation. Oxidation of LDL in the arterial wall occurs as a result of its exposure to nitric oxide, macrophages, and some enzymes such as lipoxygenase. Once they have migrated into the intima, monocytes differentiate into macrophages and begin to take up oxidized LDL that has gotten into the intima. Macrophages retain the lipid they take up, and as they become more lipid-laden, they are referred to as "foam cells." Eventually, the foam cell will undergo apoptosis and die, but the lipid will accumulate in the intima.
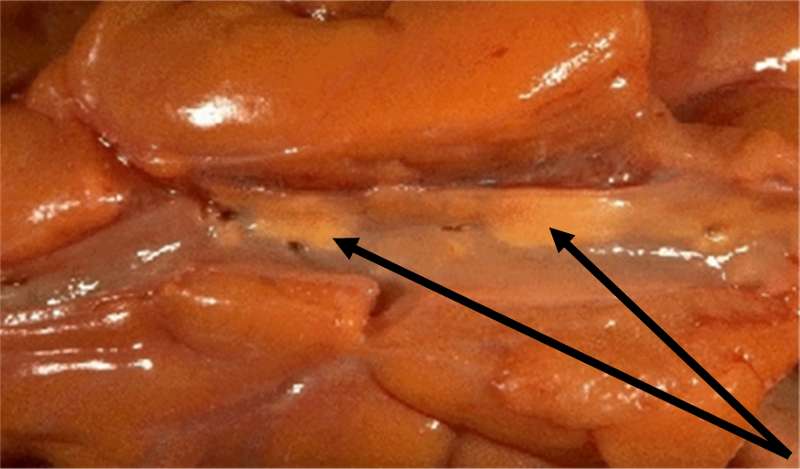
Fatty streaks are the first signs of atherosclerosis that are visible without magnification. They consist of lipid-containing foam cells in the arterial wall just beneath the endothelium. The image below on the left is a photograph of the inside of an artery; one can see two yellowish fatty streaks beneath the thin endothelial lining of the artery. These lesions occur in the aorta and coronary arteries of most people by age 20. Over time, they can evolve into atherosclerotic plaques or they can remain stable or even regress.
Adapted from http://wwwf.imperial.ac.uk/~ajm8/BioFluids/Pictures/
The cartoon below summarizes the steps by which a fatty streak evolves. Injury to the endothelium triggers monocyte adhesion, a loosening of endothelial cell junctions, and migration of monocytes beneath the endolthelium where they differentiate into macrophages. The more permeable endothelium also permits LDL to enter the intima of the artery, and macrophages begin engulfing the LDL by phagocytosis. After macrophages become laden with lipid from ingesting LDL, they are referred to as "foam cells," and collections of these create fatty streaks.
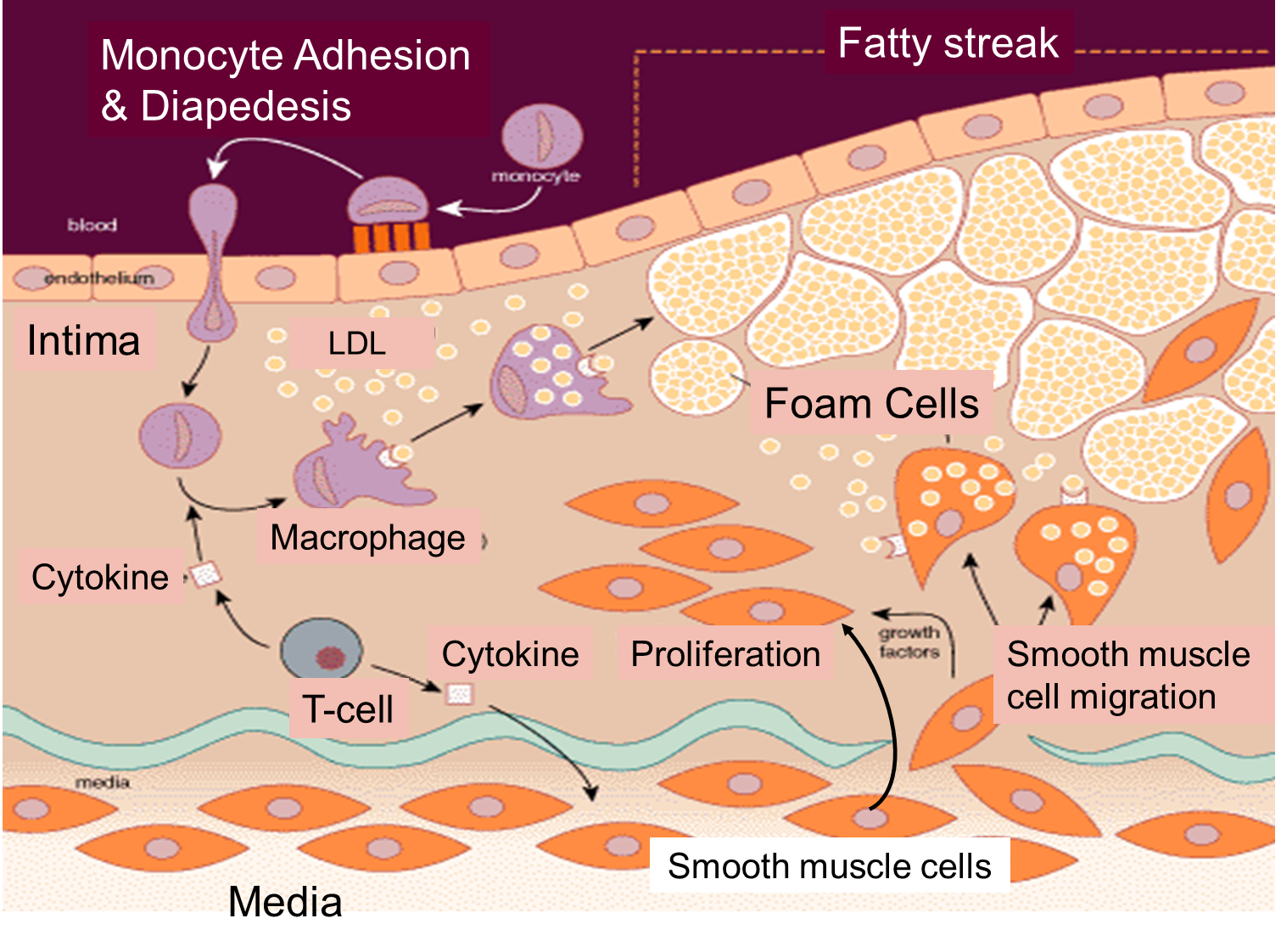
The cartoon also emphasizes the role of T-lymphocytes, which are also in the intima. They secrete cytokines that eventually induce smooth muscle cells to migrate from the media to the intima. These smooth muscle cells also begin to proliferate under the influence of growth factors. Over time there is a progressive accumulation of lipid and smooth muscle cells in the intima, and eventually the growing lesion begins to raise the endothelium and encroach on the lumen of the artery. This is depicted in the image below, which shows a cross-section of an artery at the site of an atherosclerotic plaque.
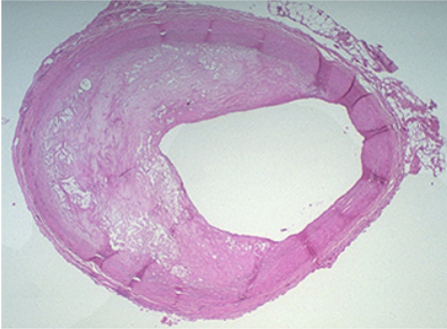
The right side of the artery has a fairly normal appearance, but an atherosclerotic plaque has evolved on the left side. The mass of the "atheroma" is composed of a mixture of lipid and subintimal smooth muscle cells. Note that much of the lumen of the artery is occupied by this growing lesion.
The image below illustrates the evolution of atherosclerotic plaques and also indicates that there are two possible forms of evolution. Slowly growing plaques expand gradually due to accumulation of lipid in foam cells and migration and proliferation of smooth muscle cells. These plaques tend to stabilize and are not prone to rupture. The so-called fibrin cap on the lesion matures. In contrast, other plaques grow more rapidly as a result of more rapid lipid deposition. These have thin fibrin caps that are prone to rupture. Once a plaque ruptures, it can trigger an acute thrombosis (clot) by activating platelets and the clotting cascade.
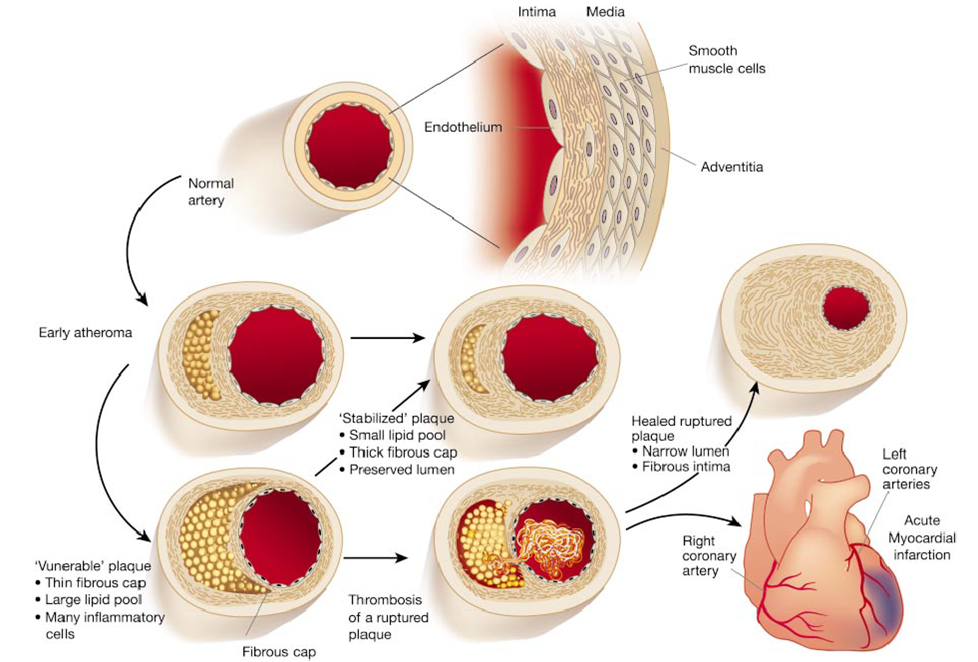
Illustration from from Libby P: Inflammation in Atherosclerosis. Nature 202;420:868
![]()
In its early stages atheroslerotic disease is asymptomatic, but as the condition progresses, blood supply can become increasing compromised as the blood vessels narrow. This can lead to a variety of symptomatic problems, depending on the location of the atherosclerotic plaques. Bear in mind also, that atherosclerosis tends to be a diffuse process; if an individual has evidence of atherosclerosis in one location, they are likely to have blockages at other sites as well.
The three videos below provide additional information on some of the more serious sequelae.
|
Overview of Coronary Artery Disease |
Peripheral Arterial Disease
|
Congestive Heart Failure
|
It is now well-established that the risk of cardiovascular disease and mortality from coronary artery disease is directly correlated with the concentration of cholesterol in blood. The figure below summarizes this relationship in a large group of men from the MRFIT study.

Source: Iso H, et al. N Engl J Med. 1989 Apr 6;320(14):904-10.
|
After an exhaustive review of the available evidence, the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) concluded the following: "Research from experimental animals, laboratory investigations, epidemiology, and genetic forms of hypercholesterolemia indicate that elevated LDL cholesterol is a major cause of CHD. In addition, recent clinical trials robustly show that LDL-lowering therapy reduces risk for CHD. For these reasons, [then panel] continues to identify elevated LDL cholesterol as the primary target of cholesterol-lowering therapy. As a result, the primary goals of therapy and the cut points for initiating treatment are stated in terms of LDL."
|
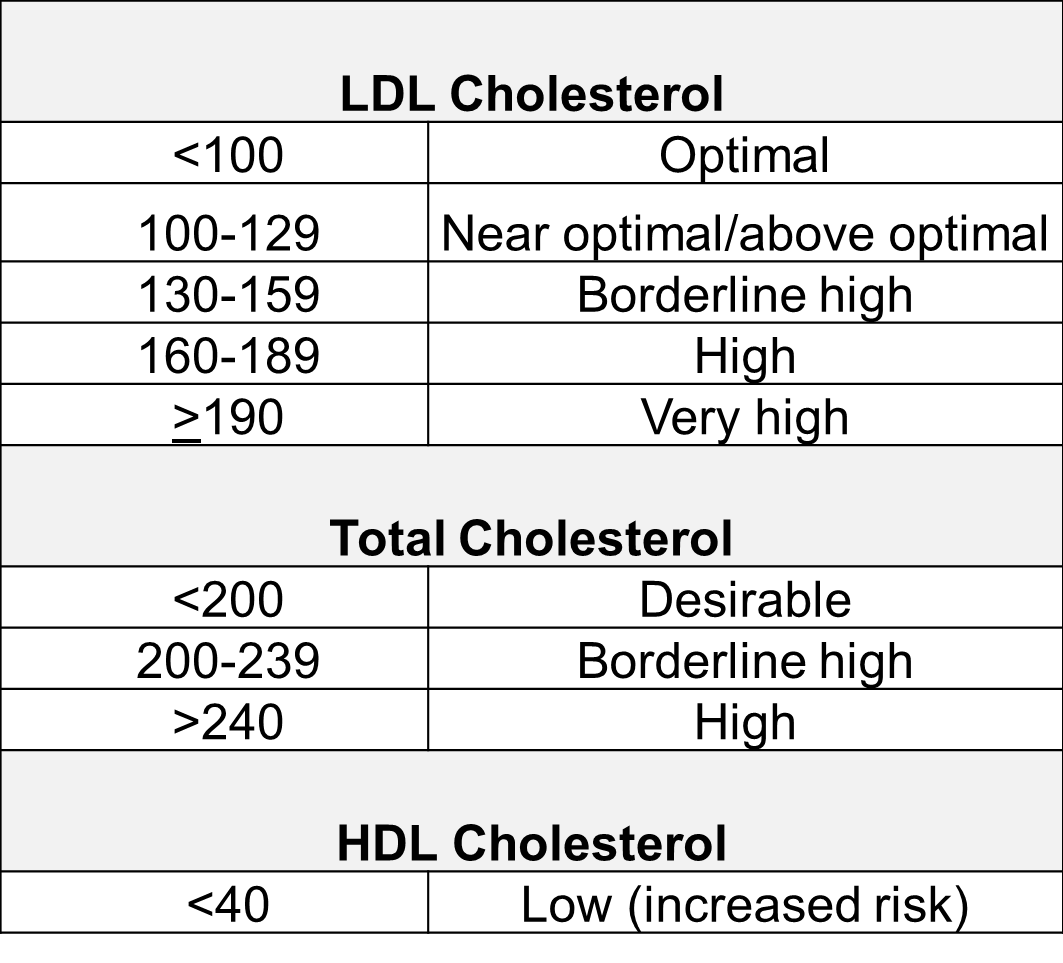
The NCEP panel published the risk classifications based on blood cholesterol concentrations:
The evidence that high LDL concentrations play a causal role in coronary artery disease (CAD)is quite compelling.
Statins are currently the most powerful cholesterol-lowering drugs available. They act by inhibiting the action of 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase, which is the rate-limiting enzyme in the sequence of steps by which cholesterol is synthesized in the liver. The liver has two sources of cholesterol: it can take up LDL particles from the blood, or it can synthesis cholesterol using HMG-CoA reductase. The diagram below illustrates cholesterol homeostasis in a liver cell. LDL (shown in red) can bind to LDL receptors on the surface of the liver.
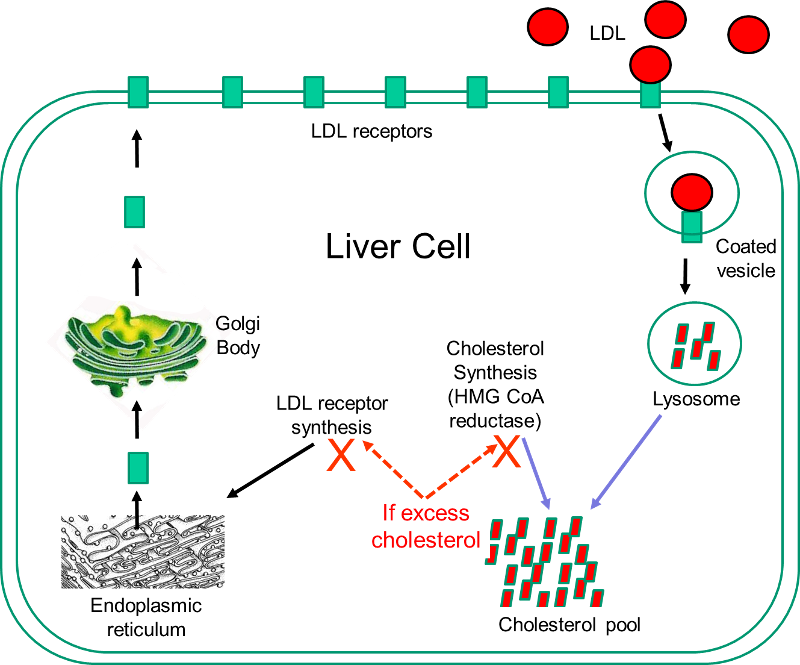
Binding causes the LDL to be taken up by the liver cell and digested in a lysosome. Fatty acids and amino acids in the LDL are recycled, and the cholesterol enters the cholesterol pool in the liver cell. Note that if the liver cell synthesizes cholesterol, this too will be added to the cholesterol pool. If the concentration of cholesterol in the liver cells exceeds a certain level, HMG CoA reductase is inhibited, and the synthesis of LDL receptors is also inhibited.
Statins act by inhibiting HMG-CoA reductase and shutting off internal cholesterol production. In this way, statins reduce cholesterol concentrations in liver cells, which causes increased production of LDL receptors and increased uptake of LDL by the liver. This ultimately results in a lowering of blood concentrations of LDL cholesterol, and this generally results in a slower progression of atherosclerotic plaques and a reduced risk of plaque rupture. However, observers occasionally report regression of atherosclerotic plaques in patient on statins.
While statins are effective in reducing LDL cholesterol levels, they can be associated with side effects.
Because of their effectiveness in reducing CAD in patients at high risk, some advocated expanding the use of statins to people who did not necessarily have elevated cholesterol levels. A number of large, well-done clinical trials have demonstrated that statins can reduce the risk of CAD in low-risk individuals, but most experts caution against this because of the cost and the risk of side effects.
|
Statins for Primary Prevention? From The Cochrane Collaboration
"Reducing high blood cholesterol, a risk factor for cardiovascular disease (CVD) events in people with and without a past history of coronary heart disease (CHD) is an important goal of pharmacotherapy. Statins are the first-choice agents. Previous reviews of the effects of statins have highlighted their benefits in people with coronary artery disease. The case for primary prevention, however, is less clear. Fourteen randomized control trials (16 trial arms; 34,272 participants) were included. Eleven trials recruited patients with specific conditions (raised lipids, diabetes, hypertension, microalbuminuria). All-cause mortality was reduced by statins (RR 0.84, 95% CI 0.73 to 0.96) as was combined fatal and non-fatal CVD endpoints (RR 0.70, 95% CI 0.61 to 0.79). Benefits were also seen in the reduction of revascularisation rates (RR 0.66, 95% CI 0.53 to 0.83). Total cholesterol and LDL cholesterol were reduced in all trials but there was evidence of heterogeneity of effects. There was no clear evidence of any significant harm caused by statin prescription or of effects on patient quality of life. Reductions in all-cause mortality, major vascular events and revascularisations were found with no excess of cancers or muscle pain among people without evidence of cardiovascular disease treated with statins. Other potential adverse events were not reported and some trials included people with cardiovascular disease. Only limited evidence showed that primary prevention with statins may be cost effective and improve patient quality of life. Caution should be taken in prescribing statins for primary prevention among people at low cardiovascular risk."
|
Blood levels of HDL are inversely related to risk of coronary artery disease, and it was thought that low HDL levels represented an independent risk factor. This led to a concerted effort to identify treatments that might prevent CAD by raising HDL concentrations. This area has been very controversial, but recent evidence suggests that although low HDL is inversely correlated with risk of CAD, the relationship is not causal. In other words, low HDL levels are a marker for other factors that cause progression of CAD. Several pieces of evidence suggest this.
How is it possible that low HDL is associated with increased risk, but the relationship is not causal? The most likely answer is that low HDL is a marker for other risk factors that do increase risk. Dr. Sekar Kathiresan, one of the coauthors of the article cited above was quoted in the New York Times as saying that a number of other risk factors track with low HDL, including obesity, being sedentary, smoking, insulin resistance, having small LDL particles, and increased coagulation of blood. Thus, the current thinking is that HDL is not a causal factor, but rather a marker for the presence of other causal factors.
In 1949, Ancel Keys warned of a possible epidemic of obesity that would be caused by a combination of economic and social conditions. Keys said, "While our calorie intake goes up our output goes down. The wonderful advances of technology not merely free us from backbreaking toil; they make it almost impossible to get a decent amount of calorie-using exercise."
Excess body fat is indicative of a metabolic condition that is associated with an increased risk of adverse health events including cardiovascular disease, some cancers, type 2 diabetes, hypertension (high blood pressure), dyslipidemia (for example, high total cholesterol or high levels of triglycerides), stroke, gallstone disease, sleep apnea, and gastroesophageal reflux disease (GERD).
Source: Calle EE, et al.: N Engl J Med 1999; 341:1097-1105
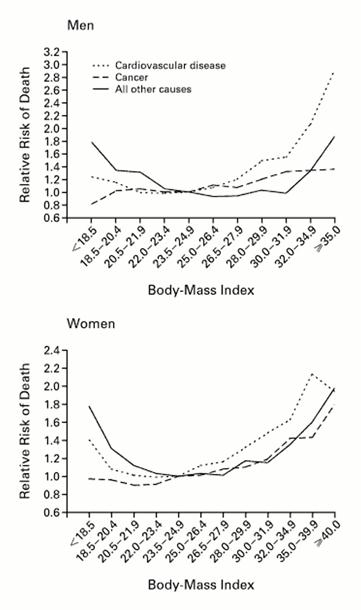
Obesity is most commonly quantified by calculating the body mass index (BMI) which expresses total body weight in kilograms indexed to height (expressed as meters squared). The graphs to the left shows the relationship between BMI and risk of death from cardiovascular disease, cancer, and other causes for a large cohort of men and women. The table below shows the most commonly used classification of obesity based on the BMI in adults.
| BMI |
Classification |
|---|---|
|
Below 18.5 |
Underweight |
|
18.5 – 24.9 |
Normal |
|
25.0 – 29.9 |
Overweight |
|
30.0 and above |
Obese |
You can calculate your BMI using the "widget" below from the CDC.
There has been a dramatic increase in the prevalence of obesity in the United States; it is currently estimated that about a third of adults in the US are obese. Click here http://www.cdc.gov/obesity/data/trends.html to see the prevalence of obesity from 1985 to 2010 through an animated series of maps of the United States. However, the BMI can be misleading, since it does not take into account muscular development or distribution of body fat, and classification of childhood obesity needs to take into account age and gender. For example, "central adiposity," i.e., fat deposition primarily in the torso (the apple-shaped person) is more indicative of an increased risk of cardiovascular disease. This is defined based on measurement of waist circumference, i.e.,
Men - 40 inches or more
Women - 35 inches or more
and central adiposity is one of the criteria for the metabolic syndrome (see below).
For individuals between the ages of 2-20 years of age, classification of obesity uses a nomogram that establishes the individual's percentile of BMI based on age and gender. The figure below shows the nomogram for males and provides several examples for hypothetical boys plotted as shown by the blue dots.
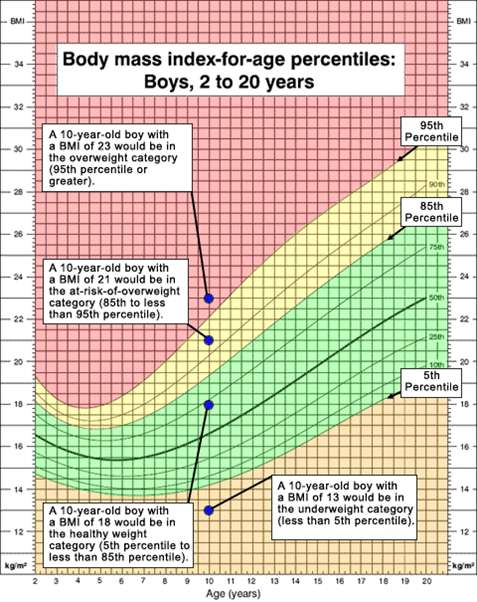
Source: Centers for Disease Control and Prvention
The CDC classifies individuals above the 95th percentile for age and gender as as overweight (The Institute of Medicine would classify these individuals as obese.) Boys who fall between the 85th-95th percentile are classified as "at risk of overweight" by CDC (... and IOM would classify them as overweight). Boys below the 5th percentile are classified as underweight for age.
The Centers for Disease Control (CDC) also have an online "widget" which will calculate results for a child after entering their age, height, and weight.
See http://http://nccd.cdc.gov/dnpabmi/Calculator.aspx
With obesity there is increased delivery of fatty acids to muscle cells, and this leads to the dysfunctional interaction between insulin and its receptors a defect in insulin signaling through insulin receptor substrate. Resistance to insulin leads to generalized insulin resistance and increased release of fatty acids from fat cells. The liver synthesizes and secretes increased amounts of very low-density lipoprotein (VLDL). Exercise reverses these abnormalities by diverting fatty acids in muscle toward mitochondrial oxidation.
In obese individuals, the cardiac workload is greater than in lean people at any level of activity. This is caused by an increased metabolic demand which produces an increment in total blood volume and cardiac output. The increase in cardiac output is attributed to increased stroke volume. Another effect of obesity is seen in an increase in left ventricular filling pressure and volume, which can lead to the production of chamber dilation, a condition that causes increased wall stress and predisposes to an increase in myocardial mass and left ventricular hypertrophy (LVH). Obese individuals also have a further increase in cardiac filling pressures during exercise. Weight reduction causes a decrease in central blood volume, as well as relief of some other conditions that are associated with obesity.
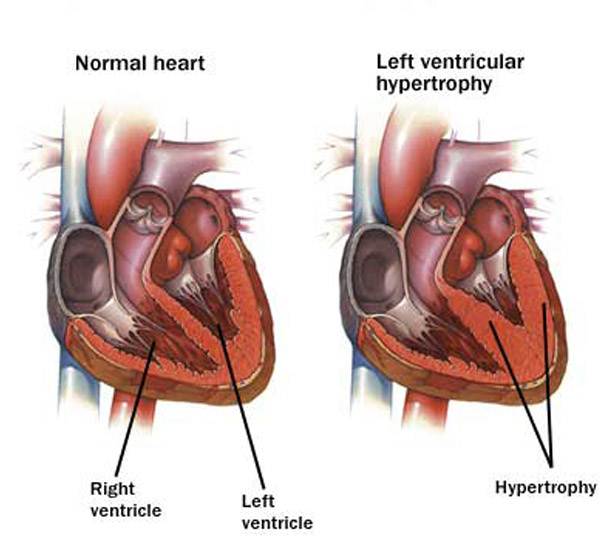
Source: http://epharmapedia.com/diseases/profile/296/Left-ventricular-hypertrophy.html?lang=en
Many individuals have a cluster of risk factors called the metabolic syndrome. These factors include abdominal obesity, atherogenic dyslipidemia (elevated triglyceride, small LDL particles, low HDL cholesterol), raised blood pressure, insulin resistance (with or without glucose intolerance), and prothrombotic and proinflammatory states. Individuals with this constellation of risk factors have an increased risk for coronary artery disease, stroke, and type 2 diabetes. According to the American Heart Association and National Heart, Lung and Blood Institute, metabolic syndrome is present if you have 3 or more of these traits:
An individual with metabolic syndrome has a 1.4 fold increased risk of all-cause mortality and a 2.3-2.8 fold increased risk of cardiovascular death.
Recommendations are similar to those for preventing and treating cardiovascular disease in general:
The Centers for Disease Control and Prevention (CDC) has published a list of community strategies and guidelinesthat can be undertaken to reduce obesity. They can be accessed at this link:
http://www.cdc.gov/obesity/resources/strategies-guidelines.html or in the frame below.
The rise in blood sugar after a meal or snack stimulates the secretion of the hormone insulin from the β-cells in the pancreas. Insulin circulates in the blood and binds to insulin receptors on muscle and fat cells. Binding to the receptor triggers phosphorylation of a protein called 'insulin receptor substrate' or IRS-1. This, in turn, triggers the insertion of specialized glucose transporters (GLUT4) into the cell membrane, where they act as a conduit to facilitate the entry of glucose from the blood stream into the cell. These events are depicted in the image below showing how glucose molecules in a capillary enter a muscle cell.
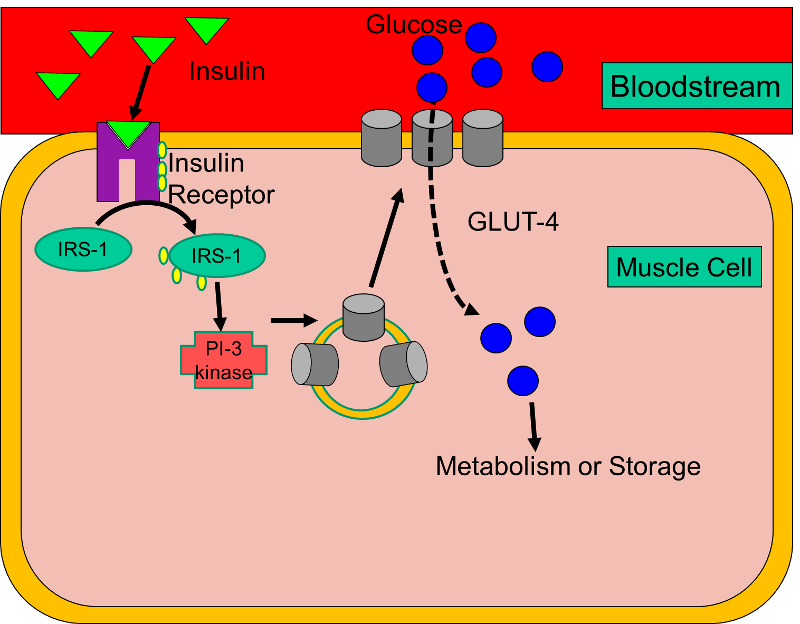
Type I Diabetes (also called insulin-dependent diabetes or juvenile diabetes) results from an autoimmune process that destroys the β-cells, causing a lack of insulin. As a result, glucose cannot enter fat or muscle cells, so blood levels of glucose rise, and there is increasingly greater reliance on breakdown of fat and protein to provide an alternate source of fuel.
In contrast, Type II Diabetes (also known as adult onset diabetes or non-insulin dependent diabetes) is primarily due to insulin resistance. Despite adequate levels of insulin, at least initially, the interaction between insulin and its receptor is dysfunctional. As a result, GLUT4 transporters are not efficiently inserted into the membranes of fat and muscle cells, and glucose concentrations in blood rise (hyperglycemia), leading to endothelial cell dysfunction.
Both type 1 diabetes and type 2 diabetes are independent risk factors for coronary artery disease, and diabetes may predispose to multiple small coronary and peripheral vessels.
The complications of diabetes develop gradually, but they can be disabling and can eventually be fatal. Some of the more prominent complications include:
NOTE: Diabetes is the leading cause of blindness, renal failure, and amputation in the United States.
|
Type 2 Diabetes: A Great, But Unrecognized Risk The excerpts below are from R. Todd Hurst and Richard W. Lee: Increased Incidence of Coronary Atherosclerosis in Type 2 Diabetes Mellitus: Mechanisms and Management. Ann Intern Med. 2003;139:824-834.
"Type 2 diabetes mellitus is a vascular disease. More than 3 out of 4 diabetic patients die of causes related to atherosclerosis, in most cases (75%) because of coronary artery disease. Yet, 70% of diabetic persons do not believe they are at serious risk for cardiovascular disease. An increasing number of patients have diabetes and its attendant complications, and this trend is predicted to continue. In the United States, the number of diabetic patients is expected to increase from 15 million to 22 million by 2025. This increase correlates strongly with increasing obesity and is reflected in the development of diabetes at an earlier age. The younger age at onset portends an increased future prevalence of premature coronary artery disease and resource utilization that will exceed the current $100 billion annual expenditure in the United States. Type 2 diabetes increases the risk for coronary artery disease by 2 to 4 times in the overall population. Haffner and colleagues found that diabetic patients with no history of coronary artery disease have the same risk for future myocardial infarction as do nondiabetic patients with known disease. The National Cholesterol Education Program considers diabetes to be a coronary disease equivalent in their lipid guidelines. The risk is even greater in women. Diabetes eliminates the usual female advantage in risk for death from coronary artery disease; these patients have a 5-fold to 8-fold higher death rate than do nondiabetic women." --------------------------------------------------------------------- [My Comment: Type 2 diabetes represents an enormous public health challenge. It is a highly prevalent condition whose incidence continues to rise with the burgeoning problem of overweight and obesity, and it carries a substantially increased risk of complications and death from a variety of cardiovascular diseases. It presents a rapidly expanding problem that imposes a growing burden of premature disability, death, and cost. One important aspect of the challenge to public health is that it is a condition which is largely preventable by proper nutrition and physical activity. Moreover, even after it occurs, the long range complications can be greatly diminished or delayed by proper management. A second aspect of the public health challenge is that the disease is asymptomatic at first, and many afflicted individuals are unaware that they are affected. The third aspect of the public health challenge, as these authors point out, is that even when diagnosed, the majority do not believe they are at risk and are not taking adequate care to manage their disease./ Wayne LaMorte]
|
Hu, FB, et al: Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001;345:790-7.
This prospective cohort study followed 84,941 female nurses from 1980 to 1996; the subjects were initially free of diagnosed cardiovascular disease, diabetes, and cancer. The investigators defined a "low risk" group based on five characteristics:
After 6 years of follow-up, the study found that overweight or obesity was the single most important predictor of type 2 diabetes. However, "... lack of exercise, a poor diet, current smoking, and abstinence from alcohol use were all associated with a significantly increased risk of diabetes, even after adjustment for the body-mass index. "
Only 3.4% of the women in the cohort met the criteria for being "low-risk." Nevertheless, compared with the rest of the cohort, these low-risk women had a risk ratio of 0.09 (95% confidence interval: 0.05 - 0.17), suggesting that 91% of the cases of type 2 diabetes in the cohort (95% confidence interval: 38-95%) could be attributed to a lifestyle that did not conform to the low-risk criteria. They concluded that the majority of cases of type 2 diabetes could be prevented by the adoption of a healthier lifestyle.
The Diabetes Prevention Trial (The Diabetes Prevention Program (DPP) Trial)
In May 2010 Dr. Francis Collins, Director of the National Institutes of Health, appeared as a witness before the Senate Subcommittee on Labor – HHS – Education Appropriations to support the NIH budget request for FY 2011. Dr. Collins testified:
"For type 2 diabetes, prevention appears to be the name of the game. This form of the disease, which accounts for more than 90% of diabetes among adults, often can be averted or delayed by lifestyle factors. The NIH-funded Diabetes Prevention Program (DPP) trial showed that one the most effective ways to lower the risk of type 2 diabetes is through regular exercise and modest weight loss. There is good reason to believe that such efforts may lead to a lifetime of health benefits. A recent follow-up study of DPP participants found the protective effects of weight loss and exercise persist for at least a decade. The United Health Group has recently announced a partnership with Walgreen's and the YMCA to implement the results of this groundbreaking NIH-funded research on a broad scale."
Tuomilehto J, et al Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 20013441343-50.
A Finnish group conducted a randomized clinical trial to test whether lifestyle changes could prevent type 2 diabetes. The investigators enrolled 522 middle-aged overweight subjects who were pre-diabetic based on glucose tolerance tests.
Subjects in the intervention group lost an average of 4.2 kg of body weight after one year, compared to 0.8 kg in the control group. By the end of the second year average loss in the intervention group was 3.5 kg compared to 0.8 kg in the control group (P<0.001 for both). After four years of follow-up the incidence of diabetes in the intervention group was 11% (95% confidence interval:6-15%), compared to 23% (95% CI: 17-29) in the control group. Moreover, it was shown that the likelihood of prevention of diabetes was directly associated with changes in lifestyle. Consequently, this study shows that type 2 diabetes can be prevented by changes in the lifestyles of high-risk subjects.
An editorial on this report acknowledged that it convincingly showed that type 2 diabetes was delayed in the short term, but raised the question of whether the lifestyle changes could be maintained and how long the reduced incidence of diabetes would last. The editorial comment went on to say that
"... physicians and policymakers may wish to consider whether such intervention programs should be routinely covered by insurance companies and made more broadly available in primary care settings. Such decisions will probably require evidence that the complications of diabetes can be delayed or prevented. It is reasonable to expect, however, that the onset of microvascular complications will be delayed, since the frequency of these complications is closely correlated with the duration of diabetes."
The authors of the editorial concluded by saying:
"At present, the results of the Finnish Diabetes Prevention Study should encourage physicians and other health care providers to persevere in the difficult task of promoting a healthy lifestyle, since by doing so they will give patients a better chance at a life less burdened by many diseases, including type 2 diabetes."
The studies in the previous section focus on the efficacy of lifestyle changes in preventing the development of type II diabetes. A separate but related question is whether lifestyle changes are beneficial in preventing adverse cardiovascular events after type II diabetes has already developed. This question was addressed in a multi-center randomized clinical trial [The Look AHEAD Research Group: Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N. Engl. J. Med. 2013;369:145-54.] Study subjects were overweight or obese. The intervention promoted weight loss through decreased caloric intake and increased physical activity, while the control group received diabetes support and education. During a median follow-up of 9.6 years, the intervention group lost more body weight (8.6% vs. 0.7% after one year; 6.0% vs. 3.5% at study end) and had reductions in glycated hemoglobin levels and increase in fitness. Despite these beneficial changes, the reduction in cardiovascular events in the intervention group was not statistically significant (rate ratio: 0.83; 95% confidence interval 0.83-1.09). The intervention group experienced fewer cardiovascular deaths and fewer myocardial infarctions, but despite a study population consisting of 5,145 subjects, the differences were not statistically significant. Perhaps these findings confirm Benjamin Franklin's adage that "An ounce of prevention is worth a pound of cure."
[See Walter Willett: Dietary Fats and Coronary Heart Disease. J. Intern. Med. 2012; 272: 13–24.]
In the 1970s several observations pointed to a potential relationship between diet and coronary heart disease. The Seven Countries Study by Ancel Keys found that the per capita consumption of dietary cholesterol and saturated fat correlated with mortality from coronary heart disease, and studies in animals also pointed to dietary lipids as a risk factor for atherosclerosis. These studies spawned the widespread recommendations for decreasing dietary cholesterol, decreasing the percentage of dietary calories obtained from fat, and replacing dietary saturated fat with polyunsaturated fat.
Hu F, Stampfer MJ, Manson JE et al. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med 1997;337:1491–9.
This study, using the Nurses' Health Study cohort, analyzed data from 80,082 women free of diagnosed coronary heart disease (CHD) in 1980. Dietary composition for each subject was assessed diet in 1980 using a 61-item food frequency questionnaire, and the assessment was repeated at 4-year intervals. During the subsequent 14 years of follow-up, there were 939 cases of acute myocardial infarction or death from coronary heart disease. For the analysis, the cohort was divided into quintiles for the percentage of energy obtained from each type of fat, and for each type of fat, the rate ratio for each quintile was computed using the group with the lowest intake of a given fat type as the reference. A multivariate analysis was conducted to adjust for age and other confounding variables. A separate analysis used multiple linear regression and treated dietary fat intakes as continuous variables. They then used the coefficients from these models to the estimate the effect of substituting a specific percentage of energy from fat for the same percentage of energy from carbohydrates. The results of these projects are shown in the figure below.

Source: Hu F, et al. N Engl J Med 1997;337:1491–9
In essence, this analysis uses different percentages of carbohydrate intake as a reference (the horizontal purple line) and compares the risk expected with substitution of a given percentage of energy from fat (trans fat, saturated, monounsaturated, or polyunsaturated). Substitution of 5% of carbohydrate energy intake with saturated fat was associated with a 17% increase in the risk of coronary disease (rate ratio, 1.17; 95 % confidence interval, 0.97-1.41; P=0.10). Substitution of 2% of energy from carbohydrates with equivalent calories from trans unsaturated fat was associated with almost a doubling of risk (rate ratio=1.93 (95% confidence interval, 1.43-2.61; P=0.001). Substitution of 5% of energy from monounsaturated fat was associated with a 19% decrease in risk (rate ratio = 0.81 (95% confidence interval, 0.65-1.00; P=0.05). Finally, substitution of 5% of energy from polyunsaturated fat was estimated to be associated with a 38% reduction in risk of coronary heart disease (rate ratio = 0.62 (95% confidence interval, 0.46-0.85; P=0.003). Total fat intake was not significantly related to the risk of coronary disease; for a 5 percent increase in energy from fat versus carbohydrate, the rate ratio was 1.02; 95 percent confidence interval, 0.97-1.07; P=0.55). The authors also estimated that the replacement of 5 percent of energy from saturated fat with energy from unsaturated fats would reduce risk by 42% (95% confidence interval, 23-56; P=0.001) and that the replacement of 2 percent of energy from trans fat with energy from unhydrogenated, unsaturated fats would reduce risk by 53% (95% confidence interval, 34%-67%; P=0.001). The results of this study were largely confirmed in a meta-analysis that included results from 11 cohort studies. The meta-analysis found that the percentage of calories from saturated fat was not associated with higher risk of coronary heart disease when compared to the same percentage of energy from carbohydrates (risk ratio = 0.97, 95% CI 0.81–1.16), but saturated fat was associated with higher risk if compared to polyunsaturated fat (RR = 1.25, 95% CI 1.01–1.56). Like the previous study, it found that the overall percentage of energy from fat was not associated with risk of CHD.
Howard BV, Van Horn L, Hsia J et al. Low-fat dietary pattern and risk of cardiovascular disease the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006;295:655–66.
The Women's Health Initiative conducted a very large randomized clinical trial to examine the effect of a low fat diet on breast cancer and heart disease. The type of fat in the diet was not appreciably altered. A total of 48,000 women were randomly assigned to the low fat diet or their usual diet. The low fat diet had no effect on CHD after an average follow-up of 8 years (RR= 0.97; 95% CI 0.90–1.06) or total cardiovascular disease. This study also found no effect on plasma HDL cholesterol or triglycerides, possibly because of poor adherence resulting in minimal difference in fat intake.
de Lorgeril M, Renaud S, Mamelle N et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 1994;343:1454–9. (The Lion Heart Diet Study)
In Ancel Keys's Seven Countries study a Greek/Mediterranean style diet was associated with the lowest risk of CHD. The Mediterranean diet was mostly vegetarian and consisted of a variety of vegetables, fruits, legumes, nuts, seeds and unrefined cereals. There is high intake of olive oil, but low intake of saturated fat, moderately high intake of fish, low-to-moderate intake of dairy products (mostly cheese or yogurt), low intake of meat and poultry, and regular but moderate intake wine. The inclusion of vegetables, seeds, fish, and olive oil provide a source of omega-3 and monounsaturated fatty acids. The Lyon Diet Heart Study enrolled subjects with known CHD and randomly assigned them to a Mediterranean diet or to an American Heart Association "step 1 diet," which is a low-fat diet (total fat <30% of energy intake; saturated fat <10%). Subjects were followed for 48 months. Remarkably, while the Mediterranean diet had little effect on plasma lipids, these subjects experiences a 70% reduction in CHD events compared to the AHA control diet. Given the multiple differences between the two diets, it was impossible to attribute the benefits to any particular aspect of diet composition.
Dean Ornish has also advocated a multi-pronged approach with lifestyle changes that include low-fat vegetarian food, smoking cessation, regular exercise, and meditation. His findings suggest that adopting this type of lifestyle can not only stop the progression of coronary arterial disease but actually reverse it. The video below is a 15 minute TED talk in which Dr. Ornish summarizes his approach. Note that some of his dietary recommendations differ markedly from the Mediterranean style diet. Two other details are perhaps noteworthy in his talk. First, he recommends reducing dietary fat primarily because fat is calorie dense (9 kcal/gram) compared to carbohydrates or protein (each with 4 kcal/gram). Second, he recommends dietary supplementation with 3 grams of fish oil per day in order to boost omega-3 fatty acids.
The studies described above point to the potential importance of different types of dietary fat. The adipose tissue consists of cells (adipocytes) filled with triglyceride. All triglycerides have the same basic structure and consist of a three carbon glycerol backbone with fatty acids (acyl groups) attached to each of the carbons in the glycerol backbone as illustrated below.
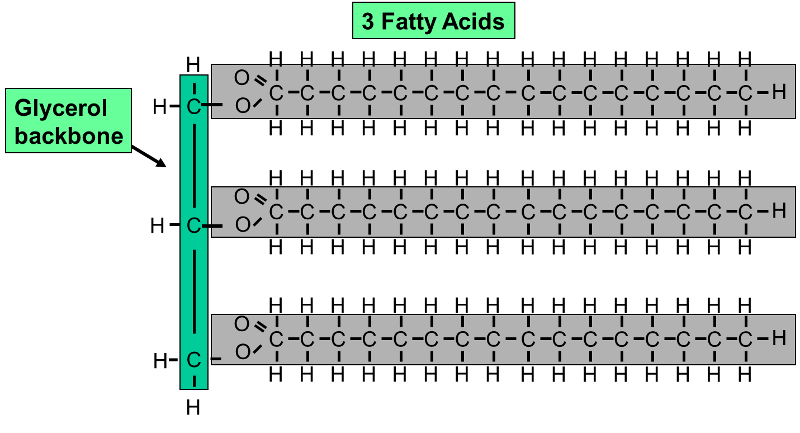
This example shows a triglyceride (fat) molecule with three saturated fatty acids with the same number of carbon atoms in each of the three chains. In reality, there are many "species" of fatty acids which differ in the number of carbon atoms in the acyl chain and the number and location of carbon-carbon double bonds in the acyl chain. Examples of some of the more common naturally occurring fatty acids are shown in the table below.
|
Examples of Different Types of Dietary Fatty Acid and Their Nomenclature |
|
|---|---|
|
Stearic acid, 18:0 is a saturated fatty acid because it has no double bonds between the carbon atoms in the hydrocarbon chain. |
Oleic acid, 18:1, w9 This is the most abundant fatty acid in olive oil. It is monounsaturated and has a cis double bond that produces a kink in the acyl chain. The notation "w9" indicates that it is an omega-9 fatty acid because the double bond is located after the ninth carbon from the methyl end (the left end in this image) |
|
Linoleic acid, 18:2, w6 This is a polyunsaturated fatty acid that is abundant in corn oil. It has two cis double bonds. It is designated "w6", i.e., omega-6 because the first double bond is located after the sixth carbon from the methyl end, which is on the left here. |
Eicosapentaenoic acid, 20:5, w3 EPA is a highly polyunsaturated fatty acid that is found in fish oil from deep water fish like salmon. It is designated "w3", i.e., omega-3 because the first double bond is located after the third carbon from the methyl end, which is on the left here. |
|
Docosahexaenoic acid, 22:6, w3 DHA is also a highly polyunsaturated fatty acid that is found in fish oil from deep water fish like salmon. Like EPA, it is an omega-3 fatty acid because the first double bond is located after the third carbon from the methyl end of the acyl chain, which the on the left here.
|
Source: Mozalfarian, D. et al.: N Engl J Med 2006; 354:1601-1613 These are both monounsaturated fatty acids with 18 carbons in the acyl chain. The fatty acid on the left is oleic acid, which has a cis double bond which characteristically produces a kink in the chain. The fatty acid on the right has a trans double bond which results in a straight chain. |
Triglycerides from naturally occurring sources can have a wide variety of fatty acids, and the table below illustrates some of this variability. It is important to note that none of the fats in the table below consist of just a single species of fatty acid; they are all mixtures.
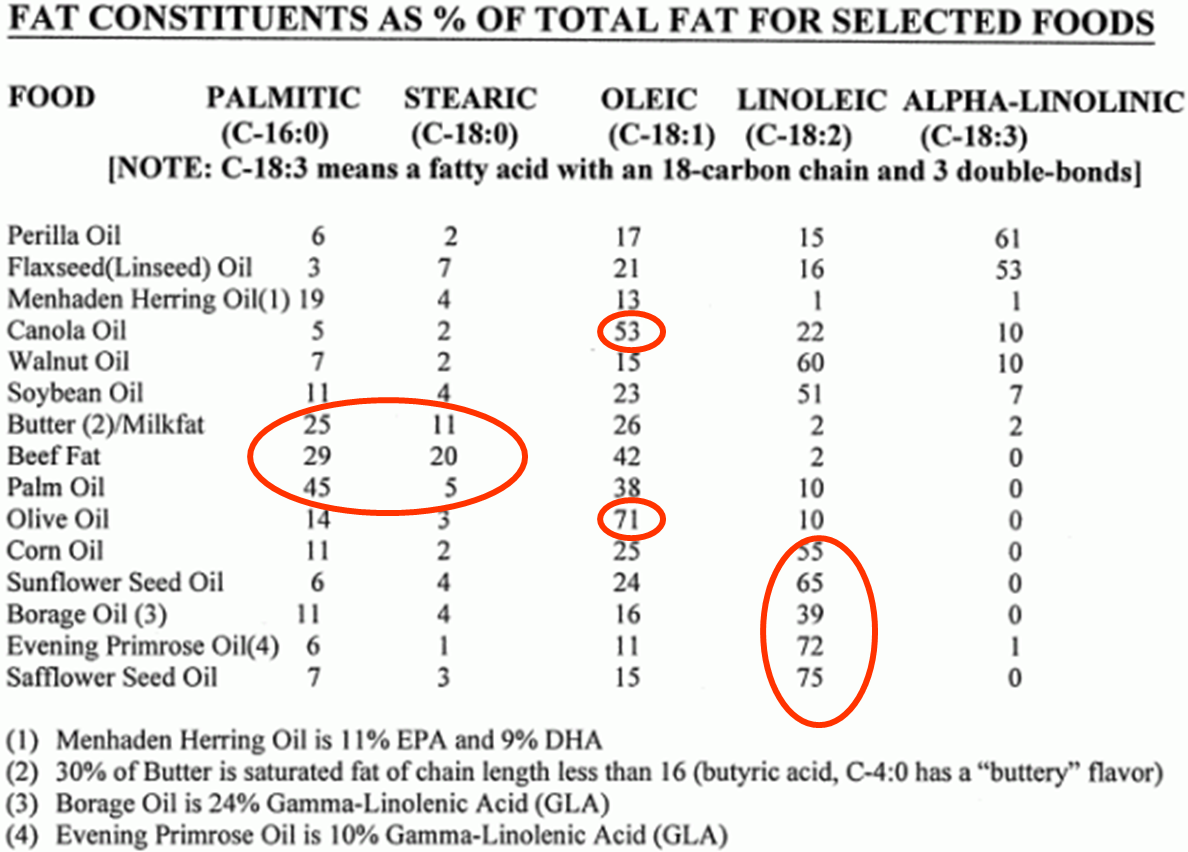
Note in the table that canola oil and olive oil have a very high percentage of oleic acid, a monounsaturated fatty acid with 18 carbon atoms and a single double bond in the 9 position. However, while we refer to canola oil and olive oil as "monounsaturated fats," note that both of them also have some polyunsaturated fatty acids (linoleic and alpha-linolenic) and some saturated fatty acids (palmitic acid and stearic acid). Similarly, corn oil and sunflower oil are referred to as polyunsaturated fats, because they contain a high percentage of linoleic acid. However, these "polyunsaturated fats" also contain lesser amounts of saturated and monounsaturated fatty acids. Fish oil (see Menhaden Herring Oil in the footnote) is sometimes referred to as "highly polyunsaturated," because it has EPA and DHA which have 5 and 6 double bonds in their chains respectively. Nevertheless, note that herring oil contains only 11% EPA and 9% DHA. In addition, fish oil also contains a mixture of saturated, monounsaturated, and polyunsaturated fatty acids. It's just that fish oil has relatively more of the highly unsaturated omega-3 fatty acids than other types of oils.
Many clinicians recommend dietary supplementation with fish oil, but the efficacy of fish oil supplementation remains controversial. Early ecologic studies identified low rates of CHD in Japan and Greenland, which raised the possibility that consumption of fish might be beneficial, possibly by inhibiting platelet adhesion and blood clotting, by reducing blood triglyceride concentrations, or perhaps by reducing arrhythmias. There have been a number of studies that have found beneficial effects, but others that did not. In 1985 Kromhout et al. published the results of a prospective cohort study conducted in Zutphen in the Netherlands. They found an inverse relationship between fish consumption reported in 1960 and the rate of coronary heart disease mortality occurring overt the subsequent 20 years of follow-up. In 2006 Mozaffarian and Rimm conducted a meta-analysis of cohort studies and clinical trials and concluded that a daily intake of 250 mg of EPA and DHA reduced the risk of fatal coronary heart disease by 36%. In 2008 a review of the literature by Artham et al. concluded: ",,, all clinicians should strongly consider therapy with fish oil, specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), for patients with known cardiovascular disease and for patients at increased risk for cardiovascular disease.... The target DHA + EPA consumption levels are about 800 to 1000 mg/d for individuals with known CHD and at least 500 mg/d for individuals without disease." In 2009 Hernando León, et al. conducted a meta-analysis which was published in the British Medical Journal. The subjects were patients who had had a myocardial infarction, or revascularization of implantation of a defibrillator. They concluded, "Fish oil supplementation was associated with a significant reduction in deaths from cardiac causes but had no effect on arrhythmias or all cause mortality. Evidence to recommend an optimal formulation of EPA or DHA to reduce these outcomes is insufficient."
Nevertheless, more recent large trials have failed to confirm the efficacy of fish oil supplementation in high risk patients.
The ORIGIN Trial Investigators n–3 Fatty Acids and Cardiovascular Outcomes in Patients with Dysglycemia. N Engl J Med 2012 367309-318.
This double-blind randomized trial examined the effect of 1 gram of fish oil per day compared to a "placebo" containing 1 gram of olive oil in 12,536 subjects who were at high risk of a cardiac event. All patients had a past history of myocardial infarction, stroke, angina with documented ischemia, or revascularization, and all had marginally abnormal fasting blood sugars. It should be noted that, given their past history of heart disease, all of these subjects were already receiving optimal medical therapy that included medications to control blood pressure, aspirin or other anticoagulant therapy, statins, and smoking cessation counseling.
"During a median follow up of 6.2 years, the incidence of the primary outcome was not significantly decreased among patients receiving n–3 fatty acids, as compared with those receiving placebo (574 patients [9.1%] vs. 581 patients [9.3%]; hazard ratio, 0.98; 95% confidence interval [CI], 0.87 to 1.10; P=0.72). The use of n–3 fatty acids also had no significant effect on the rates of major vascular events (1034 patients [16.5%] vs. 1017 patients [16.3%]; hazard ratio, 1.01; 95% CI, 0.93 to 1.10; P=0.81), death from any cause (951 [15.1%] vs. 964 [15.4%]; hazard ratio, 0.98; 95% CI, 0.89 to 1.07; P=0.63), or death from arrhythmia (288 [4.6%] vs. 259 [4.1%]; hazard ratio, 1.10; 95% CI, 0.93 to 1.30; P=0.26). Triglyceride levels were reduced by 14.5 mg per deciliter (0.16 mmol per liter) more among patients receiving n–3 fatty acids than among those receiving placebo (P<0.001), without a significant effect on other lipids. Adverse effects were similar in the two groups."
Kromhout D, et al.: n–3 Fatty Acids and Cardiovascular Events after Myocardial Infarction. N Engl J Med 2010;363:2015-26.
These investigators conducted a multi-center, double-blind, placebo-controlled trial to examine the effect of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) from fish oil and of the plant-derived alpha-linolenic acid (ALA) in 4837 elderly patients who had already had a myocardial infarction. It should be noted here also that all of these subjects with previously documented heart disease were also receiving state-of-the-art antihypertensive, antithrombotic, and lipid modifying therapy. The investigators formulated four margarines that were supplemented with one of the following: EPA-DHA, ALA, EPA-DHA+ALA, or placebo. They randomly assigned subjects to receive one of the four margarines. The authors found that neither the EPA-DHA supplemented margarine, nor the ALA supplemented margarine reduced the incidence of major coronary events. However, it should also be noted that the actual consumption of the active agents varied depending on consumption of margarine, and the average consumption of EPA-DHA was only 226 mg of EPA and 150 mg of DHA., which is quite low.
Kwak SM, Myung SK, Lee YJ, Seo HG; Korean Meta-analysis Study Group. Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta-analysis of randomized, double-blind, placebo-controlled trials. Arch Intern Med. 2012;172(9):686-94.
In 2012 this study group conducted a meta-analysis of randomized clinical trials examining the effectiveness of fish oil supplementation in patients with known coronary heart disease. They concluded that there was insufficient evidence of a secondary preventive effect of omega-3 fatty acid supplements against overall cardiovascular events among patients with a history of cardiovascular disease.
In the same issue of the Archives of Internal Medicine there was an invited commentary by Dr. Frank Hu and Dr. Joanne Manson from the Department Epidemiology at Harvard School of Public Health:
|
Excerpts from an invited commentary by Frank B. Hu, MD, PhD; JoAnn E. Manson, MD, DrPH in Arch Intern Med. 2012;172(9):694-696 May 14, 2012. "Omega-3 Fatty Acids and Secondary Prevention of Cardiovascular Disease—Is It Just a Fish Tale?: Comment on "Efficacy of Omega-3 Fatty Acid Supplements (Eicosapentaenoic Acid and Docosahexaenoic Acid) in the Secondary Prevention of Cardiovascular Disease" "One question that has been raised is why more recent trials ... have not replicated significant effects of fish oil supplementation on secondary prevention of CVD that were found in earlier trials. Differences in study designs, population characteristics, and types and dosages of omega-3 fatty acids are possible explanations. Most important, the newer trials were each substantially underpowered and unable to detect significant small to modest benefits on CVD outcomes because of their small sample sizes and much lower-than-expected event rates. Another explanation could be that the patients in the more recent trials received much better treatment with statins and antithrombotic and antihypertensive medications than those in earlier trials. The additional benefits of fish oil supplementation or any other therapy on top of statins, β-blockers, angiotensin-converting enzyme inhibitors, and other cardiovascular medications are likely to be small; therefore, a much larger sample size is critical to achieve sufficient power. Another important question is whether fish oil has different effects in primary and secondary prevention of CVD. While waiting for more definitive results, what should physicians tell their patients? To date, there is no conclusive evidence to recommend fish oil supplementation for primary or secondary prevention of CVD. However, a diet high in fatty fish (≥2 servings of marine fish per week) should continue to be recommended for the general population and for patients with existing CVD because fish not only provides omega-3 fatty acids but also may replace less healthy protein sources, such as red meat. Individuals who are unable or unwilling to eat fish or related products should consider increasing their consumption of plant-derived omega-3 fatty acid (α-linolenic acid). For primary or secondary prevention, omega-3 supplementation cannot supersede an overall healthy diet, but a cardioprotective diet needs to be rich in omega-3 fatty acids." |
The failure of the newer trials to replicate the apparent benefits seen in earlier trials may be due to the fact that patients in the newer trials are already receiving optimal medical therapy with statins and antithrombotic and antihypertensive medications, while patients in the earlier trials for secondary prevention were not. This also leaves unanswered the question regarding the efficacy of fish oil for primary prevention of coronary heart disease. Since the incidence of significant cardiac events would be much lower in subjects with no prior history of coronary disease, a randomized clinical trial to test efficacy in these subjects would require a massive sample size and would be prohibitively expensive.
In 2003 Antonia Trichopoulou and colleagues published the results of a prospective cohort study conducted in Greece showing that close adherence to a Mediterranean style diet was associated with a significant reduction in mortality from cardiovascular disease and cancer. Of interest, while the degree of adherence to a Mediterranean diet was associated with reduced mortality, there was no significant association with any particular diet component.
|
Characteristics of the Traditional Mediterranean Diet |
||
|
High Intake of: |
Moderate Intake of: |
Low Intake of: |
|
olive oil, fruit nuts vegetables cereals |
fish poultry wine in moderation with meals |
dairy products red meat processed meats sweets |
More recently, a randomized clinical trial (Estruch et al.: Primary Prevention of Cardiovascular Disease with a Mediterranean Diet, N Engl J Med; online article published Feb, 13, 2013) among subjects at high risk of developing cardiovascul
Trans fats are unsaturated fatty acids with at least one double bond in the trans configuration, as illustrated by elaidic acid in the figure on the right (Source: Mozaffarian D, et al.: Trans fatty acids and cardiovascular disease. N Engl J Med 2006;354:1601-13.) Trans fats are formed by subjecting vegetable oil to a process of "hydrogenation," which was popular in the commercial food industry because of their increased their shelf life, stability during deep fat frying, and their conversion into a semisolid state at room temperature (e.g., margarine). The use of trans fats is increasingly being discouraged, but they were commonly used in fried foods, and in the manufacture of margarines and commercial baked goods, such as donuts, cookies, and crackers.
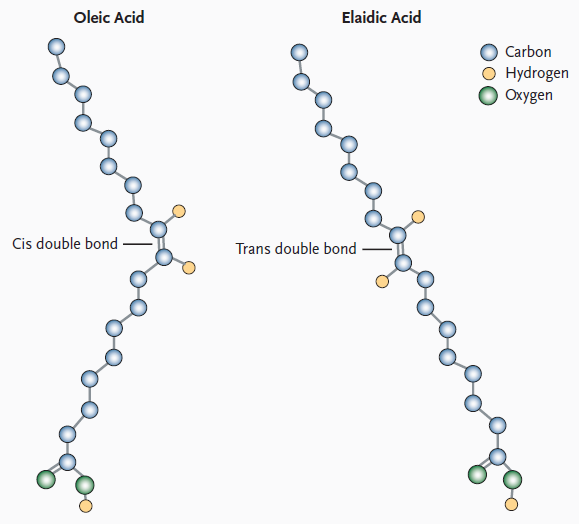
Source: Mozalfarian, D. et al.: N Engl J Med 2006; 354:1601-1613
Trans fats have several adverse effects that increase the risk of coronary heart disease:
The US Food and Drug Administration (FDA) now requires that nutrition labels must indicate the content of trans fatty acids, and the US Department of Agriculture recommends reducing intake of trans fats. The New York City Department of Health and has asked restaurants and food suppliers to stop using partially hydrogenated oils.
Cassidy A, et al.: High Anthocyanin Intake Is Associated With a Reduced Risk of Myocardial Infarction in Young and Middle-Aged Women. Circulation. 2013;127:188-196.
There is growing evidence indicating that dietary flavonoids have a beneficial effect on endothelial function and blood pressure. Flavonoids are believed to improve endothelial function through an anti-inflammatory effects which reduces oxidation of LDL and increased synthesis of nitric oxide in endothelial cells. Flavonoids are found in a variety of plants and can be consumed as fruits, vegetables, tea, and wine.
These researchers used data from the Nurses' Health Study to examine the relationship between anthocyanins and other flavonoids and the risk of MI. Intake of flavonoid subclasses was calculated from validated food-frequency questionnaires collected every 4 years. They found that the highest intake of anthocyanins (upper quintile) was associated with a 32% reduction in risk of CHD (compared to the lowest quintile after adjusting for other risk factors (hazard ratio, 0.68; 95% confidence interval, 0.49–0.96; P=0.03, highest versus lowest quintiles). Combined intake of 2 anthocyanin-rich foods, blueberries and strawberries, tended to be associated with a decreased risk of MI in subjects consuming >3 servings per week (hazard ratio, 0.66; 95% confidence interval, 0.40–1.08). While these finding are intriguing, they will need to be confirmed by randomized clinical trials.
Red meat has been suspected of being a risk factors for heart disease for a number of years, and recent studies have provided evidence for such an association. Bernstein et al. ( Bernstein AM, Sun Q, Hu FB Stampfer MJ, Manson JE, and Willett WC: Major Dietary Protein Sources and Risk of Coronary Heart Disease in Women. Circulation. 2010;122:876-883.) prospectively followed 84,136 women aged 30 to 55 years in the Nurses' Health Study. All women were initially free of known cardiovascular disease for about 26 years. Diet was assessed periodically using a standardized questionnaire. The authors reported that higher intakes of red meat, red meat excluding processed meat, and high-fat dairy were significantly associated with elevated risk of CHD, while higher intakes of poultry, fish, and nuts were significantly associated with lower risk.
A subsequent study from Boston University School of Public Health (Ashaye A, Gaziano J, Djoussé L: Red meat consumption and risk of heart failure in male physicians. Nutr Metab Cardiovasc Dis. 2011 Dec;21(12):941-6.) reached a similar conclusion in a cohort of male physicians. Men in the highest quintile for red meat consumption had a 24% increase in risk of heart failure compared to men in the lowest quintile of consumption (risk ratio: 1.24; 95% confidence limits, 1.03-1.48.
Other recent studies suggest that the association between consumption of red meat and heart disease may be related to the metabolism of dietary choline and carnitine in the human intestine. Phoshatidylcholines (lecithins) are a family of phospholipids that are important components of all cell membranes, and dietary phosphatidylcholine the major dietary source of choline, which has several metabolic roles besides being a major component of cell membranes. It is involved in lipid metabolism and it is a precursor for the synthesis of the neurotransmitter acetylcholine. Intestinal microbial organisms (microbiota) metabolize dietary choline to trimethylamine (TMA), which is then absorbed by the intestine and tranported to the liver, where it is converted into timethylamine-N-oxide (TMAO). TMAO is believed to promote atherosclerosis by promoting the transformation of macrophages into foam cells and fostering the deposition of cholesterol in arterial lesions.
A 2013 publication in the New England Journal of Medicine provided evidence for the conversion of dietary choline to TMAO by gut microbes. [Tang WH, Wang Z, et al.: Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013 Apr 25;368(17):1575-84.] These investigators had healthy subject eat two hard-boiled eggs as a source of phosphatidylcholine and measured TMAO production. Plasma levels of TMAO increased after ingestion of the eggs, but TMAO production was markedly suppressed when broad spectrum antibiotics were given to reduce gut bacteria. These investigators also studied the relationship between fasting plasma levels of TMAO and incident cardiovascular events (death, myocardial infarction, or stroke) during 3 years of follow-up in 4007 patients undergoing elective coronary angiography. Increased plasma levels of TMAO were associated with an increased risk of cardiovascular disease even after adjustment for other know risk factors (hazard ratio = 2.54 for the highest TMAO quartile compared to the lowest; 95% confidence interval: 1.96 to 3.28; P<0.001). They concluded that production of TMAO from dietary phosphatidylcholine is dependent on metabolism by the intestinal microbiota, and that increased TMAO levels are associated with an increased risk of incident major adverse cardiovascular events.
Another recent study [Koeth RA, Wang Z, et al.: [Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013 May;19(5):576-85] provided evidence that dietary carnitine, which is abundant in red meat, can also be converted to TMAO by intestinal microbes. They found that omnivorous human subjects produced more TMAO than vegans or vegetarians after ingestion of L-carnitine. They found that specific types of gut bacteria were associated with both plasma TMAO concentration and dietary status. Moreover, higher plasma L-carnitine concentrations were found in patients with known heart disease, and higher levels of carnitine were also associated with an increased incidence of subsequent cardiovascular events (myocardial infarction, stroke or death) in 2,595 subjects who were followed after cardia evaluation . Studies in mice have shown that chronic dietary L-carnitine supplementation altered gut microbial composition and dramatically increased formation of TMA and TMAO, and increased atherosclerosis. However, this did not occur if intestinal microbe populations were suppressed by administration of broad spectrum antibiotics.
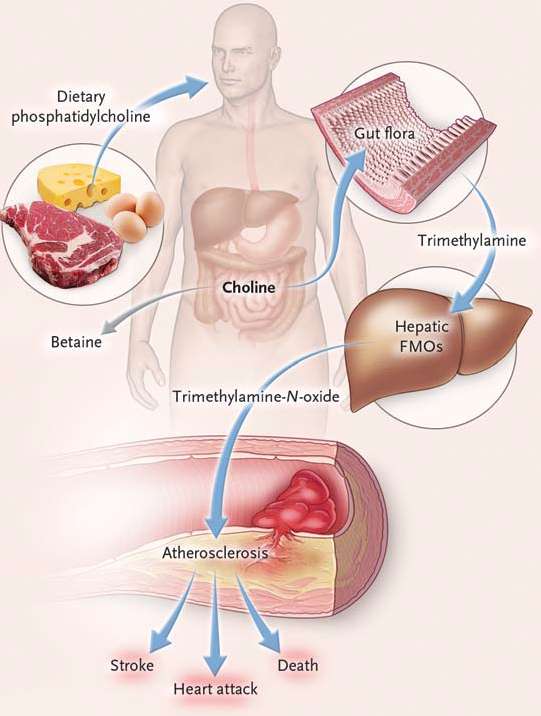
Source: Tang, WHW, et al.: N. Engl. J. Med. 2013;368:1575-1584.
TMAO production is also influenced by genetic factors. Taken together, these observations provide evidence of a complex interaction among humans, their resident gut flora, and environmental and behavioral factors (diet). Moreover, these newer observations raise the possibility of new interventions, e.g., by modifying diet to reduce consumption of L-carnitine and phosphatidylcholine, by modifying gut flora via antibiotics or probiotics, or by inhibiting the synthesis of TMAO pharmacologically. It is advisable to limit red meat consumption and to avoid lecithin (phosphatidlycholine) supplements (which are sold as tablets in drug stores and "health food stores."
Note that these recommendations do not include specific recommendations based on some of the newest scientific evidence cited above.
|
American Heart Association Recommendations |
|---|
|
As part of a healthy diet, an adult consuming 2,000 calories daily should aim for:
Other Dietary Measures:
|
Several well done studies have demonstrated substantial benefits of exercise in reducing the risk of coronary heart disease.
Manson J, et al: A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. N Engl J Med 1999;341:650-8.
In this prospective cohort study Manson and her colleagues examined the association physical activity and coronary heart disease events in 72,488 female nurses who were 40 to 65 years old in 1986 and who had no know heart disease or cancer at the beginning of the observation period. Detailed information on physical activity was first collected in 1986 and was updated in 1988 and 1992. Participants were asked to report the average amount of time spent per week during the previous year on a wide variety of physical activities, and they used this information to calculate a "MET-hr/week" expenditure of energy, and they divided the cohort into quintiles based on their physical acclivity. During the subsequent 8 years of follow-up, there were 645 incident coronary events (nonfatal myocardial infarction or death from coronary disease). The table below summarizes their findings.
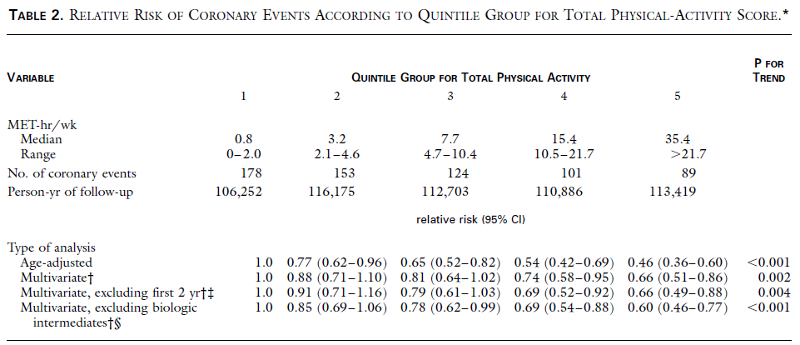
The rate ratio for each quintile was calculated using the incidence rate in the less active women (quintile #1) as the reference group. The 95% confidence interval for each rate ratio is shown in parentheses. The table demonstrates that there was an inverse relationship between activity and coronary events, and there was a clear biologic gradient. a strong, graded inverse association between physical activity and the risk of coronary events. The second multivariate analysis, which was adjusted for many risk factors for coronary disease, showed that, compared to the least active quintile, women with progressively greater activity had rate ratios of 0.88, 0.81, 0.74, and 0.66. For example, women who exercised even moderately (quintile #3) had almost a 20% reduction in risk of a severe coronary event (death or infarction). The authors further stated:
"Walking was inversely associated with the risk of coronary events; women in the highest quintile group for walking, who walked the equivalent of three or more hours per week at a brisk pace, had a multivariate relative risk of 0.65 (95 percent confidence interval, 0.47 to 0.91) as compared with women who walked infrequently. Regular vigorous exercise (»6 MET) was associated with similar risk reductions (30 to 40 percent). Sedentary women who became active in middle adulthood or later had a lower risk of coronary events than their counterparts who remained sedentary."
The authors concluded that "brisk walking and vigorous exercise are associated with substantial and similar reductions in the incidence of coronary events among women." They further stated, "These findings lend further support to current federal exercise guidelines, which endorse moderate intensity exercise for at least 30 minutes on most (preferably all) days of the week. Our results suggest that such a regimen (e.g., brisk walking for three or more hours per week) could reduce the risk of coronary events in women by 30 to 40 percent. Increasing walking time or combining walking with vigorous exercise appears to be associated with even greater risk reductions. Given the high prevalence in the United States of a sedentary lifestyle (78 percent of adults engage in less physical activity than currently recommended), we estimate, on the basis of our multivariate relative-risk analyses, that one third of coronary events among middle-aged women in the United States are attributable to physical inactivity."
Hu FB, et al: Adiposity as Compared with Physical Activity in Predicting Mortality among Women. N Engl J Med 2004;351:2694-703.
These authors used the Nurses' Health Study to examine the associations of BMI and physical activity with death among 116,564 women. They found that higher levels of physical activity reduced the risk of death at all levels of obesity, but but did not eliminate the adverse effect of obesity. Compared to women who were lean (BMI< 25) and active (exercising 3.5 or more hrs/week), the adjusted rate ratios were:
They concluded that both obesity and reduced physical activity are strong and independent predictors for death. Moreover, they estimated that BMI>25 and physical inactivity (weekly exercise <3.5 hours) together could account for 31 % of all premature deaths, 59% of deaths from cardiovascular disease, and 21% of deaths from cancer among nonsmoking women.
Blood pressure is a measure of the force of blood pushing against the arterial walls as the heart pumps blood around the body. Blood pressure is highest when the heart contracts (systole), and falls when the heart is relaxing and refilling (diastole), and pressures in the arteries during these alternating phases are referred to as systolic and diastolic pressures. The figure below shows changes in pressure within large arteries during a single cardiac cycle of contraction and relaxation.
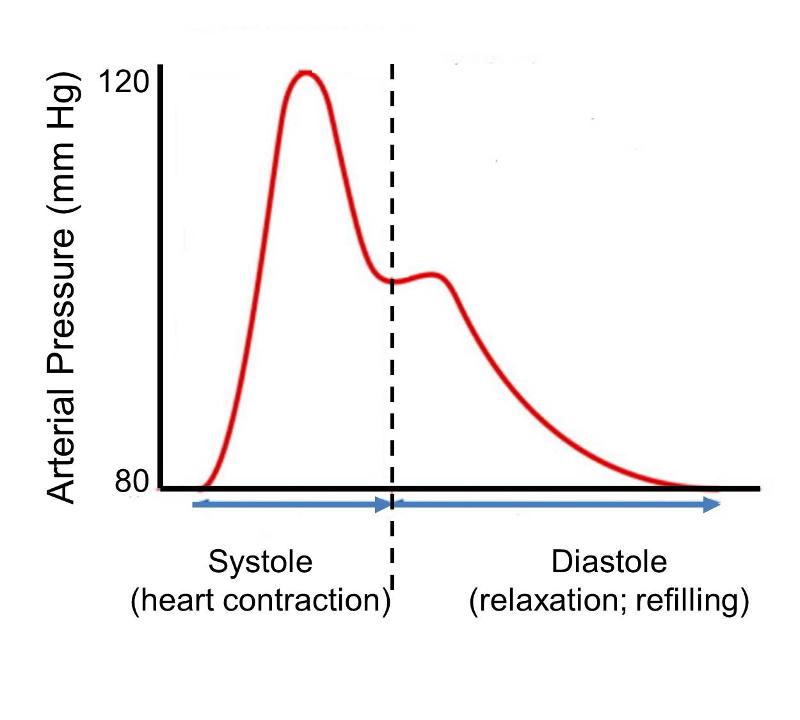
Systolic and diastolic blood pressures vary continually depending on activity and many other factors, and the range of observed pressures vary among individuals. Nevertheless, the image depicts a steeotypic normal adult with minimum diastolic pressure of 80 mm of mercury and a peak systolic pressure of 120 mm of mercury. At the and of diastole the pressure is 80. As systolic contraction begins arterial pressure rises rapidly to a peak of 120 in mid systole and then falls to about 105 by the end of systole. During diastole, when the heart relaxes, pressure declines back to 80 mm of mercury. The small secondary pressure increase in the beginning of diastole is referred to as the 'dicrotic notch' and is due to closure of the aortic valve and elastic recoil of the aortic wall. The pulse pressure depicted here indicates an arterial blood pressure of 120/80, i.e., the first number indicates peak systolic pressure, and the second indicates pressure at the end of diastole. The National Heart, Lung, and Blood Institute defines normal blood pressure at rest as 120/80 or lower. Individuals with resting blood pressures that are consistently greater than 140/90 are considered to have hypertension (high blood pressure). Hypertension leads to endothelium dysfunction. The longer hypertension goes untreated, the more damage it can cause.
Hypertension affects almost 50 million people in the US. Clinical trials have demonstrated that a diet emphasizing fruits, vegetables, low-fat dairy products, whole grains, poultry, fish, and nuts with reductions in red meat, sugar, and total and saturated fat and cholesterol lowers blood pressure in people with and without hypertension. Reducing the sodium chloride content of typical diets in the US or Europe lowers blood pressure.
Facts About Hypertension from the CDC
From a public health perspective high blood pressure is an enormous problem that presents a real opportunity for low-cost, high-impact intervention. Hypertension is highly prevalent and substantially under diagnosed. Moreover, it contributes very significantly to atherosclerotic disease and stroke. Nevertheless, it is an ideal condition for screening, and it can be effectively treated by behavior modification and/or low-cost medication.
Smoking increases the risk of atherosclerosis, because components of tobacco smoke generate reactive oxygen species and reduce antioxidants, which causes endothelial dysfunction. Smoking tobacco in any form will have the effect of increasing LDL cholesterol, decreasing HDL cholesterol, and slightly increasing triglycerides. This negatively affects all of the cholesterol levels in the body.
Cholesterol has a direct correlation with atherosclerosis. Nicotine not only causes addiction to smoking cigarettes, but also has a negative effect on the arteries. Nicotine speeds up the heart, raises blood pressure, and constricts the arteries. Carbon monoxide minimizes the oxygen supply that travels to the heart. Both nicotine and carbon monoxide also increase blood clotting and clogging of the arteries.
Smoking accelerates the process of atherosclerosis. Each time a person smokes a cigarette, the blood vessels become sticky from the chemicals in the tobacco smoke, which leads to fat collecting and sticking to the artery walls. Smoking decreases a person's tolerance to exercise, which would help keep the heart strong. It also increases the tendency for the blood to clot due to an increase in the levels of fibrinogen, a protein that can cause the blood to clot. Smoking facilitates the progression of atherosclerosis, which leads to most of the other cardiovascular diseases and coronary heart diseases.
(See Heart Disease in Women - Harvard Medical School)
Years ago it was believed that women had less risk of coronary artery disease than men, but we now know that the risk is similar, although women tend to develop heart disease about 10 years later than men. The table below shows age-specific mortality from coronary artery disease in men and women.
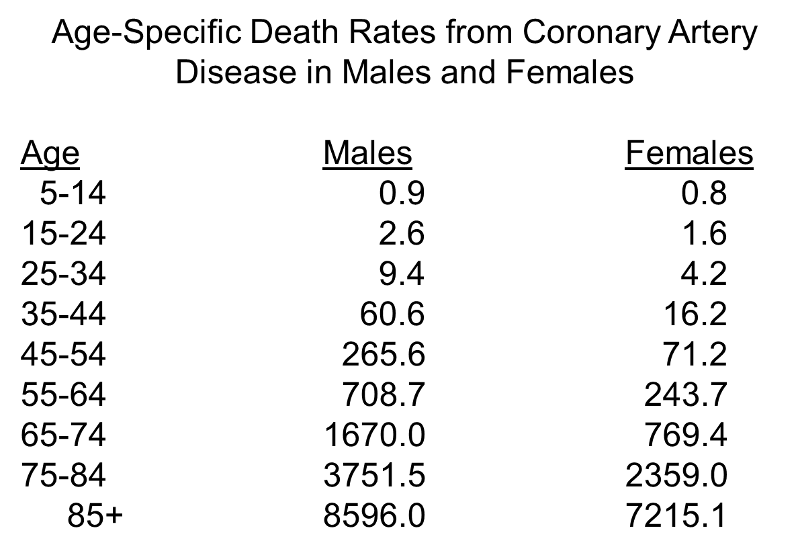
Note, first, the progressive increase in risk with increasing age. The initial age-related increase is greater in men, but after menopause in women (mostly during the 6th decade), the rate in women increases and they begin to catch up to men.
Estrogens give women a somewhat more favorable lipid profile before menopause by increasing HDL (good) cholesterol and decreasing LDL (bad) cholesterol. After menopause, however, women have higher concentrations of total cholesterol than men, and elevated triglycerides become an important risk factor in women, particularly over age 65.
Another important difference is that women frequently don't experience the classic chest pressure and crushing chest pain that often occurs in men. Instead, they may report extreme fatigue or shortness of breath, or they may have nausea or abdominal, neck, or shoulder pain.
Almost all of the epidemiologic studies that have examined this issue have concluded that moderate alcohol consumption is associated with a 20-40% lower incidence of coronary artery disease and lower risk of mortality from coronary artery disease compared to non-drinkers or heavy drinkers. A number of large prospective cohort studies have demonstrated that moderate drinking lowers the risk of coronary heart disease.
Mukamal KJ, et al.:Roles of Drinking Pattern and Type of Alcohol Consumed in Coronary Heart Disease in Men. N Engl J Med 2003;348:109-18.
This prospective cohort study used The Health Professionals Follow-up Study, which included 51,529 U.S. male dentists, veterinarians, optometrists, osteopathic physicians, and podiatrists 40 to 75 years of age who have been followed since 1986. In 1986 the subjects were asked to report the number of days per week that they typically drank any alcohol, with five response categories. This study included 38,077 men who did not have any history of coronary heart disease in 1986. After 12 years of follow-up, there were 1418 cases of myocardial infarction. The abstract for the report states:
"As compared with men who consumed alcohol less than once per week, men who consumed alcohol three to four or five to seven days per week had decreased risks of myocardial infarction (multivariate relative risk, 0.68 [95 percent confidence interval, 0.55 to 0.84] and 0.63 [95 percent confidence interval, 0.54 to 0.74], respectively). The risk was similar among men who consumed less than 10 g of alcohol per drinking day and those who consumed 30 g or more. No single type of beverage conferred additional benefit, nor did consumption with meals. A 12.5-g increase in daily alcohol consumption over a four-year follow-up period was associated with a relative risk of myocardial infarction of 0.78 (95 percent confidence interval, 0.62 to 0.99)."
A meta-analysis by Ronksley PE, et al. found that light to moderate alcohol consumption was associated with a reduced risk of cardiovascular disease. Relative to non-drinkers, alcohol drinkers had a rate ratio of 0.75 (95% confidence interval 0.70 - 0.80) for cardiovascular disease mortality (21 studies), 0.71 (0.66 - 0.77) for incident coronary heart disease (29 studies), 0.75 (0.68 to 0.81) for coronary heart disease mortality (31 studies), 0.98 (0.91 - 1.06) for incident stroke (17 studies), and 1.06 (0.91 - 1.23) for stroke mortality (10 studies). Their analysis suggested that the lowest risk of mortality from coronary heart disease occurred with 1-2 drinks a day, while the lowest risk for stroke occurred with ≤1 drink per day. Most other large prospective investigations have also found that moderate drinking is associated with lower risk for coronary heart disease.
An negative association between moderate drinking and lower risk for CHD does not necessarily mean that alcohol itself is the cause of the lower risk. There is always the possibility that residue confounding may be responsible for an apparent beneficial effect. For example, few studies have adjusted for subjects' levels of physical activity, despite evidence physically active people tend to drink more more frequently, and exercise protects against CHD occurrence and mortality. In addition, those who drink wine may be generally more health conscious and follow a more favorable lifestyle.

Final report on the aspirin component of the ongoing Physicians' Health Study. Steering Committee of the Physicians' Health Study Research Group. N Engl J Med. 1989;321(3):129-35.
In the middle of the 20th century a number of descriptive studies suggested that people who took aspirin regularly seemed to have a lower risk of myocardial infarction. Subsequent observational studies suggested perhaps a 30% reduction in risk of myocardial infarction, but there were concerns about confounding. Several small clinical trials suggested similar reductions, but the sample sizes were too small to arrive at a solid conclusion. In the early 1980s The Physician's Health Study was conducted to test the hypothesis that 325 mg. of aspirin (one 'adult' sized aspirin, i.e., 325 mg) taken every other day would reduce mortality from cardiovascular disease (N. Engl. J. Med. 320:1238, 1989). Male physicians 40 to 84 years of age living in the US in 1980 were eligible to participate. Physicians were excluded if they had a personal history of myocardial infarction, stroke or transient ischemic attack; peptic ulcer disease; contraindication to aspirin consumption; current use of aspirin, platelet-active drugs or non-steroidal anti-inflammatory agents; intolerance to aspirin; or inability to comply with the protocol. Eligible subjects who met the inclusion criteria and who successfully completed a run-in phase were randomly assigned to receive aspirin or a placebo. Eventually 22,071 physicians were enrolled; 11,037 were assigned to aspirin, and 11,034 were assigned to placebo. The agents (aspirin and placebo) were identical in appearance and were mailed to the subjects.
From the abstract of the final report:
"There was a 44 percent reduction in the risk of myocardial infarction (relative risk, 0.56; 95 percent confidence interval, 0.45 to 0.70; P less than 0.00001) in the aspirin group (254.8 per 100,000 per year as compared with 439.7 in the placebo group). A slightly increased risk of stroke among those taking aspirin was not statistically significant; this trend was observed primarily in the subgroup with hemorrhagic stroke (relative risk, 2.14; 95 percent confidence interval, 0.96 to 4.77; P = 0.06). No reduction in mortality from all cardiovascular causes was associated with aspirin (relative risk, 0.96; 95 percent confidence interval, 0.60 to 1.54). Further analyses showed that the reduction in the risk of myocardial infarction was apparent only among those who were 50 years of age and older."
Patrono C, et al.: Low-Dose Aspirin for the Prevention of Atherothrombosis. N Engl J Med 2005;353:2373-83.
Aspirin acts by inhibiting the action of cyclooxygenases, key enzymes in the conversion of the fatty acid arachidonic acid into prostaglandins. The prostaglandins are important signaling molecules that can be produced by almost all tissues in the body. They are important regulators of physiologic function and key mediators of the inflammatory response. Arachidonic acid is a 20-carbon fatty acid with four double bonds; that is present in the phospholipids in the cell's plasma membrane. The cyclooxygenases exist in two forms, cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2). Low-dose aspirin selectively inhibits COX-1, whereas high-dose aspirin inhibits both COX-1 and COX-2. These act on arachidonic acid to create prostaglandin H2, an intermediate compound that is then converted into any one of several prostaglandins (thromboxane, prostaglandin E2, prostaglandin F2a, and prostacyclin). Thromboxane promotes platelet aggregation and clotting, while prostacyclin, produced primarily by endothelium, promotes vascular relaxation and inhibits platelet aggregation.
The effect of aspirin on prostaglandin synthesis is differential. Mature platelets express only COX-1, but vascular endothelial cells express both COX-1 and COX-2. Thromboxane derived mainly from COX-1 in platelets, and its synthesis is highly sensitive to inhibition by aspirin. In contrast, vascular PGI2 is derived predominantly from COX-2 and is less susceptible to inhibition by low doses of aspirin. As a result, aspirin induces a long-lasting inhibition of thromboxane synthesis and a prolongation of bleeding time. In contrast, low-dose aspirin little effect on prostacyclin (PGI2) production. In individuals with atherosclerotic vascular disease, low dose aspirin has been shown by many studies to reduce the risk of myocardial infarction by about 34%, and it reduces the risk of occlusive stroke by about 25%. However, long-term therapy with low-dose aspirin increases the risk of bleeding (mostly from the gastrointestinal tract) in middle-aged patients. There also appears to be a slight increase in the risk of hemorrhagic stroke. Despite the potential increased risk of bleeding which long term therapy, there is good evidence that low dose aspirin is of benefit to individuals with high risk of cardiovascular disease. On the other hand, the benefit in people with low risk is not clear.
One of the questions that arose after the results of the Physicians' Health Study were reported was whether the results could be generalized to women. This question was finally addressed by a subsequent randomized trial conducted in women and reported by Ridker et al. in 2005.
Ridker RM, et al.: A Randomized Trial of Low-Dose Aspirin in the Primary Prevention of Cardiovascular Disease in Women. N Engl J Med 2005;352:1293-304.
These investigators conducted a clinical trial among 39,876 initially healthy women 45 years of age or older who were randomly assigned to receive 100 mg of aspirin on alternate days or placebo. During roughly ten years of follow-up, there was a 17% reduction in the risk of stroke in the aspirin group (rate ratio = 0.83; 95% confidence interval, 0.69 - 0.99; P=0.04), primarily due to a 24% reduction in ischemic (occlusive) strokes and a non-significant increase in the risk of hemorrhagic stroke (rate ratio =1.24; 95% confidence interval, 0.82 - 1.87; P=0.31). However, aspirin had no significant effect on the risk of fatal or nonfatal myocardial infarction (rate ratio = 1.02; 95% confidence interval, 0.84 - 1.25; P=0.83) or death from cardiovascular causes (rate ratio = 0.95; 95% confidence interval, 0.74 - 1.22; P=0.68). Gastrointestinal bleeding requiring transfusion was more frequent in the aspirin group (rate ratio = 1.40; 95% confidence interval, 1.07 - 1.83; P=0.02). Subgroup analyses showed that aspirin significantly reduced the risk of major cardiovascular events, ischemic stroke, and myocardial infarction among women 65 years of age or older.
A follow-up letter to the editor pointed out that the majority of patients in this study (84.5 percent) had a 10-year risk of less than 5% for an incident myocardial infarction and therefore would not have received aspirin as primary prophylaxis, according to the American Heart Association guidelines. The American Heart Association recommendations indicate that aspirin should be used as primary prevention for coronary events in persons with a 10-year risk of myocardial infarction that is greater than 10%.
In a 2009 statement, the U.S. Preventive Services Task Force issued a recommendation for aspirin therapy based on analysis of evidence from literature since 2002. They recommend aspirin therapy for:
Oxidation of LDL contributes to the development of atherosclerosis. Oxidized LDL is found in atherosclerotic plaques, and oxidation of LDL appears to enhance its uptake by macrophages. This posed the question of whether treatment with antioxidants might retard the development of atherosclerosis. This hypothesis became more compelling when treatment antioxidants was shown to inhibit atherosclerosis in animal models. Epidemiologic studies initially suggested that vitamin E (but not vitamin C) was beneficial in reducing the risk of coronary heart disease in humans. The first two articles cited below are large prospective cohort studies - one in men and the other in women.
Rimm EB, et al.: Vitamin E Consumption and the Risk of Coronary Heart Disease in Men. N Engl J Med 1993; 328:1450-1456
From the abstract:
"In 1986, 39,910 U.S. male health professionals 40 to 75 years of age who were free of diagnosed coronary heart disease, diabetes, and hypercholesterolemia completed detailed dietary questionnaires that assessed their usual intake of vitamin C, carotene, and vitamin E in addition to other nutrients. During four years of follow-up, we documented 667 cases of coronary disease.
After controlling for age and several coronary risk factors, we observed a lower risk of coronary disease among men with higher intakes of vitamin E (P for trend = 0.003). For men consuming more than 60 IU per day of vitamin E, the multivariate relative risk was 0.64 (95 percent confidence interval, 0.49 to 0.83) as compared with those consuming less than 7.5 IU per day. As compared with men who did not take vitamin E supplements, men who took at least 100 IU per day for at least two years had a multivariate relative risk of coronary disease of 0.63 (95 percent confidence interval, 0.47 to 0.84). Carotene intake was not associated with a lower risk of coronary disease among those who had never smoked, but it was inversely associated with the risk among current smokers (relative risk, 0.30; 95 percent confidence interval, 0.11 to 0.82) and former smokers (relative risk, 0.60; 95 percent confidence interval, 0.38 to 0.94). In contrast, a high intake of vitamin C was not associated with a lower risk of coronary disease."
Kushi LH, et al.: Dietary Antioxidant Vitamins and Death from Coronary Heart Disease in Postmenopausal Women. N Engl J Med 1996; 334:1156-1162
From the abstract:
"We studied 34,486 postmenopausal women with no cardiovascular disease who in early 1986 completed a questionnaire that assessed, among other factors, their intake of vitamins A, E, and C from food sources and supplements. During approximately seven years of follow-up (ending December 31, 1992), 242 of the women died of coronary heart disease.
In analyses adjusted for age and dietary energy intake, vitamin E consumption appeared to be inversely associated with the risk of death from coronary heart disease. This association was particularly striking in the subgroup of 21,809 women who did not consume vitamin supplements (relative risks from lowest to highest quintile of vitamin E intake, 1.0, 0.68, 0.71, 0.42, and 0.42; P for trend = 0.008). After adjustment for possible confounding variables, this inverse association remained (relative risks from lowest to highest quintile, 1.0, 0.70, 0.76, 0.32, and 0.38; P for trend = 0.004). There was little evidence that the intake of vitamin E from supplements was associated with a decreased risk of death from coronary heart disease, but the effects of high-dose supplementation and the duration of supplement use could not be definitively addressed. Intake of vitamins A and C did not appear to be associated with the risk of death from coronary heart disease.
These results suggest that in postmenopausal women the intake of vitamin E from food is inversely associated with the risk of death from coronary heart disease and that such women can lower their risk without using vitamin supplements. By contrast, the intake of vitamins A and C was not associated with lower risks of dying from coronary disease."
While these findings suggested a benefit of vitamin E in reducing cardiovascular disease, subsequent randomized clinical trials in men and women failed to show any benefit. See the excerpts from the two randomized clinical trials cited below.
Sesso HD, et al.: Vitamins E and C in the prevention of cardiovascular disease in men: the Physicians' Health Study II randomized controlled trial. JAMA. 2008 Nov 12;300(18):2123-33.
From the abstract:
"The Physicians' Health Study II was a randomized, double-blind, placebo-controlled factorial trial of vitamin E and vitamin C that began in 1997 and continued until its scheduled completion on August 31, 2007. There were 14,641 US male physicians enrolled, who were initially aged 50 years or older, including 754 men (5.1%) with prevalent cardiovascular disease at randomization.
INTERVENTION: Individual supplements of 400 IU of vitamin E every other day and 500 mg of vitamin C daily.
MAIN OUTCOME MEASURES: A composite end point of major cardiovascular events (nonfatal myocardial infarction, nonfatal stroke, and cardiovascular disease death).
RESULTS: During a mean follow-up of 8 years, there were 1245 confirmed major cardiovascular events. Compared with placebo, vitamin E had no effect on the incidence of major cardiovascular events (both active and placebo vitamin E groups, 10.9 events per 1000 person-years; hazard ratio [HR], 1.01 [95% confidence interval {CI}, 0.90-1.13]; P = .86), as well as total myocardial infarction (HR, 0.90 [95% CI, 0.75-1.07]; P = .22), total stroke (HR, 1.07 [95% CI, 0.89-1.29]; P = .45), and cardiovascular mortality (HR, 1.07 [95% CI, 0.90-1.28]; P = .43). There also was no significant effect of vitamin C on major cardiovascular events (active and placebo vitamin E groups, 10.8 and 10.9 events per 1000 person-years, respectively; HR, 0.99 [95% CI, 0.89-1.11]; P = .91), as well as total myocardial infarction (HR, 1.04 [95% CI, 0.87-1.24]; P = .65), total stroke (HR, 0.89 [95% CI, 0.74-1.07]; P = .21), and cardiovascular mortality (HR, 1.02 [95% CI, 0.85-1.21]; P = .86). Neither vitamin E (HR, 1.07 [95% CI, 0.97-1.18]; P = .15) nor vitamin C (HR, 1.07 [95% CI, 0.97-1.18]; P = .16) had a significant effect on total mortality but vitamin E was associated with an increased risk of hemorrhagic stroke (HR, 1.74 [95% CI, 1.04-2.91]; P = .04).
CONCLUSIONS: In this large, long-term trial of male physicians, neither vitamin E nor vitamin C supplementation reduced the risk of major cardiovascular events. These data provide no support for the use of these supplements for the prevention of cardiovascular disease in middle-aged and older men."
Song Y, et al.: Effects of vitamins C and E and beta-carotene on the risk of type 2 diabetes in women at high risk of cardiovascular disease: a randomized controlled trial. Am J Clin Nutr. 2009;90(2):429-37.
From the abstract:
"The purpose of this study was to investigate the long-term effects of supplementation with vitamin C, vitamin E, and beta-carotene for primary prevention of type 2 diabetes.
In the Women's Antioxidant Cardiovascular Study, a randomized trial that occurred between 1995 and 2005, 8171 female health professionals aged > or =40 y with either a history of cardiovascular disease (CVD) or > or =3 CVD risk factors were randomly assigned to receive vitamin C (ascorbic acid, 500 mg every day), vitamin E (RRR-alpha-tocopherol acetate, 600 IU every other day), beta-carotene (50 mg every other day), or their respective placebos.
During a median follow-up of 9.2 y, a total of 895 incident cases occurred among 6574 women who were free of diabetes at baseline. There was a trend toward a modest reduction in diabetes risk in women assigned to receive vitamin C compared with those assigned to receive placebo [relative risk (RR): 0.89; 95% CI: 0.78, 1.02; P = 0.09], whereas a trend for a slight elevation in diabetes risk was observed for vitamin E treatment (RR: 1.13; 95% CI: 0.99, 1.29; P = 0.07). However, neither of these effects reached statistical significance. No significant effect was observed for beta-carotene treatment (RR: 0.97; 95% CI: 0.85, 1.11; P = 0.68).
Our randomized trial data showed no significant overall effects of vitamin C, vitamin E, and beta-carotene on risk of developing type 2 diabetes in women at high risk of CVD."
|
Prospective cohort studies suggested that individuals who ate diets rich in vitamin E had a lower risk of heart disease, but clinical trials demonstrated that supplementation with neither vitamin E nor vitamin C had any effect. Two points might be made:
|
Numerous observational studies have established that elevated blood levels of homocysteine are associated with a graded increase in risk of coronary artery disease, MI, stroke, venous thromboembolism, and peripheral vascular disease. It is believed that the mechanism for this increased risks is related to oxidative stress. Dietary supplementation with folic acid (folate) and vitamin B12 reduces homocysteine levels, but vitamin therapy has generally not been successful in reducing vascular disease outcomes in subjects with mildly elevated homocysteine levels. The first large, randomized trial found that lowering the total homocysteine level with B vitamins failed to prevent recurrent stroke, myocardial infarction, or death in patients who had had a recent stroke
Bønaa KH, et al.: Homocysteine lowering and cardiovascular events after acute myocardial infarction. N Engl J Med 2006;354:1578-88.
These authors conducted a randomized clinical trial with 3749 men and women who had had an acute myocardial infarction within seven days before randomization.
From the abstract:
"Patients were randomly assigned, in a two-by-two factorial design, to receive one of the following four daily treatments: 0.8 mg of folic acid, 0.4 mg of vitamin B12, and 40 mg of vitamin B6; 0.8 mg of folic acid and 0.4 mg of vitamin B12; 40 mg of vitamin B6; or placebo. The primary end point during a median follow-up of 40 months was a composite of recurrent myocardial infarction, stroke, and sudden death attributed to coronary artery disease.
RESULTS
The mean total homocysteine level was lowered by 27 percent among patients given folic acid plus vitamin B12, but such treatment had no significant effect on the primary end point (risk ratio, 1.08; 95 percent confidence interval, 0.93 to 1.25; P = 0.31). Also, treatment with vitamin B6 was not associated with any significant benefit with regard to the primary end point (relative risk of the primary end point, 1.14; 95 percent confidence interval, 0.98 to 1.32; P = 0.09). In the group given folic acid, vitamin B12, and vitamin B6, there was a trend toward an increased risk (relative risk, 1.22; 95 percent confidence interval, 1.00 to 1.50; P = 0.05).
CONCLUSIONS
Treatment with B vitamins did not lower the risk of recurrent cardiovascular disease after acute myocardial infarction. A harmful effect from combined B vitamin treatment was suggested. Such treatment should therefore not be recommended."
A number of pieces of evidence suggest a link between chronic infection and risk of atherosclerotic cardiovascular disease. Herpesviruses promote atherosclerosis in experimental animals, and they have been found in atherosclerotic plaques in humans. Chlamydia pneumoniae have been found in atheromatous plaques, and increased antibodies to these agents are associated with increased risk of new infarction in patients who have had myocardial infarction. Periodontal disease is also associated with an increased risk of coronary artery disease and peripheral vascular disease, even after adjusting for known confounding factors. Mouth organisms, such as Porphyromonas gingivalis and Streptococcus sanguis have been found in plaques. Injection of Cytomegalovirus, Chlamydia, or P. gingivalis into animal models does not cause atherosclerosis, but it does accelerate its progression. It is also noteworthy that C-reactive protein, which is produced by the liver in response to inflammation, is a non-specific marker of chronic inflammation, and it is considered to be an independent risk factor for atherosclerotic disease.
For an excellent review see Mattila KJ, et al.: Role of Infection as a Risk Factor for Atherosclerosis, Myocardial Infarction, and Stroke. Clin. Infect. Dis. 1998;26(3):719-734.
These observations led to a number of clinical trials that tested the possibility of treating high risk patients with antibiotics. Nevertheless, the results to date have been almost universally negative. (See editorial by Jeffrey L Anderson in N. Engl. J. Med.) Given the lack of effect of antibiotics, some believe that it may be the total "pathogen burden," i.e., the cumulative exposure to multiple atherogenic infectious agents that might enhance risk over a long period of time. While the role of infection remains to be established, the report below by Tonetti et al. suggests that chronic infection may predispose to atherogenesis by causing endothelial dysfunction.
Tonetti MS, et al.: Periodontal Disease Treatment of Periodontitis and Endothelial Function. N Engl J Med 2007;356:911-20.
From the abstract:
"We randomly assigned 120 patients with severe periodontitis to community-based periodontal care (59 patients) or intensive periodontal treatment (61). Endothelial function, as assessed by measurement of the diameter of the brachial artery during flow (flow-mediated dilatation), and inflammatory biomarkers and markers of coagulation and endothelial activation were evaluated before treatment and 1, 7, 30, 60, and 180 days after treatment.
Results
Twenty-four hours after treatment, flow-mediated dilatation was significantly lower in the intensive-treatment group than in the control-treatment group (absolute difference, 1.4%; 95% confidence interval [CI], 0.5 to 2.3; P = 0.002), and levels of C-reactive protein, interleukin-6, and the endothelial-activation markers soluble E-selectin and von Willebrand factor were significantly higher (P<0.05 for all comparisons). However, flow-mediated dilatation was greater and the plasma levels of soluble E-selectin were lower in the intensive-treatment group than in the control treatment group 60 days after therapy (absolute difference in flow-mediated dilatation, 0.9%; 95% CI, 0.1 to 1.7; P = 0.02) and 180 days after therapy (difference, 2.0%; 95% CI, 1.2 to 2.8; P<0.001). The degree of improvement was associated with improvement in measures of periodontal disease (r = 0.29 by Spearman rank correlation, P = 0.003). There were no serious adverse effects in either of the two groups, and no cardiovascular events occurred.
Conclusions
Intensive periodontal treatment resulted in acute, short-term systemic inflammation and endothelial dysfunction. However, 6 months after therapy, the benefits in oral health were associated with improvement in endothelial function."
Cardiovascular disease already exact a devastating toll in non-Western countries, and mortality and morbidity from cardiovascular disease are increasing at an alarming rate. The excerpts below are from a Perspectives article in New England Journal of Medicine in which K. Srinath Reddy portrays this epidemic as a complex challenge and an opportunity to forestall the epidemic by creatively and thoughtfully applying the lessons we have learned about public health interventions. He says, "A concerted public health response must integrate population-based prevention strategies and cost-effective clinical care, since the health systems of developing countries can ill afford the demands of technology-intensive treatments."
|
K. Srinath Reddy: Cardiovascular Disease in Non-Western Countries. Perspective article in: N. Engl. J. Med. 2004; 350;24. "These epidemics [of cardiovascular disease] are driven by social and economic changes that have profound effects on living habits. Although sharp shifts in demographic patterns and lifestyle have resulted from urbanization and industrialization, the globalization that constituted the tailwind of the 20th century propelled developing countries into the worldwide epidemic of cardiovascular disease. The change reflects both a demographic shift toward increasing life expectancy and a shift in nutrition: people who live longer have greater exposure to cardiovascular risk factors, and Westernized diets and patterns of physical inactivity result in elevations in blood pressure, body weight, blood sugar levels, and lipid concentrations. A huge increase in the prevalence of diabetes will further increase the burden of cardiovascular disease; India, where nearly 20 million people had diabetes in 1995, will see at least a tripling of that number by 2025. Moreover, the global expansion of the tobacco trade has led to large increases in the rate of smoking. The levels of these risk factors have increased steeply in most non-Western countries over the past two decades. Although there are some differences among ethnic groups in the interactions between genes and the environment, the available evidence indicates that the main risk factors for cardiovascular disease are relevant to all populations and that most of the risk is environmentally determined. Thus, these trends portend an explosion of atherothrombotic cardiovascular diseases in developing countries. Given the rate at which the distributions of body-mass index and blood cholesterol levels have changed in the Chinese population, possibly in association with a sharp increase in fat consumption, it is clear that countries like China will see a rapid escalation of the rate of coronary heart disease. The epidemics of cardiovascular disease struck the more affluent sections of developing countries first, but as the epidemics mature, the social gradient is reversing, with socioeconomically disadvantaged groups becoming increasingly vulnerable. The poor and the less educated everywhere now use tobacco with greater frequency than the rich and the better educated do. In Brazil, women in lower-income groups have had increasing rates of overweight and obesity since 1989, in contrast to the significant decrease observed in high-income groups. Studies conducted in Indian cities in the past decade have shown that the poor have a higher risk of heart attack than the rich. The poor also have less access to health care; their risk factors are not recognized in a timely fashion; and they often do not receive effective treatment, since public health care is generally restricted to the treatment of infectious diseases. Neglect of the epidemics of cardiovascular disease will heap greater injustice on the poorest of countries and the poorest of people. Although these developments mirror in many ways the path of the epidemics of cardiovascular disease in Western countries, there are important differences. Whereas the epidemics in the West flowed and ebbed over the course of a century, the health transition in developing countries has been compressed into a few decades. Urbanization is occurring in places with uncorrected poverty and increasing disparities in income, causing the poor to be especially vulnerable, while resource-constrained national health systems are ill equipped to cope with the double burden of infectious and chronic diseases. Globalization accelerates the change, as Western products and models of behavior are increasingly exported to non-Western countries. However, globalization also offers opportunities to facilitate the prevention of cardiovascular disease, through the application of knowledge generated in Western countries: the understanding of risk factors, evidence regarding effective interventions, tools and technology for reducing risk, new models of healthy behavior that can be promoted through the mass media. Thus, there is an opportunity to alter the pattern of health transition in developing countries by implementing effective measures for prevention and control before the epidemics peak — ideally, permitting a rapid shift to a state in which cardiovascular events occur only or primarily after 70 years of age. A concerted public health response must integrate population-based prevention strategies and cost-effective clinical care, since the health systems of developing countries can ill afford the demands of technology-intensive treatments. The population approach is more rewarding and sustainable in the medium and long term, since even small reductions in each risk factor can add up to huge reductions in the rate of cardiovascular events. And if healthy behavior is established as a desirable norm in a society, it can have a multigenerational effect. There are differences of opinion, however, regarding whether population-level interventions should rely principally on behavioral change governed by the personal choices of well-informed people or should operate through policy interventions that modify behavior through social and economic determinants. Western countries generally favor the personal-choice approach, but this approach assumes that healthy choices are widely available and affordable and that it is easy to educate consumers about the merits and demerits of each option. The North Karelia project in Finland provides a successful model of behavioral change through community health education combined with industry-level interventions for providing healthful food choices. Such programs, however, may be less effective in non-Western societies, where personal choice is limited by lack of awareness and highly restricted options. Policy-level interventions have proved effective in bringing about population-wide behavioral change and risk reduction even in the short term. In Mauritius, governmental action to substitute soybean oil for palm oil as the subsidized, rationed oil resulted in a remarkable reduction in cholesterol levels. Changes in economic policy that increased the availability of fresh fruits and vegetables and helped to substitute vegetable fats for animal fats led to a sharp decline in mortality from cardiovascular causes in Poland. Non-Western countries must implement policies that will help to reduce the consumption of tobacco, salt, and unhealthful fats and increase the consumption of fruits and vegetables, through production and pricing mechanisms that increase options and influence consumer choice. But policy interventions will have limited success if the community is unwilling to accept them. Hence, the top-down approach of enabling legislation and regulation must be complemented by a bottom-up approach of community mobilization through health education. Measures taken in Western countries to protect nonsmokers from exposure to environmental tobacco smoke illustrate such a combined approach. At the same time, people with a high risk of cardiovascular disease or clinical manifestations of disease need protection from premature death and prolonged disability. Evidence-based, context-specific, and resource-sensitive interventions must be cost-effectively integrated into all levels of health care, to strengthen both primary and secondary prevention of cardiovascular disease. The extensive use of aspirin in primary care settings for the treatment of suspected myocardial infarction can save millions of lives at low cost (about $3 per life saved, in India). Blood-pressure–lowering therapies reduce overall cardiovascular risk and have a substantial effect on mortality from coronary heart disease and stroke, and smoking cessation effectively reduces cardiovascular risk. Operational research is required to ensure the effective integration of such therapies and community-based preventive strategies into the health care systems of non-Western countries. The Initiative for Cardiovascular Health Research in the Developing Countries is a multi-institutional, international program that works to stimulate, support, and strengthen such research. Epidemics of cardiovascular disease in non-Western countries present complex challenges but also great opportunities. Seldom in the history of human health have we been endowed with such foresight about our destiny and forearmed with such power to change it. It is a challenge to human intellect and enterprise to apply our knowledge creatively and cost-effectively to minimize the burden of cardiovascular disease throughout the world." |