Behavioral Change Models
Introduction
Public health is a multi-disciplinary field that aims to 1) prevent disease and death, 2) promote a better quality of life, and 3) create environmental conditions in which people can be healthy by intervening at the institutional, community, and societal level.
Whether public health practitioners can achieve this mission depends upon their ability to accurately identify and define public health problems, assess the fundamental causes of these problems, determine populations most at-risk, develop and implement theory- and evidence-based interventions, and evaluate and refine those interventions to ensure that they are achieving their desired outcomes without unwanted negative consequences.
To be effective in these endeavors, public health practitioners must know how to apply the basic principles, theories, research findings, and methods of the social and behavioral sciences to inform their efforts. A thorough understanding of theories used in public health, which are mainly derived from the social and behavioral sciences, allow practitioners to:
- Assess the fundamental causes of a public health problem, and
- Develop interventions to address those problems.
Note: This module has been translated into Estonian by Marie Stefanova. The translation can be accessed at
https://www.bildeleekspert.dk/blog/2018/08/06/sotsiaalsete-normide-teooria/
Learning Objectives
After successfully reviewing these modules, students will be able to:
- List and describe the key constructs of the Health Belief Model and the theory of planned behavior and explain how they might be applied to develop effective public health interventions
- List and describe the elements of "perceived behavioral control"
- Describe the underlying theory and basic elements of Social Norms Theory and marketing campaigns
- List and describe the key constructs of Social Cognitive Theory and explain how they might be applied to develop effective public health interventions
- Summarize the criticisms that have been made regarding the major traditional models of health behavior change and why these models do not seem adequate to account for observed health behaviors
- Outline the major steps in the Transtheoretical Model
- List the characteristics of each step of the Transtheoretical Model
- Describe Diffusion of Innovation Theory and how it can be applied in health promotion
- Outline the basic structures of the Theory of Gender and Power and its application to Public Health
- Explain the constructs of the Sexual Health Model and its application to public health
The Health Belief Model
The Health Belief Model (HBM) was developed in the early 1950s by social scientists at the U.S. Public Health Service in order to understand the failure of people to adopt disease prevention strategies or screening tests for the early detection of disease. Later uses of HBM were for patients' responses to symptoms and compliance with medical treatments. The HBM suggests that a person's belief in a personal threat of an illness or disease together with a person's belief in the effectiveness of the recommended health behavior or action will predict the likelihood the person will adopt the behavior.
The HBM derives from psychological and behavioral theory with the foundation that the two components of health-related behavior are 1) the desire to avoid illness, or conversely get well if already ill; and, 2) the belief that a specific health action will prevent, or cure, illness. Ultimately, an individual's course of action often depends on the person's perceptions of the benefits and barriers related to health behavior. There are six constructs of the HBM. The first four constructs were developed as the original tenets of the HBM. The last two were added as research about the HBM evolved.
- Perceived susceptibility - This refers to a person's subjective perception of the risk of acquiring an illness or disease. There is wide variation in a person's feelings of personal vulnerability to an illness or disease.
- Perceived severity - This refers to a person's feelings on the seriousness of contracting an illness or disease (or leaving the illness or disease untreated). There is wide variation in a person's feelings of severity, and often a person considers the medical consequences (e.g., death, disability) and social consequences (e.g., family life, social relationships) when evaluating the severity.
- Perceived benefits - This refers to a person's perception of the effectiveness of various actions available to reduce the threat of illness or disease (or to cure illness or disease). The course of action a person takes in preventing (or curing) illness or disease relies on consideration and evaluation of both perceived susceptibility and perceived benefit, such that the person would accept the recommended health action if it was perceived as beneficial.
- Perceived barriers - This refers to a person's feelings on the obstacles to performing a recommended health action. There is wide variation in a person's feelings of barriers, or impediments, which lead to a cost/benefit analysis. The person weighs the effectiveness of the actions against the perceptions that it may be expensive, dangerous (e.g., side effects), unpleasant (e.g., painful), time-consuming, or inconvenient.
- Cue to action - This is the stimulus needed to trigger the decision-making process to accept a recommended health action. These cues can be internal (e.g., chest pains, wheezing, etc.) or external (e.g., advice from others, illness of family member, newspaper article, etc.).
- Self-efficacy - This refers to the level of a person's confidence in his or her ability to successfully perform a behavior. This construct was added to the model most recently in mid-1980. Self-efficacy is a construct in many behavioral theories as it directly relates to whether a person performs the desired behavior.
Limitations of Health Belief Model
There are several limitations of the HBM which limit its utility in public health. Limitations of the model include the following:
- It does not account for a person's attitudes, beliefs, or other individual determinants that dictate a person's acceptance of a health behavior.
- It does not take into account behaviors that are habitual and thus may inform the decision-making process to accept a recommended action (e.g., smoking).
- It does not take into account behaviors that are performed for non-health related reasons such as social acceptability.
- It does not account for environmental or economic factors that may prohibit or promote the recommended action.
- It assumes that everyone has access to equal amounts of information on the illness or disease.
- It assumes that cues to action are widely prevalent in encouraging people to act and that "health" actions are the main goal in the decision-making process.
The HBM is more descriptive than explanatory, and does not suggest a strategy for changing health-related actions. In preventive health behaviors, early studies showed that perceived susceptibility, benefits, and barriers were consistently associated with the desired health behavior; perceived severity was less often associated with the desired health behavior. The individual constructs are useful, depending on the health outcome of interest, but for the most effective use of the model it should be integrated with other models that account for the environmental context and suggest strategies for change.
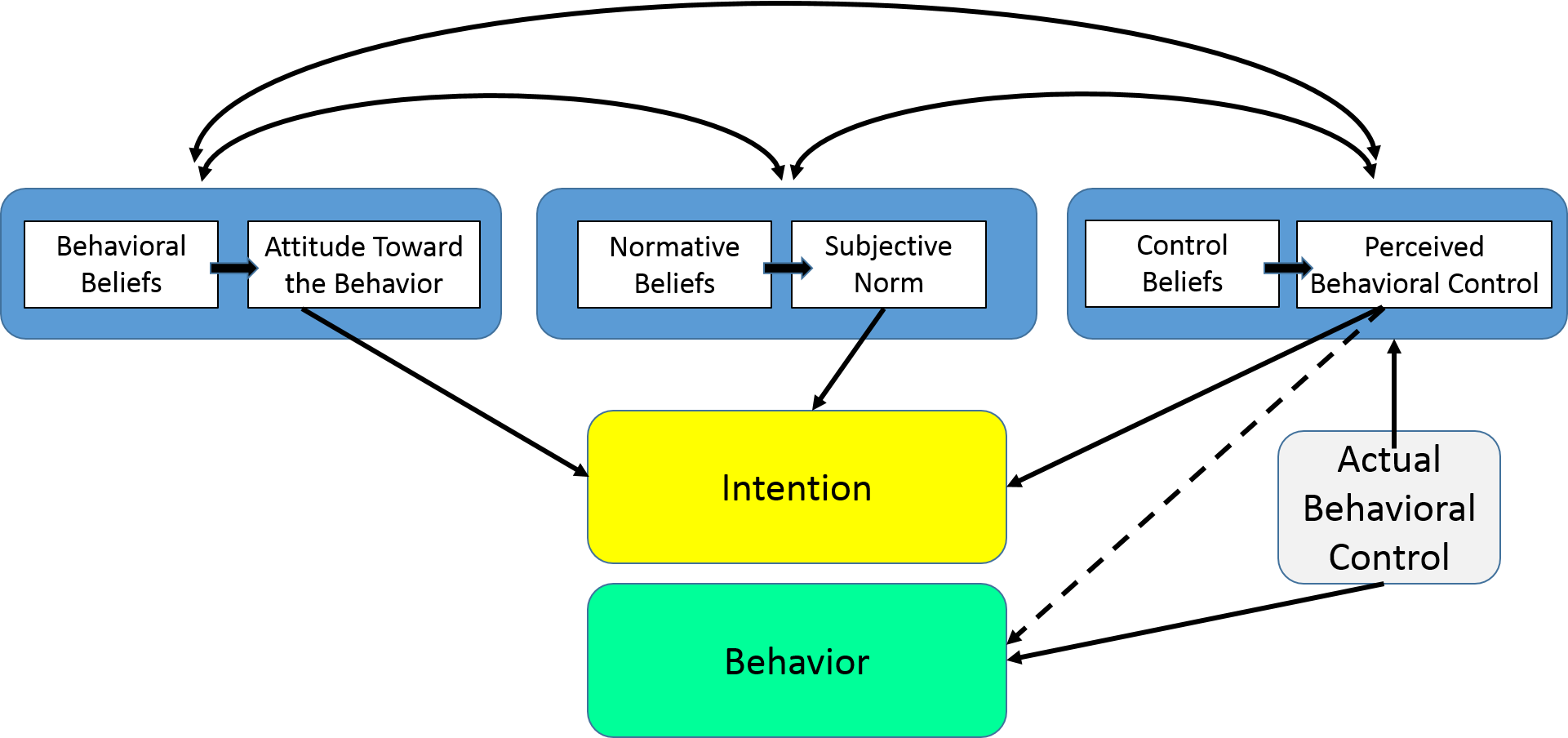
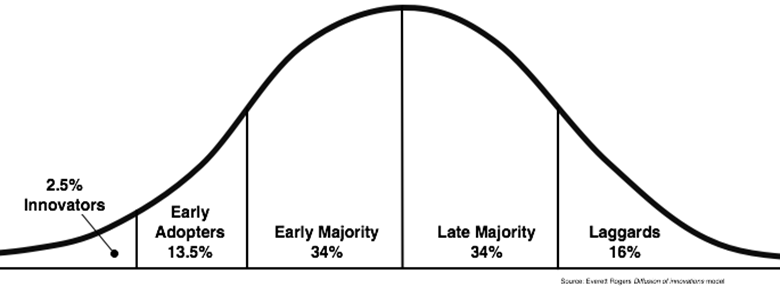
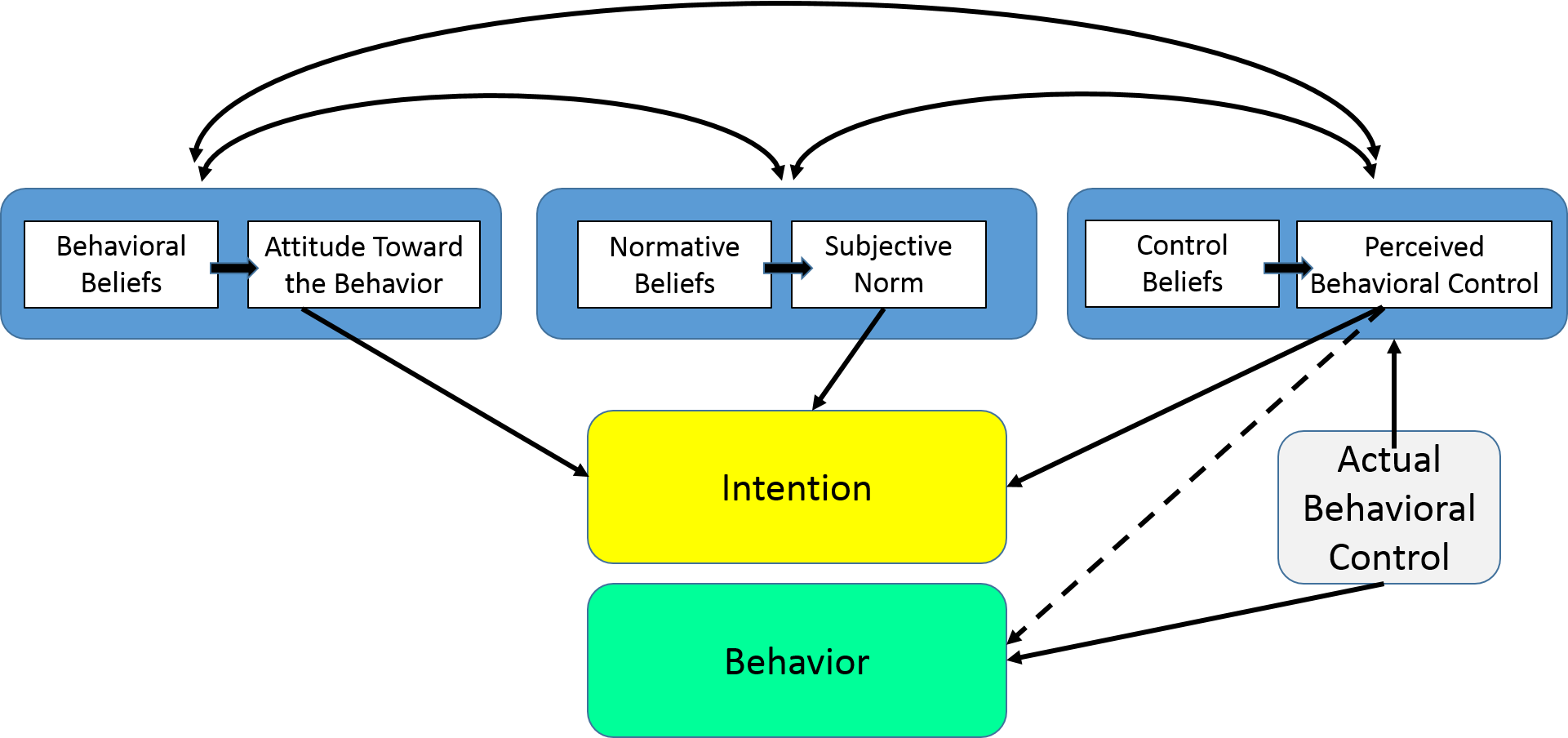
The Theory of Planned Behavior
The Theory of Planned Behavior (TPB) started as the Theory of Reasoned Action in 1980 to predict an individual's intention to engage in a behavior at a specific time and place. The theory was intended to explain all behaviors over which people have the ability to exert self-control. The key component to this model is behavioral intent; behavioral intentions are influenced by the attitude about the likelihood that the behavior will have the expected outcome and the subjective evaluation of the risks and benefits of that outcome.
The TPB has been used successfully to predict and explain a wide range of health behaviors and intentions including smoking, drinking, health services utilization, breastfeeding, and substance use, among others. The TPB states that behavioral achievement depends on both motivation (intention) and ability (behavioral control). It distinguishes between three types of beliefs - behavioral, normative, and control. The TPB is comprised of six constructs that collectively represent a person's actual control over the behavior.
- Attitudes - This refers to the degree to which a person has a favorable or unfavorable evaluation of the behavior of interest. It entails a consideration of the outcomes of performing the behavior.
- Behavioral intention - This refers to the motivational factors that influence a given behavior where the stronger the intention to perform the behavior, the more likely the behavior will be performed.
- Subjective norms - This refers to the belief about whether most people approve or disapprove of the behavior. It relates to a person's beliefs about whether peers and people of importance to the person think he or she should engage in the behavior.
- Social norms - This refers to the customary codes of behavior in a group or people or larger cultural context. Social norms are considered normative, or standard, in a group of people.
- Perceived power - This refers to the perceived presence of factors that may facilitate or impede performance of a behavior. Perceived power contributes to a person's perceived behavioral control over each of those factors.
- Perceived behavioral control - This refers to a person's perception of the ease or difficulty of performing the behavior of interest. Perceived behavioral control varies across situations and actions, which results in a person having varying perceptions of behavioral control depending on the situation. This construct of the theory was added later, and created the shift from the Theory of Reasoned Action to the Theory of Planned Behavior.
Limitations of the Theory of Planned Behavior
There are several limitations of the TPB, which include the following:
- It assumes the person has acquired the opportunities and resources to be successful in performing the desired behavior, regardless of the intention.
- It does not account for other variables that factor into behavioral intention and motivation, such as fear, threat, mood, or past experience.
- While it does consider normative influences, it still does not take into account environmental or economic factors that may influence a person's intention to perform a behavior.
- It assumes that behavior is the result of a linear decision-making process, and does not consider that it can change over time.
- While the added construct of perceived behavioral control was an important addition to the theory, it doesn't say anything about actual control over behavior.
- The time frame between "intent" and "behavioral action" is not addressed by the theory.
The TPB has shown more utility in public health than the Health Belief Model, but it is still limiting in its inability to consider environmental and economic influences. Over the past several years, researchers have used some constructs of the TPB and added other components from behavioral theory to make it a more integrated model. This has been in response to some of the limitations of the TPB in addressing public health problems.
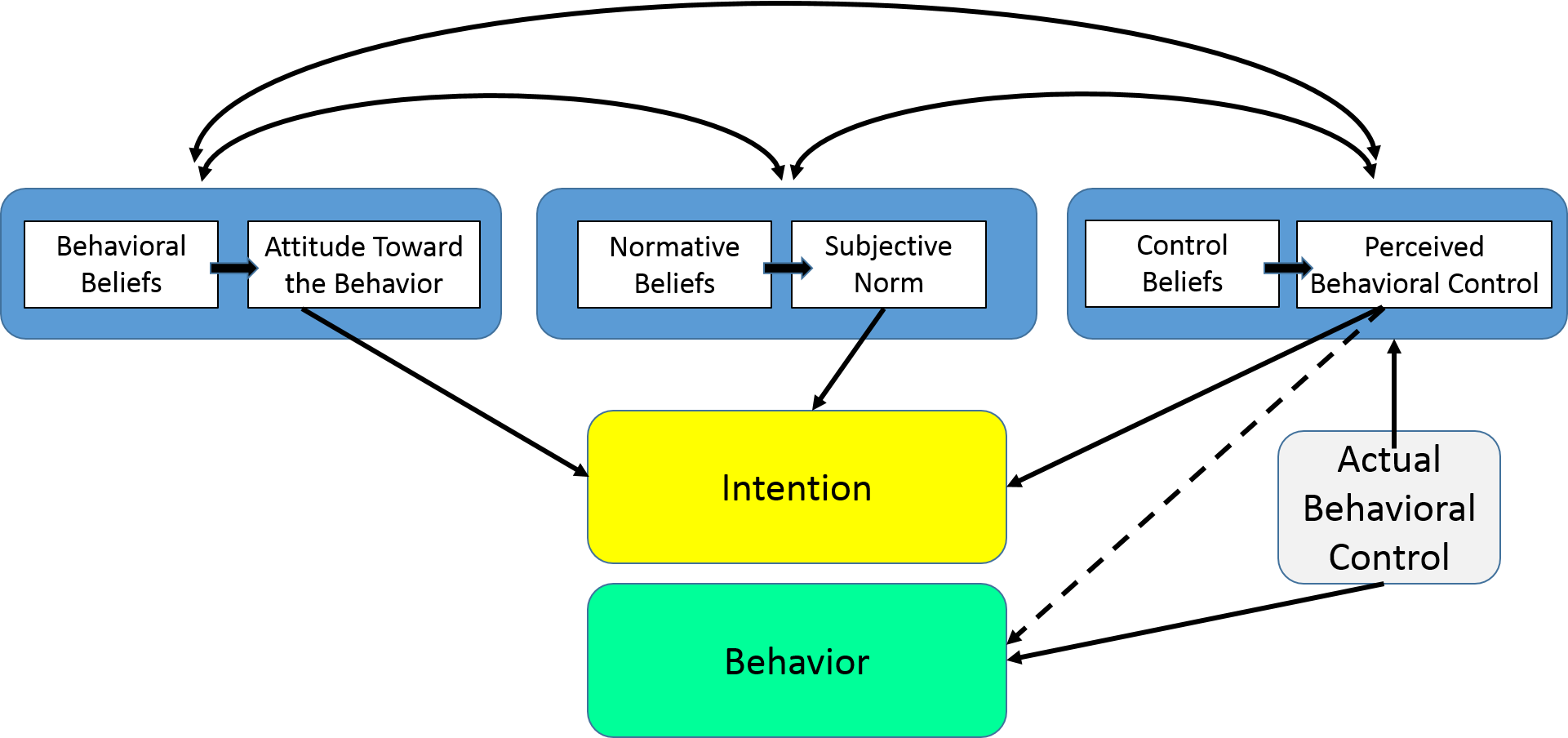
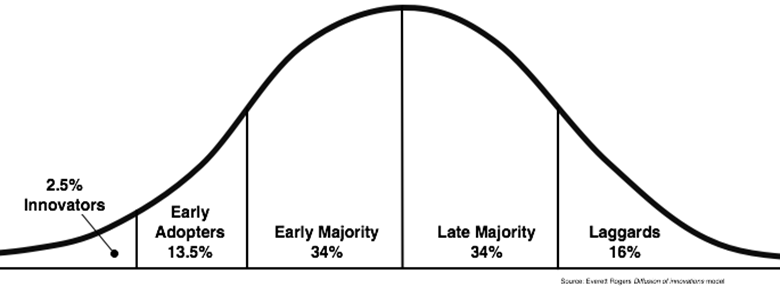
Diffusion of Innovation Theory
Diffusion of Innovation (DOI) Theory, developed by E.M. Rogers in 1962, is one of the oldest social science theories. It originated in communication to explain how, over time, an idea or product gains momentum and diffuses (or spreads) through a specific population or social system. The end result of this diffusion is that people, as part of a social system, adopt a new idea, behavior, or product. Adoption means that a person does something differently than what they had previously (i.e., purchase or use a new product, acquire and perform a new behavior, etc.). The key to adoption is that the person must perceive the idea, behavior, or product as new or innovative. It is through this that diffusion is possible.
Adoption of a new idea, behavior, or product (i.e., "innovation") does not happen simultaneously in a social system; rather it is a process whereby some people are more apt to adopt the innovation than others. Researchers have found that people who adopt an innovation early have different characteristics than people who adopt an innovation later. When promoting an innovation to a target population, it is important to understand the characteristics of the target population that will help or hinder adoption of the innovation. There are five established adopter categories, and while the majority of the general population tends to fall in the middle categories, it is still necessary to understand the characteristics of the target population. When promoting an innovation, there are different strategies used to appeal to the different adopter categories.
- Innovators - These are people who want to be the first to try the innovation. They are venturesome and interested in new ideas. These people are very willing to take risks, and are often the first to develop new ideas. Very little, if anything, needs to be done to appeal to this population.
- Early Adopters - These are people who represent opinion leaders. They enjoy leadership roles, and embrace change opportunities. They are already aware of the need to change and so are very comfortable adopting new ideas. Strategies to appeal to this population include how-to manuals and information sheets on implementation. They do not need information to convince them to change.
- Early Majority - These people are rarely leaders, but they do adopt new ideas before the average person. That said, they typically need to see evidence that the innovation works before they are willing to adopt it. Strategies to appeal to this population include success stories and evidence of the innovation's effectiveness.
- Late Majority - These people are skeptical of change, and will only adopt an innovation after it has been tried by the majority. Strategies to appeal to this population include information on how many other people have tried the innovation and have adopted it successfully.
- Laggards - These people are bound by tradition and very conservative. They are very skeptical of change and are the hardest group to bring on board. Strategies to appeal to this population include statistics, fear appeals, and pressure from people in the other adopter groups.
Source: http://blog.leanmonitor.com/early-adopters-allies-launching-product/
The stages by which a person adopts an innovation, and whereby diffusion is accomplished, include awareness of the need for an innovation, decision to adopt (or reject) the innovation, initial use of the innovation to test it, and continued use of the innovation. There are five main factors that influence adoption of an innovation, and each of these factors is at play to a different extent in the five adopter categories.
- Relative Advantage - The degree to which an innovation is seen as better than the idea, program, or product it replaces.
- Compatibility - How consistent the innovation is with the values, experiences, and needs of the potential adopters.
- Complexity - How difficult the innovation is to understand and/or use.
- Triability - The extent to which the innovation can be tested or experimented with before a commitment to adopt is made.
- Observability - The extent to which the innovation provides tangible results.
Limitations of Diffusion of Innovation Theory
There are several limitations of Diffusion of Innovation Theory, which include the following:
- Much of the evidence for this theory, including the adopter categories, did not originate in public health and it was not developed to explicitly apply to adoption of new behaviors or health innovations.
- It does not foster a participatory approach to adoption of a public health program.
- It works better with adoption of behaviors rather than cessation or prevention of behaviors.
- It doesn't take into account an individual's resources or social support to adopt the new behavior (or innovation).
This theory has been used successfully in many fields including communication, agriculture, public health, criminal justice, social work, and marketing. In public health, Diffusion of Innovation Theory is used to accelerate the adoption of important public health programs that typically aim to change the behavior of a social system. For example, an intervention to address a public health problem is developed, and the intervention is promoted to people in a social system with the goal of adoption (based on Diffusion of Innovation Theory). The most successful adoption of a public health program results from understanding the target population and the factors influencing their rate of adoption.
For more on diffusion of innovation theory see "On the Diffusion of Innovations: How New Ideas Spread" by Leif Singer.
The Social Cognitive Theory
Social Cognitive Theory (SCT) started as the Social Learning Theory (SLT) in the 1960s by Albert Bandura. It developed into the SCT in 1986 and posits that learning occurs in a social context with a dynamic and reciprocal interaction of the person, environment, and behavior. The unique feature of SCT is the emphasis on social influence and its emphasis on external and internal social reinforcement. SCT considers the unique way in which individuals acquire and maintain behavior, while also considering the social environment in which individuals perform the behavior. The theory takes into account a person's past experiences, which factor into whether behavioral action will occur. These past experiences influences reinforcements, expectations, and expectancies, all of which shape whether a person will engage in a specific behavior and the reasons why a person engages in that behavior.
Many theories of behavior used in health promotion do not consider maintenance of behavior, but rather focus on initiating behavior. This is unfortunate as maintenance of behavior, and not just initiation of behavior, is the true goal in public health. The goal of SCT is to explain how people regulate their behavior through control and reinforcement to achieve goal-directed behavior that can be maintained over time. The first five constructs were developed as part of the SLT; the construct of self-efficacy was added when the theory evolved into SCT.
- Reciprocal Determinism - This is the central concept of SCT. This refers to the dynamic and reciprocal interaction of person (individual with a set of learned experiences), environment (external social context), and behavior (responses to stimuli to achieve goals).
- Behavioral Capability - This refers to a person's actual ability to perform a behavior through essential knowledge and skills. In order to successfully perform a behavior, a person must know what to do and how to do it. People learn from the consequences of their behavior, which also affects the environment in which they live.
- Observational Learning - This asserts that people can witness and observe a behavior conducted by others, and then reproduce those actions. This is often exhibited through "modeling" of behaviors. If individuals see successful demonstration of a behavior, they can also complete the behavior successfully.
- Reinforcements - This refers to the internal or external responses to a person's behavior that affect the likelihood of continuing or discontinuing the behavior. Reinforcements can be self-initiated or in the environment, and reinforcements can be positive or negative. This is the construct of SCT that most closely ties to the reciprocal relationship between behavior and environment.
- Expectations - This refers to the anticipated consequences of a person's behavior. Outcome expectations can be health-related or not health-related. People anticipate the consequences of their actions before engaging in the behavior, and these anticipated consequences can influence successful completion of the behavior. Expectations derive largely from previous experience. While expectancies also derive from previous experience, expectancies focus on the value that is placed on the outcome and are subjective to the individual.
- Self-efficacy - This refers to the level of a person's confidence in his or her ability to successfully perform a behavior. Self-efficacy is unique to SCT although other theories have added this construct at later dates, such as the Theory of Planned Behavior. Self-efficacy is influenced by a person's specific capabilities and other individual factors, as well as by environmental factors (barriers and facilitators).
Limitation of Social Cognitive Theory
There are several limitations of SCT, which should be considered when using this theory in public health. Limitations of the model include the following:
- The theory assumes that changes in the environment will automatically lead to changes in the person, when this may not always be true.
- The theory is loosely organized, based solely on the dynamic interplay between person, behavior, and environment. It is unclear the extent to which each of these factors into actual behavior and if one is more influential than another.
- The theory heavily focuses on processes of learning and in doing so disregards biological and hormonal predispositions that may influence behaviors, regardless of past experience and expectations.
- The theory does not focus on emotion or motivation, other than through reference to past experience. There is minimal attention on these factors.
- The theory can be broad-reaching, so can be difficult to operationalize in entirety.
Social Cognitive Theory considers many levels of the social ecological model in addressing behavior change of individuals. SCT has been widely used in health promotion given the emphasis on the individual and the environment, the latter of which has become a major point of focus in recent years for health promotion activities. As with other theories, applicability of all the constructs of SCT to one public health problem may be difficult especially in developing focused public health programs.
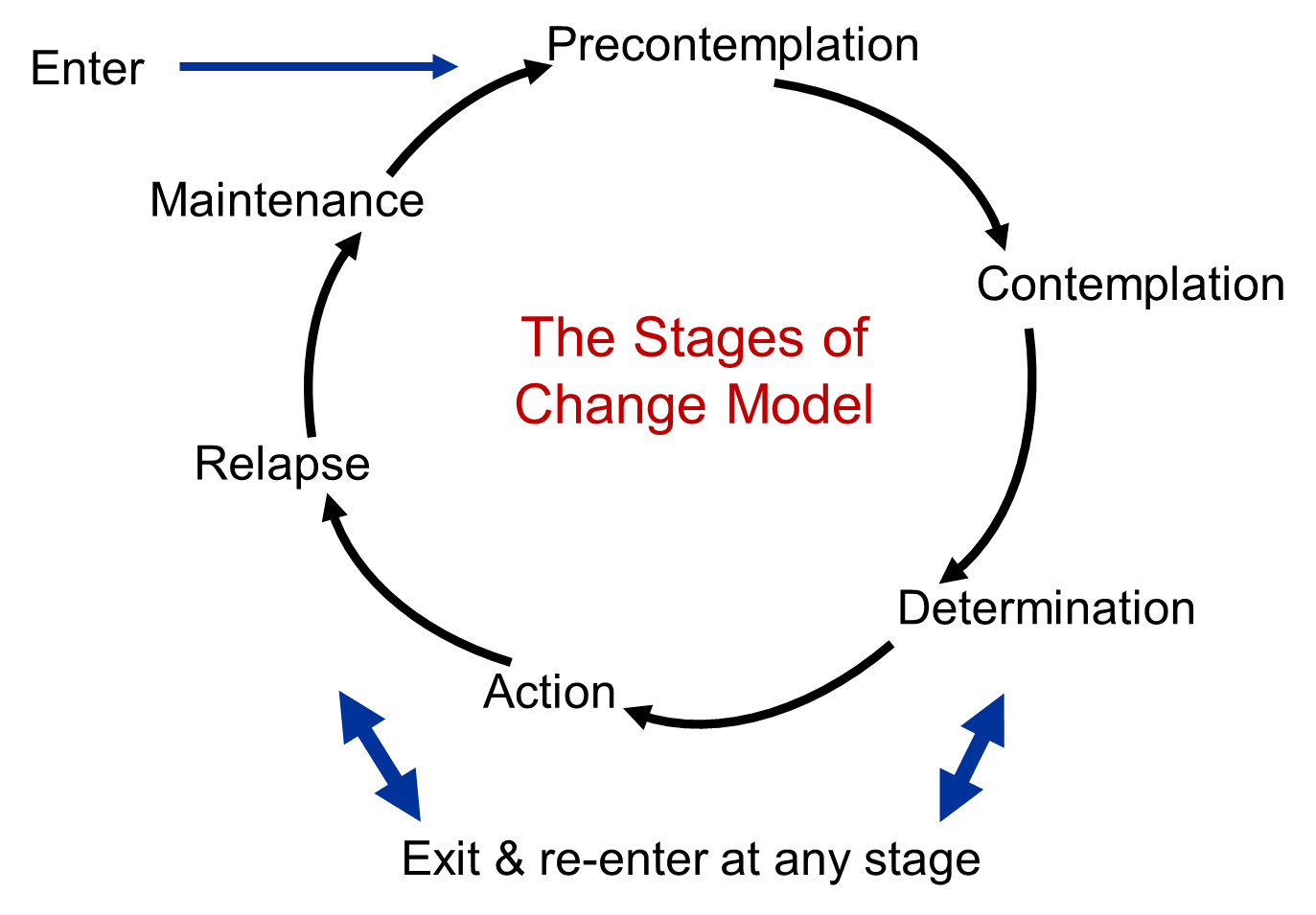
The Transtheoretical Model (Stages of Change)
The Transtheoretical Model (also called the Stages of Change Model), developed by Prochaska and DiClemente in the late 1970s, evolved through studies examining the experiences of smokers who quit on their own with those requiring further treatment to understand why some people were capable of quitting on their own. It was determined that people quit smoking if they were ready to do so. Thus, the Transtheoretical Model (TTM) focuses on the decision-making of the individual and is a model of intentional change. The TTM operates on the assumption that people do not change behaviors quickly and decisively. Rather, change in behavior, especially habitual behavior, occurs continuously through a cyclical process. The TTM is not a theory but a model; different behavioral theories and constructs can be applied to various stages of the model where they may be most effective.
The TTM posits that individuals move through six stages of change: precontemplation, contemplation, preparation, action, maintenance, and termination. Termination was not part of the original model and is less often used in application of stages of change for health-related behaviors. For each stage of change, different intervention strategies are most effective at moving the person to the next stage of change and subsequently through the model to maintenance, the ideal stage of behavior.
- Precontemplation - In this stage, people do not intend to take action in the foreseeable future (defined as within the next 6 months). People are often unaware that their behavior is problematic or produces negative consequences. People in this stage often underestimate the pros of changing behavior and place too much emphasis on the cons of changing behavior.
- Contemplation - In this stage, people are intending to start the healthy behavior in the foreseeable future (defined as within the next 6 months). People recognize that their behavior may be problematic, and a more thoughtful and practical consideration of the pros and cons of changing the behavior takes place, with equal emphasis placed on both. Even with this recognition, people may still feel ambivalent toward changing their behavior.
- Preparation (Determination) - In this stage, people are ready to take action within the next 30 days. People start to take small steps toward the behavior change, and they believe changing their behavior can lead to a healthier life.
- Action - In this stage, people have recently changed their behavior (defined as within the last 6 months) and intend to keep moving forward with that behavior change. People may exhibit this by modifying their problem behavior or acquiring new healthy behaviors.
- Maintenance - In this stage, people have sustained their behavior change for a while (defined as more than 6 months) and intend to maintain the behavior change going forward. People in this stage work to prevent relapse to earlier stages.
- Termination - In this stage, people have no desire to return to their unhealthy behaviors and are sure they will not relapse. Since this is rarely reached, and people tend to stay in the maintenance stage, this stage is often not considered in health promotion programs.
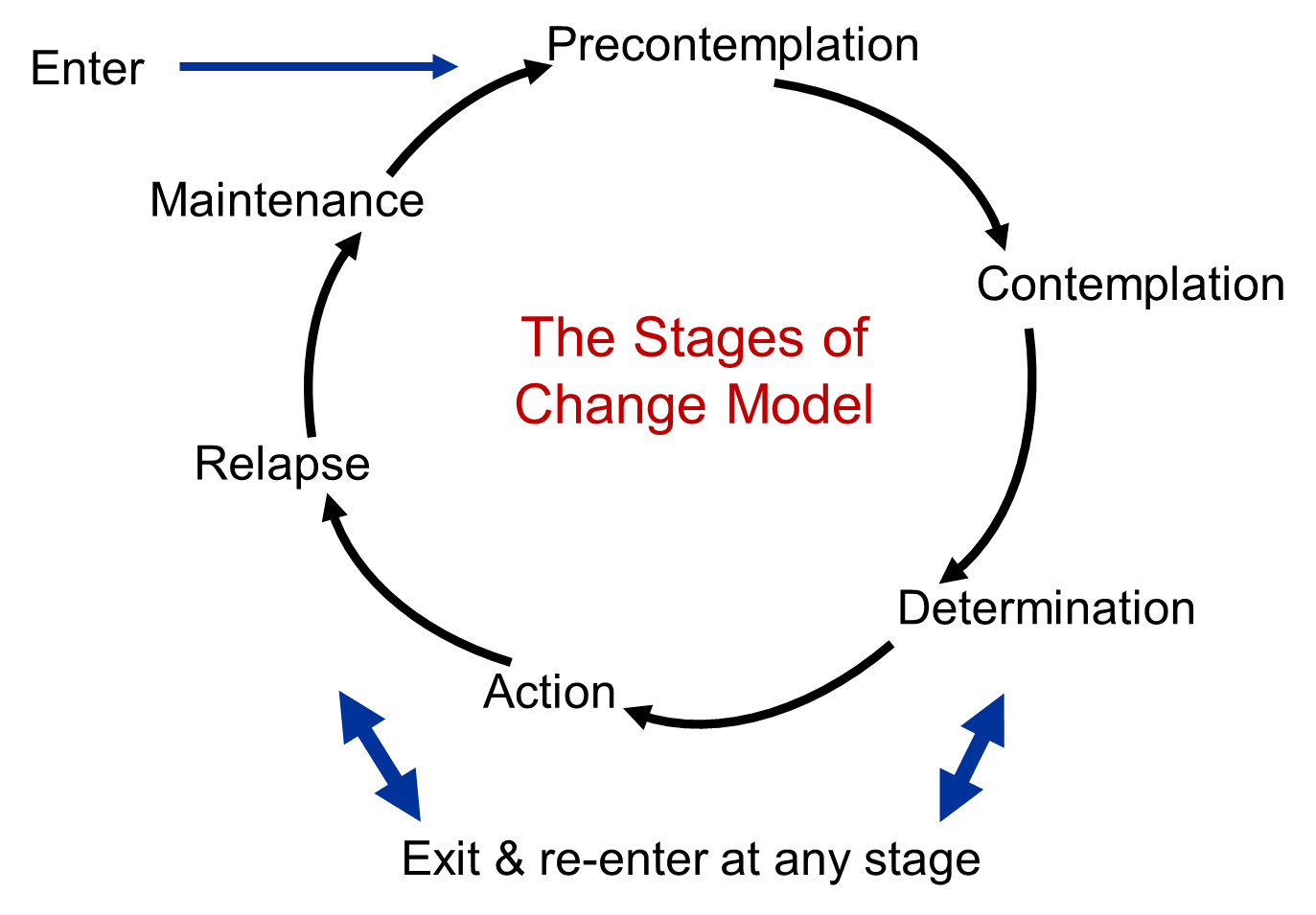
To progress through the stages of change, people apply cognitive, affective, and evaluative processes. Ten processes of change have been identified with some processes being more relevant to a specific stage of change than other processes. These processes result in strategies that help people make and maintain change.
- Consciousness Raising - Increasing awareness about the healthy behavior.
- Dramatic Relief - Emotional arousal about the health behavior, whether positive or negative arousal.
- Self-Reevaluation - Self reappraisal to realize the healthy behavior is part of who they want to be.
- Environmental Reevaluation - Social reappraisal to realize how their unhealthy behavior affects others.
- Social Liberation - Environmental opportunities that exist to show society is supportive of the healthy behavior.
- Self-Liberation - Commitment to change behavior based on the belief that achievement of the healthy behavior is possible.
- Helping Relationships - Finding supportive relationships that encourage the desired change.
- Counter-Conditioning - Substituting healthy behaviors and thoughts for unhealthy behaviors and thoughts.
- Reinforcement Management - Rewarding the positive behavior and reducing the rewards that come from negative behavior.
- Stimulus Control - Re-engineering the environment to have reminders and cues that support and encourage the healthy behavior and remove those that encourage the unhealthy behavior.
Limitations of the Transtheoretical Model
There are several limitations of TTM, which should be considered when using this theory in public health. Limitations of the model include the following:
- The theory ignores the social context in which change occurs, such as SES and income.
- The lines between the stages can be arbitrary with no set criteria of how to determine a person's stage of change. The questionnaires that have been developed to assign a person to a stage of change are not always standardized or validated.
- There is no clear sense for how much time is needed for each stage, or how long a person can remain in a stage.
- The model assumes that individuals make coherent and logical plans in their decision-making process when this is not always true.
The Transtheoretical Model provides suggested strategies for public health interventions to address people at various stages of the decision-making process. This can result in interventions that are tailored (i.e., a message or program component has been specifically created for a target population's level of knowledge and motivation) and effective. The TTM encourages an assessment of an individual's current stage of change and accounts for relapse in people's decision-making process.
Social Norms Theory
The Social Norms Theory was first used by Perkins and Berkowitz in 1986 to address student alcohol use patterns. As a result, the theory, and subsequently the social norms approach, is best known for its effectiveness in reducing alcohol consumption and alcohol-related injury in college students. The approach has also been used to address a wide range of public health topics including tobacco use, driving under the influence prevention, seat belt use, and more recently sexual assault prevention. The target population for social norms approaches tends to be college students, but has recently been used with younger student populations (i.e., high school).
This theory aims to understand the environment and interpersonal influences (such as peers) in order to change behavior, which can be more effective than a focus on the individual to change behavior. Peer influence, and the role it plays in individual decision-making around behaviors, is the primary focus of Social Norms Theory. Peer influences and normative beliefs are especially important when addressing behaviors in youth. Peer influences are affected more by perceived norms (what we view as typical or standard in a group) rather than on the actual norm (the real beliefs and actions of the group). The gap between perceived and actual is a misperception, and this forms the foundation for the social norms approach.
The Social Norms Theory posits that our behavior is influenced by misperceptions of how our peers think and act. Overestimations of problem behavior in our peers will cause us to increase our own problem behaviors; underestimations of problem behavior in our peers will discourage us from engaging in the problematic behavior. Accordingly, the theory states that correcting misperceptions of perceived norms will most likely result in a decrease in the problem behavior or an increase in the desired behavior.
Social norms interventions aim to present correct information about peer group norms in an effort to correct misperceptions of norms. In particular, many social norms interventions are social norms media campaigns where misperceptions are addressed through community-wide electronic and print media that promote accurate and healthy norms about the health behavior. The phases of a social norms media campaign include:
- Assessment or collection of data to inform the message
- Selection of the normative message that will be distributed
- Testing the message with the target group to ensure it is well-received
- Selection of the mode in which the message will be delivered
- Amount, or dosage, of the message that will be delivered
- Evaluation of the effectiveness of the message
Social norms media campaigns are currently being funded by many federal agencies, state agencies, foundation grants, and non-profit organizations. Sometimes social norms media campaigns are funded by industry. There has been a good deal of evaluations conducted on social norms campaigns.
There are several limitations of Social Norms Theory that need to be considered prior to using the theory. Limitations of the theory include the following:
- Participants of an intervention focused on social norms are likely to question the initial message being presented to them due to misperceptions they hold. Information must be presented in a reliable way to correct those misperceptions.
- Poor data collection in the initial stages can lead to unreliable data and poor choice of normative message. This can undermine the campaign and reinforce misperceptions.
- Unreliable sources, or sources that are not credible to the target population, can result in an unappealing message that undermines the campaign, even if the message is correctly chosen.
- The dose, or amount, of the message received by the target population must be enough to make an impact, but not too much that it becomes commonplace.
Although these limitations exist, when used correctly Social Norms Theory can be very effective in changing individual behavior by focusing on changing misperceptions at the group level. Social norms interventions can be used alone or in conjunction with other types of intervention strategies. The most effective social norms interventions are those that have messages targeted to the at-risk population that are correct and influential. To target messages, a substantial amount of research and data collection has to be invested to understand the norms that exist in the group of interest. Social norms interventions are also most effective when presented in interactive formats that actively engage the target audience.