Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is a global health problem that affects millions of people and is an important cause of morbidity, mortality, and extensive utilization of health care resources. COPD is one of the top ten causes of death worldwide, and the direct costs of treating COPD in the United States alone are estimated to be around $30 billion per year. COPD actually represents a spectrum of disease ranging from destruction of the alveoli and thickening of the terminal airways on one extreme (emphysema) to thickening of the airways with chronic inflammation and repeated bouts of infection (chronic bronchitis) on the other extreme. Most frequently there are elements of both of these clinical pictures.
The likelihood of COPD is heavily influenced by both environmental/behavior risk factors and by hereditary factors. In most cases, COPD is caused by chronic inhalation of harmful particles and gases (e.g., in tobacco smoke), which triggers pathophysiologic changes in the small airways, in the alveoli, and in blood vessels in the lung. All smokers have inflammation in their lungs and airways, and they all have thickening of the airways, damage to ciliated cells, and hypersecretion of mucus. Immune fun
In addition, the normal processes for breakdown and repair of cellular elements and immune defense are impaired. These abnormalities produce a spectrum of largely irreversible changes ranging from mucous hypersecretion (chronic bronchitis), to chronic small airway inflammation and fibrosis (bronchiolitis), and outright tissue destruction and impaired airflow (emphysema).
One of the hallmarks of COPD is reduced airflow, which occurs as the result of one or more of the following:
- Loss of elastic recoil in the alveoli due to excessive breakdown of the protein elastin
- Destruction of the walls between the alveoli as a result of excessive action of enzymes called "proteases".
- Thickening of the walls of the airways due to chronic inflammation.
- Excessive secretion of mucus, which can clog the airways.
The clinical manifestations of COPD are labored breathing and shortness of breath, cough, hypoxemia , and excessive mucous production. Once the fundamental changes of COPD, they are irreversible, but individuals with COPD will intermittently experience acute exacerbations
, and excessive mucous production. Once the fundamental changes of COPD, they are irreversible, but individuals with COPD will intermittently experience acute exacerbations during episodes of lung infection. These episodes can be treated, but the underlying pathology remains unchanged.
during episodes of lung infection. These episodes can be treated, but the underlying pathology remains unchanged.

Adapted from http://www.nature.com/nature/journal/v489/n7417_supp/full/489S2a.htm
Spirometry
Spirometry is a method of measuring changes in airflow during inspiration and expiration, and it provides a sensitive way of identifying abnormalities in ventilatory function .The first image below on the left shows a subject breathing through a tube connected to a spirometer, which measures changes in air flow. The graph on the right shows normal changes in lung volume over time during inspiration and expiration, both at rest and during forced inspiration and expiration. Move your cursor over the lines of the graph to get a more detailed explanation.
.The first image below on the left shows a subject breathing through a tube connected to a spirometer, which measures changes in air flow. The graph on the right shows normal changes in lung volume over time during inspiration and expiration, both at rest and during forced inspiration and expiration. Move your cursor over the lines of the graph to get a more detailed explanation.
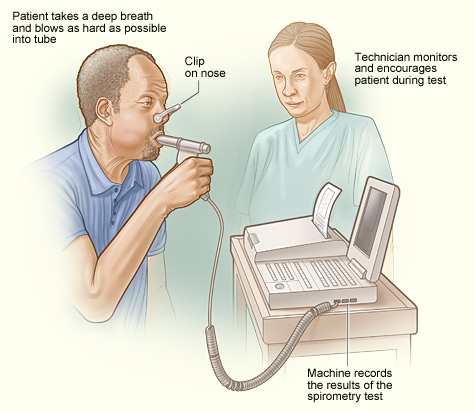
Image source: http://www.nhlbi.nih.gov/health/health-topics/topics/copd/diagnosis.html
 |
Move your cursor over the different phases of the graph to see a description. |
|
This content requires JavaScript enabled.
|
|
Spirometry is abnormal in people with COPD. The graph below on the right shows that the obstructive changes in COPD reduce the ability to expire air, and this results in an increased residual volume. As a result, the ability to move air in and out of the lungs is progressively impaired, ultimately leading to diminished oxygenation of blood. Move your cursor over the phases of the line graph for a more complete explanation.
The graph below on the left from Fletcher and Peto shows the natural history of changes in FEV1 in non-smokers, smokers, and smokers who quit smoking. Note that decreases in FEV1 lead to symptoms, disability, and death.
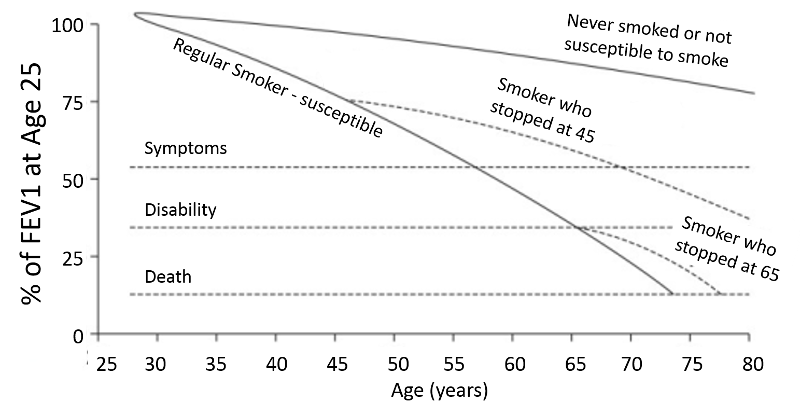
Modified from Fletcher C. and Peto R.: The natural history of chronic airflow obstruction. Br Med J. 1977;1(6077):1645–1648.
,
 |
Move your cursor over the different phases of the graph to see a description. |
|
This content requires JavaScript enabled.
|
|
Causes of COPD
Table - Frequency and Activity of Several Known Genotypes for Alpha-1 Antitrypsin
|
Genotype |
Fraction of Population |
Activity (% of normal MM genotype) |
|---|---|---|
|
MM |
0.90 |
100% |
|
MZ |
0.038 |
60% |
|
SS |
0.001 |
55% |
|
SZ |
0.0012 |
33% |
|
ZZ |
0.0004 |
12% |
Adapted from Larsson C. Acta Med. Scand. 1978;204:345-351
COPD is a chronic progressive disease, and, eventually the pathophysiologic changes in the lung lead to chronic inflammation, destruction of alveoli, impaired ventilation (air trapping), and hypoxemia with progressive disability frequently leading to premature death.. The patient in the photograph below illustrates the clinical features of end-stage COPD. Notice that he is wearing a nasal c annula that is providing supplemental oxygen. He is thin due to muscle wasting, which is characteristic of end stage COPD, but he is "barrel-chested" due to chronic air trapping. Because of the airway obstruction and difficulty in moving air, he is hunched forward with his hands on his knees in order to enable him to use his accessory muscles of respiration, i.e., muscles in his neck and shoulders and chest wall. Note also that he is pursing his lips; this enables him to increase airway pressure during expiration in order to prevent from airway collapse. The insert at the upper left side of the photo shows a blackened lung that was removed from a chronic smoker.
with progressive disability frequently leading to premature death.. The patient in the photograph below illustrates the clinical features of end-stage COPD. Notice that he is wearing a nasal c annula that is providing supplemental oxygen. He is thin due to muscle wasting, which is characteristic of end stage COPD, but he is "barrel-chested" due to chronic air trapping. Because of the airway obstruction and difficulty in moving air, he is hunched forward with his hands on his knees in order to enable him to use his accessory muscles of respiration, i.e., muscles in his neck and shoulders and chest wall. Note also that he is pursing his lips; this enables him to increase airway pressure during expiration in order to prevent from airway collapse. The insert at the upper left side of the photo shows a blackened lung that was removed from a chronic smoker.

Image sources: http://meded.ucsd.edu/clinicalmed/lung.htm (patient) and http://www.myvmc.com/diseases/emphysema (lung)
References for COPD:
- Angelis N, Porpodis K, et al.: Airway inflammation in chronic obstructive pulmonary disease. J Thorac Dis 2014;6(S1):S167-S17.
- Brode SK, Ling SC, Chapman KR: Alpha-1 antitrypsin deficiency: a commonly overlooked cause of lung disease. CMAJ 2012;184(12):1365-71.
- Rennard S and Vestbo J: Natural histories of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008 Dec 15;5(9):878-83.
- Tuder RM and Petrache I: Pathogenesis of chronic obstructive pulmonary disease. J. Clin. Invest. 2012;122(8):2749–2755.
- Vijayan VK: Chronic obstructive pulmonary disease. Indian J Med Res. 2013;137(2): 251–269.
- Yang IA, Ko FW-S, Lim TK, and Hancox RJ: Year in review 2012: Asthma and chronic obstructive pulmonary disease. Respirology 2013;18:565–572.