Looking Forward: The Future of Polio
In 1988, the 41st World Health Assembly (WHA) declared a goal to eradicate polio by 2000. Tremendous progress has been made, yet polio persists 13 years after the launch of the Global Polio Eradication Initiative's initial goal. In 2012, with the continuing urgency toward reaching eradication, the WHA declared polio eradication a global public health programmatic emergency.
Type 2 poliovirus has been eradicated, yet Type 1 persists at high levels and Type 3 at low levels (33). Today, global health leaders continue to fight for progress toward eradicating the final 1%.
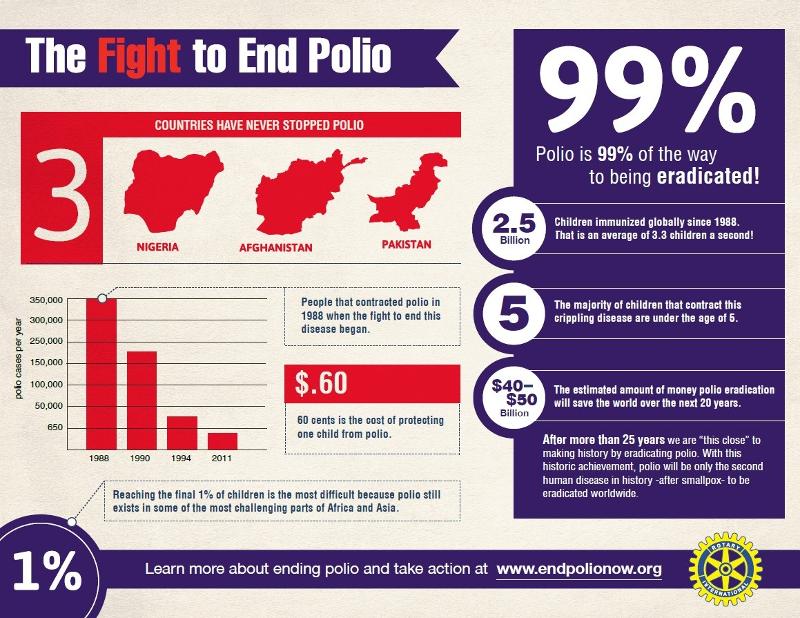
Figure 21 Rotary International's Campaign: 'The Fight to End Polio' (34)
Eradication: Why It Matters
As of 2013, the polio eradication effort has prevented paralysis in more than 10 million people. Vaccination campaigns have also promoted other health issues including the systematic administration of Vitamin A, which alone has stopped 1.5 million childhood deaths (35).
Furthermore, beyond the humanitarian benefits of eradicating a debilitating and preventable disease, the economic benefits are immense. The net benefit of the eradication effort has been estimated to be between 40-50 billion dollars from 1988 through 2035. Developing countries account for approximately 85% of these net benefits, an enormous amount that can go a long way toward other public health goals (36).
Eradication: Where We Stand
The WHO issued 'The Polio Eradication & Endgame Strategic Plan 2013-2018.' This optimism illuminates a world free of polio in the near future (37).
The plan has four primary objectives:
1. Detect and stop polio worldwide by 2014
2. Eliminate the use of OPV and implement stronger immunization systems
3. Implement a certification process stating regions have gone three years without an incident case
4. Plan polio's legacy on sharing eradication knowledge and expertise
Biology & Technology: Working With Us
As polio can only live in humans, animal vectors and animal reservoirs are not sources for the disease transmission. Therefore, eradication efforts need only to focus on humans. Despite the high level of communicability of polio, the limited incubation period reduces the period for shedding, primarily in the feces, to occur.
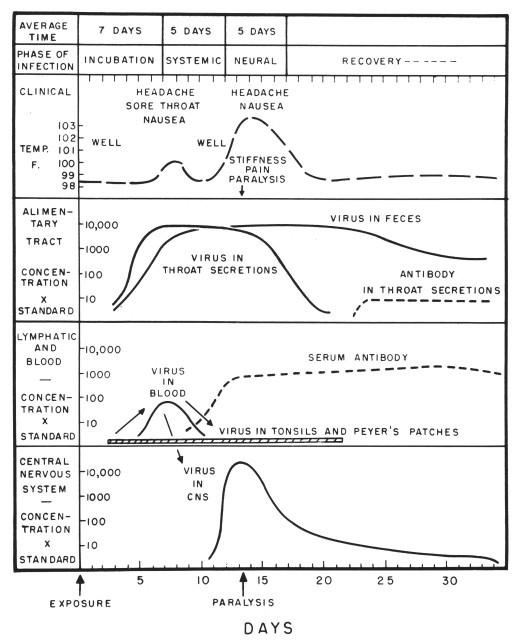
Figure 22 Timeline of the Biological Presentation of Poliovirus Infection from an American Medical Textbook published in 1959 (38)
The polio vaccines have been one of the greatest contributors to the possibility of polio eradication. In particular, community health workers without advanced medical training can administer the OPV. This has allowed access to communities hesitant toward outsider intervention and areas difficult to reach due to conflict or other mitigating factors.
Technology preserving vaccines has also been developed ensuring vaccine effectiveness since high temperatures can compromise performance. Vial monitors indicate if a vaccine's effectiveness has been compromised due to heat. If vaccines become ineffective, vial monitors will change color indicating ineffectiveness (39).

Figure 23 Vaccine vial monitors (39)
When outbreaks occur in regions previously declared polio free, quick response is of the utmost importance. A type 1 polio outbreak occurred in China in 2011. The virus was detected in a 16-month-old girl who had no history of travel outside of Xinjiang. 21 cases were confirmed between July 3 and October, 2011 and the Chinese Ministry of Health issued the highest public health emergency possible. Daily surveillance began and more than 5 million vaccines were delivered to Xinjiang for the first vaccine campaign launched by September 8. In total from August 2011 to April 2012, 43.7 million doses of OPV were administered via five supplementary immunization rounds. The outbreak was stopped 1.5 months after laboratory confirmation demonstrating how China's immediate and intense response was able to prevent a potentially devastating epidemic in the world's most populous country (40).
Biology & Technology: Working Against Us
One of the biggest obstacles is the lack of clinically visible symptoms of individuals infected. The disease can spread silently with at least 200 infected, asymptotic individuals for every one reported paralyzed polio case. This can lead to transmission unknowingly occurring within communities (41). Professor D.A. Henderson, who headed the international effort to eradicate smallpox, cites this feature as one of the biggest challenges regarding polio eradication. He said during an interview, "There were no [smallpox] patients with subclinical infections. Thus, we could readily identify infected areas and contain the outbreaks" highlighting his skepticism toward polio eradication (42).
Another obstacle is the highly communicable nature of the disease and cross-border transmission. Polio had not been seen in Somalia since 2007, yet between April 2013 through October 1, 2013, 175 cases were reported illustrating the rapid nature of disease transmission across borders. Fourteen cases were also discovered in Kenya since the last confirmed cases in July 2011 (43). The map below of poliovirus cases in the world illustrates how clusters of countries often emerge.
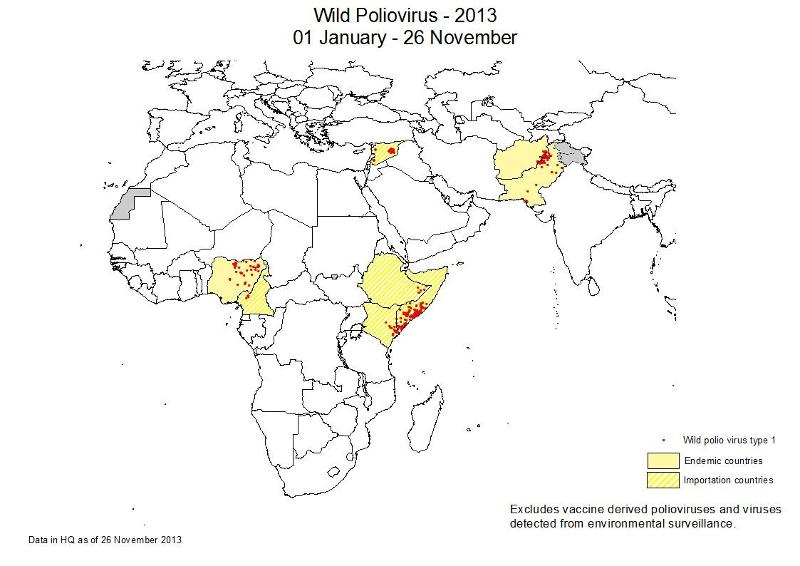
Figure 24 Districts with cases caused by wild poliovirus (44)
|
A case study of vaccine efficacy Issues with vaccine effectiveness in certain regions of the world have also occurred as demonstrated in Northern India. The trivalent oral vaccine was unable to efficiently treat the disease despite immunization coverage in children in the area. High prevalence of diarrhea and other diseases required a more potent vaccine. This outbreak demonstrated the need for proper surveillance for factors potentially impacting vaccination effectiveness. For more on this study and the crucial nature of proper surveillance, please see [link to pdf] |
The Human Factor
Other contributing factors hampering polio eradication efforts have been faulty management and oversight practices for mass vaccination campaigns, community mistrust of the safety of vaccines, inaccessible populations due to migration or conflict, and insufficient financing for programs (41).
Recently Syria has seen cases of polio for the first time in 14 years. Polio is often spread in war-torn communities as health infrastructures, including clean water and adequate sanitation, become compromised. Access to immunization is often threatened as well; immunization rates have dropped to less than 70% compared to 90% in 2010. Vaccination campaigns have been planned however the success of them is unknown at this time. As Siddharth Chatterjee notes discussing the Syrian outbreak, "Principles over politics must be the clarion call when it comes to children and their wellbeing, everywhere" (46).
Polio has become a top public health priority over the last 20-years and advocates have been successful in garnering global support financially, politically, and socially which have lead to enormous strides in the fight against polio. CDC and WHO initiated the Stop Transmission of Polio (STOP) program in 1999. Since then, it has mobilized 1,563 volunteers in 69 countries. The program has strengthened capacity of immunization program in countries and supported the surveillance of acute flaccid paralysis (47). WHO's financial and technical support have been instrumental in initiating polio as a top public health priority and will be needed for eradicating that final 1%.
| Additional Information:
For weekly reports on the status of polio worldwide, please visit: http://www.polioeradication.org/Dataandmonitoring/Poliothisweek.aspx To learn even more, an engaging talk on the public health successes and challenges in fighting polio [23:09] |
