Diet and Heart Disease
[See Walter Willett: Dietary Fats and Coronary Heart Disease. J. Intern. Med. 2012; 272: 13–24.]
In the 1970s several observations pointed to a potential relationship between diet and coronary heart disease. The Seven Countries Study by Ancel Keys found that the per capita consumption of dietary cholesterol and saturated fat correlated with mortality from coronary heart disease, and studies in animals also pointed to dietary lipids as a risk factor for atherosclerosis. These studies spawned the widespread recommendations for decreasing dietary cholesterol, decreasing the percentage of dietary calories obtained from fat, and replacing dietary saturated fat with polyunsaturated fat.
found that the per capita consumption of dietary cholesterol and saturated fat correlated with mortality from coronary heart disease, and studies in animals also pointed to dietary lipids as a risk factor for atherosclerosis. These studies spawned the widespread recommendations for decreasing dietary cholesterol, decreasing the percentage of dietary calories obtained from fat, and replacing dietary saturated fat with polyunsaturated fat.
Hu F, Stampfer MJ, Manson JE et al. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med 1997;337:1491–9.
This study, using the Nurses' Health Study cohort, analyzed data from 80,082 women free of diagnosed coronary heart disease (CHD) in 1980. Dietary composition for each subject was assessed diet in 1980 using a 61-item food frequency questionnaire, and the assessment was repeated at 4-year intervals. During the subsequent 14 years of follow-up, there were 939 cases of acute myocardial infarction or death from coronary heart disease. For the analysis, the cohort was divided into quintiles for the percentage of energy obtained from each type of fat, and for each type of fat, the rate ratio for each quintile was computed using the group with the lowest intake of a given fat type as the reference. A multivariate analysis was conducted to adjust for age and other confounding variables. A separate analysis used multiple linear regression and treated dietary fat intakes as continuous variables. They then used the coefficients from these models to the estimate the effect of substituting a specific percentage of energy from fat for the same percentage of energy from carbohydrates. The results of these projects are shown in the figure below.
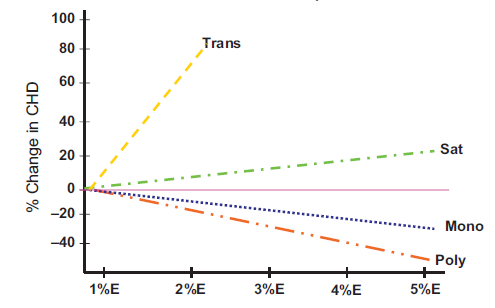
Source: Hu F, et al. N Engl J Med 1997;337:1491–9
In essence, this analysis uses different percentages of carbohydrate intake as a reference (the horizontal purple line) and compares the risk expected with substitution of a given percentage of energy from fat (trans fat, saturated, monounsaturated, or polyunsaturated). Substitution of 5% of carbohydrate energy intake with saturated fat was associated with a 17% increase in the risk of coronary disease (rate ratio, 1.17; 95 % confidence interval, 0.97-1.41; P=0.10). Substitution of 2% of energy from carbohydrates with equivalent calories from trans unsaturated fat was associated with almost a doubling of risk (rate ratio=1.93 (95% confidence interval, 1.43-2.61; P=0.001). Substitution of 5% of energy from monounsaturated fat was associated with a 19% decrease in risk (rate ratio = 0.81 (95% confidence interval, 0.65-1.00; P=0.05). Finally, substitution of 5% of energy from polyunsaturated fat was estimated to be associated with a 38% reduction in risk of coronary heart disease (rate ratio = 0.62 (95% confidence interval, 0.46-0.85; P=0.003). Total fat intake was not significantly related to the risk of coronary disease; for a 5 percent increase in energy from fat versus carbohydrate, the rate ratio was 1.02; 95 percent confidence interval, 0.97-1.07; P=0.55). The authors also estimated that the replacement of 5 percent of energy from saturated fat with energy from unsaturated fats would reduce risk by 42% (95% confidence interval, 23-56; P=0.001) and that the replacement of 2 percent of energy from trans fat with energy from unhydrogenated, unsaturated fats would reduce risk by 53% (95% confidence interval, 34%-67%; P=0.001). The results of this study were largely confirmed in a meta-analysis that included results from 11 cohort studies. The meta-analysis found that the percentage of calories from saturated fat was not associated with higher risk of coronary heart disease when compared to the same percentage of energy from carbohydrates (risk ratio = 0.97, 95% CI 0.81–1.16), but saturated fat was associated with higher risk if compared to polyunsaturated fat (RR = 1.25, 95% CI 1.01–1.56). Like the previous study, it found that the overall percentage of energy from fat was not associated with risk of CHD.
that included results from 11 cohort studies. The meta-analysis found that the percentage of calories from saturated fat was not associated with higher risk of coronary heart disease when compared to the same percentage of energy from carbohydrates (risk ratio = 0.97, 95% CI 0.81–1.16), but saturated fat was associated with higher risk if compared to polyunsaturated fat (RR = 1.25, 95% CI 1.01–1.56). Like the previous study, it found that the overall percentage of energy from fat was not associated with risk of CHD.
Howard BV, Van Horn L, Hsia J et al. Low-fat dietary pattern and risk of cardiovascular disease the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006;295:655–66.
The Women's Health Initiative conducted a very large randomized clinical trial to examine the effect of a low fat diet on breast cancer and heart disease. The type of fat in the diet was not appreciably altered. A total of 48,000 women were randomly assigned to the low fat diet or their usual diet. The low fat diet had no effect on CHD after an average follow-up of 8 years (RR= 0.97; 95% CI 0.90–1.06) or total cardiovascular disease. This study also found no effect on plasma HDL cholesterol or triglycerides, possibly because of poor adherence resulting in minimal difference in fat intake.
de Lorgeril M, Renaud S, Mamelle N et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 1994;343:1454–9. (The Lion Heart Diet Study)
In Ancel Keys's Seven Countries study a Greek/Mediterranean style diet was associated with the lowest risk of CHD. The Mediterranean diet was mostly vegetarian and consisted of a variety of vegetables, fruits, legumes, nuts, seeds and unrefined cereals. There is high intake of olive oil, but low intake of saturated fat, moderately high intake of fish, low-to-moderate intake of dairy products (mostly cheese or yogurt), low intake of meat and poultry, and regular but moderate intake wine. The inclusion of vegetables, seeds, fish, and olive oil provide a source of omega-3 and monounsaturated fatty acids. The Lyon Diet Heart Study enrolled subjects with known CHD and randomly assigned them to a Mediterranean diet or to an American Heart Association "step 1 diet," which is a low-fat diet (total fat <30% of energy intake; saturated fat <10%). Subjects were followed for 48 months. Remarkably, while the Mediterranean diet had little effect on plasma lipids, these subjects experiences a 70% reduction in CHD events compared to the AHA control diet. Given the multiple differences between the two diets, it was impossible to attribute the benefits to any particular aspect of diet composition.
Dean Ornish
Dean Ornish has also advocated a multi-pronged approach with lifestyle changes that include low-fat vegetarian food, smoking cessation, regular exercise, and meditation. His findings suggest that adopting this type of lifestyle can not only stop the progression of coronary arterial disease but actually reverse it. The video below is a 15 minute TED talk in which Dr. Ornish summarizes his approach. Note that some of his dietary recommendations differ markedly from the Mediterranean style diet. Two other details are perhaps noteworthy in his talk. First, he recommends reducing dietary fat primarily because fat is calorie dense (9 kcal/gram) compared to carbohydrates or protein (each with 4 kcal/gram). Second, he recommends dietary supplementation with 3 grams of fish oil per day in order to boost omega-3 fatty acids.
Types of Dietary Fats and Fatty Acids
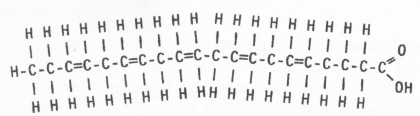
The studies described above point to the potential importance of different types of dietary fat. The adipose tissue consists of cells (adipocytes) filled with triglyceride. All triglycerides have the same basic structure and consist of a three carbon glycerol backbone with fatty acids (acyl groups) attached to each of the carbons in the glycerol backbone as illustrated below.
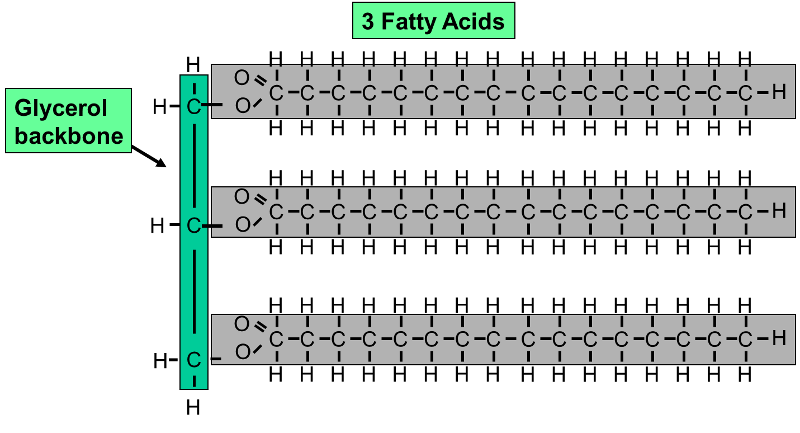
This example shows a triglyceride (fat) molecule with three saturated fatty acids with the same number of carbon atoms in each of the three chains. In reality, there are many "species" of fatty acids which differ in the number of carbon atoms in the acyl chain and the number and location of carbon-carbon double bonds in the acyl chain. Examples of some of the more common naturally occurring fatty acids are shown in the table below.
|
Examples of Different Types of Dietary Fatty Acid and Their Nomenclature |
|
|---|---|
|
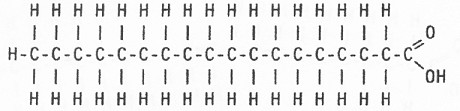
Stearic acid, 18:0 is a saturated fatty acid because it has no double bonds between the carbon atoms in the hydrocarbon chain. |
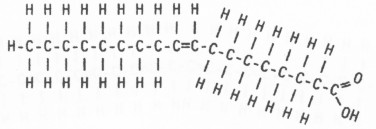
Oleic acid, 18:1, w9 This is the most abundant fatty acid in olive oil. It is monounsaturated and has a cis double bond that produces a kink in the acyl chain. The notation "w9" indicates that it is an omega-9 fatty acid because the double bond is located after the ninth carbon from the methyl end (the left end in this image) |
|
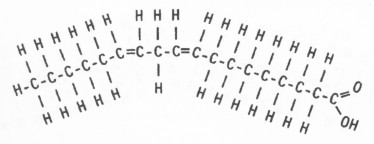
Linoleic acid, 18:2, w6 This is a polyunsaturated fatty acid that is abundant in corn oil. It has two cis double bonds. It is designated "w6", i.e., omega-6 because the first double bond is located after the sixth carbon from the methyl end, which is on the left here. |
Eicosapentaenoic acid, 20:5, w3 EPA is a highly polyunsaturated fatty acid that is found in fish oil from deep water fish like salmon. It is designated "w3", i.e., omega-3 because the first double bond is located after the third carbon from the methyl end, which is on the left here. |
|
Docosahexaenoic acid, 22:6, w3 DHA is also a highly polyunsaturated fatty acid that is found in fish oil from deep water fish like salmon. Like EPA, it is an omega-3 fatty acid because the first double bond is located after the third carbon from the methyl end of the acyl chain, which the on the left here.
|
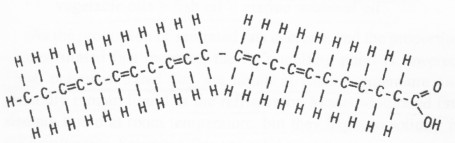
Source: Mozalfarian, D. et al.: N Engl J Med 2006; 354:1601-1613 These are both monounsaturated fatty acids with 18 carbons in the acyl chain. The fatty acid on the left is oleic acid, which has a cis double bond which characteristically produces a kink in the chain. The fatty acid on the right has a trans double bond which results in a straight chain. |
Triglycerides from naturally occurring sources can have a wide variety of fatty acids, and the table below illustrates some of this variability. It is important to note that none of the fats in the table below consist of just a single species of fatty acid; they are all mixtures.
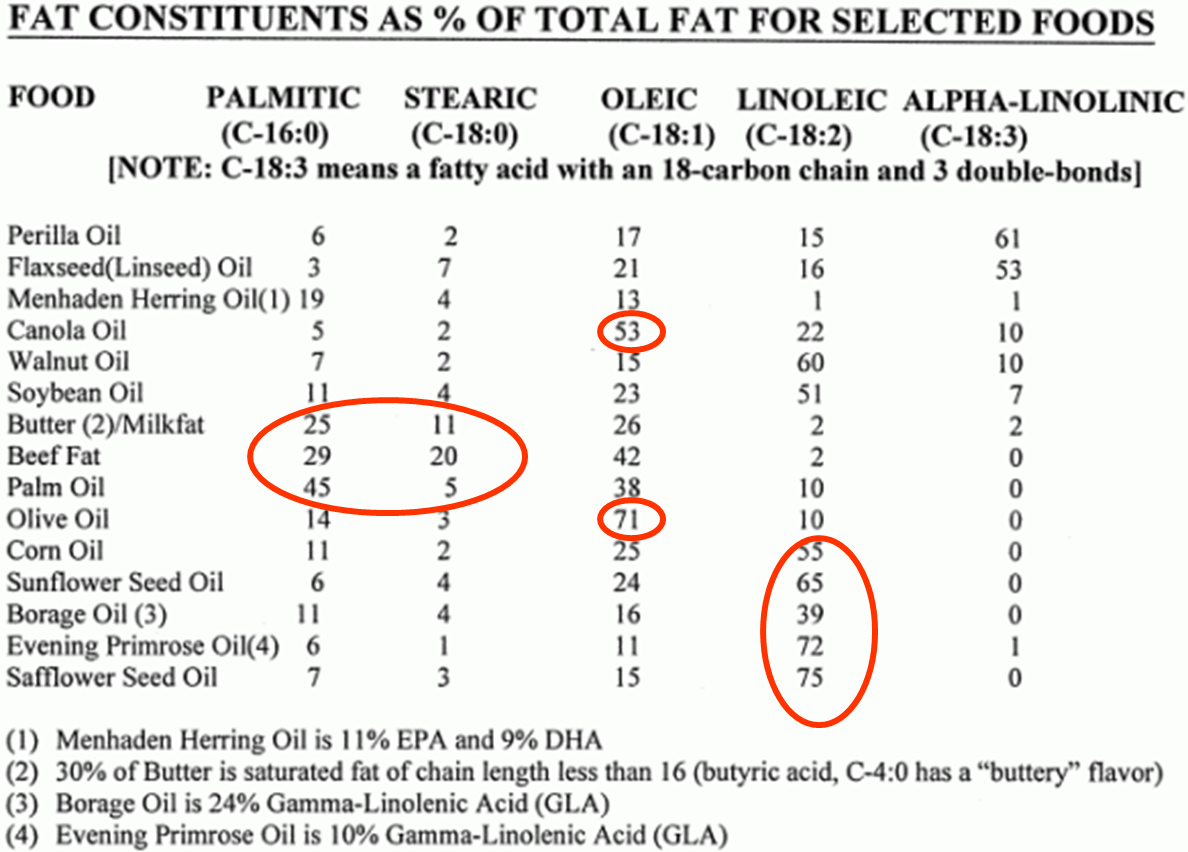
Note in the table that canola oil and olive oil have a very high percentage of oleic acid, a monounsaturated fatty acid with 18 carbon atoms and a single double bond in the 9 position. However, while we refer to canola oil and olive oil as "monounsaturated fats," note that both of them also have some polyunsaturated fatty acids (linoleic and alpha-linolenic) and some saturated fatty acids (palmitic acid and stearic acid). Similarly, corn oil and sunflower oil are referred to as polyunsaturated fats, because they contain a high percentage of linoleic acid. However, these "polyunsaturated fats" also contain lesser amounts of saturated and monounsaturated fatty acids. Fish oil (see Menhaden Herring Oil in the footnote) is sometimes referred to as "highly polyunsaturated," because it has EPA and DHA which have 5 and 6 double bonds in their chains respectively. Nevertheless, note that herring oil contains only 11% EPA and 9% DHA. In addition, fish oil also contains a mixture of saturated, monounsaturated, and polyunsaturated fatty acids. It's just that fish oil has relatively more of the highly unsaturated omega-3 fatty acids than other types of oils.
Omega-3 Fatty Acids in Fish Oil
Many clinicians recommend dietary supplementation with fish oil, but the efficacy of fish oil supplementation remains controversial. Early ecologic studies identified low rates of CHD in Japan and Greenland, which raised the possibility that consumption of fish might be beneficial, possibly by inhibiting platelet adhesion and blood clotting, by reducing blood triglyceride concentrations, or perhaps by reducing arrhythmias. There have been a number of studies that have found beneficial effects, but others that did not. In 1985 Kromhout et al. published the results of a prospective cohort study conducted in Zutphen in the Netherlands. They found an inverse relationship between fish consumption reported in 1960 and the rate of coronary heart disease mortality occurring overt the subsequent 20 years of follow-up. In 2006 Mozaffarian and Rimm conducted a meta-analysis of cohort studies and clinical trials and concluded that a daily intake of 250 mg of EPA and DHA reduced the risk of fatal coronary heart disease by 36%. In 2008 a review of the literature by Artham et al. concluded: ",,, all clinicians should strongly consider therapy with fish oil, specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), for patients with known cardiovascular disease and for patients at increased risk for cardiovascular disease.... The target DHA + EPA consumption levels are about 800 to 1000 mg/d for individuals with known CHD and at least 500 mg/d for individuals without disease." In 2009 Hernando León, et al. conducted a meta-analysis which was published in the British Medical Journal
which raised the possibility that consumption of fish might be beneficial, possibly by inhibiting platelet adhesion and blood clotting, by reducing blood triglyceride concentrations, or perhaps by reducing arrhythmias. There have been a number of studies that have found beneficial effects, but others that did not. In 1985 Kromhout et al. published the results of a prospective cohort study conducted in Zutphen in the Netherlands. They found an inverse relationship between fish consumption reported in 1960 and the rate of coronary heart disease mortality occurring overt the subsequent 20 years of follow-up. In 2006 Mozaffarian and Rimm conducted a meta-analysis of cohort studies and clinical trials and concluded that a daily intake of 250 mg of EPA and DHA reduced the risk of fatal coronary heart disease by 36%. In 2008 a review of the literature by Artham et al. concluded: ",,, all clinicians should strongly consider therapy with fish oil, specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), for patients with known cardiovascular disease and for patients at increased risk for cardiovascular disease.... The target DHA + EPA consumption levels are about 800 to 1000 mg/d for individuals with known CHD and at least 500 mg/d for individuals without disease." In 2009 Hernando León, et al. conducted a meta-analysis which was published in the British Medical Journal . The subjects were patients who had had a myocardial infarction, or revascularization of implantation of a defibrillator. They concluded, "Fish oil supplementation was associated with a significant reduction in deaths from cardiac causes but had no effect on arrhythmias or all cause mortality. Evidence to recommend an optimal formulation of EPA or DHA to reduce these outcomes is insufficient."
. The subjects were patients who had had a myocardial infarction, or revascularization of implantation of a defibrillator. They concluded, "Fish oil supplementation was associated with a significant reduction in deaths from cardiac causes but had no effect on arrhythmias or all cause mortality. Evidence to recommend an optimal formulation of EPA or DHA to reduce these outcomes is insufficient."
Nevertheless, more recent large trials have failed to confirm the efficacy of fish oil supplementation in high risk patients.
The ORIGIN Trial Investigators n–3 Fatty Acids and Cardiovascular Outcomes in Patients with Dysglycemia. N Engl J Med 2012 367309-318.
This double-blind randomized trial examined the effect of 1 gram of fish oil per day compared to a "placebo" containing 1 gram of olive oil in 12,536 subjects who were at high risk of a cardiac event. All patients had a past history of myocardial infarction, stroke, angina with documented ischemia, or revascularization, and all had marginally abnormal fasting blood sugars. It should be noted that, given their past history of heart disease, all of these subjects were already receiving optimal medical therapy that included medications to control blood pressure, aspirin or other anticoagulant therapy, statins, and smoking cessation counseling.
"During a median follow up of 6.2 years, the incidence of the primary outcome was not significantly decreased among patients receiving n–3 fatty acids, as compared with those receiving placebo (574 patients [9.1%] vs. 581 patients [9.3%]; hazard ratio, 0.98; 95% confidence interval [CI], 0.87 to 1.10; P=0.72). The use of n–3 fatty acids also had no significant effect on the rates of major vascular events (1034 patients [16.5%] vs. 1017 patients [16.3%]; hazard ratio, 1.01; 95% CI, 0.93 to 1.10; P=0.81), death from any cause (951 [15.1%] vs. 964 [15.4%]; hazard ratio, 0.98; 95% CI, 0.89 to 1.07; P=0.63), or death from arrhythmia (288 [4.6%] vs. 259 [4.1%]; hazard ratio, 1.10; 95% CI, 0.93 to 1.30; P=0.26). Triglyceride levels were reduced by 14.5 mg per deciliter (0.16 mmol per liter) more among patients receiving n–3 fatty acids than among those receiving placebo (P<0.001), without a significant effect on other lipids. Adverse effects were similar in the two groups."
Kromhout D, et al.: n–3 Fatty Acids and Cardiovascular Events after Myocardial Infarction. N Engl J Med 2010;363:2015-26.
These investigators conducted a multi-center, double-blind, placebo-controlled trial to examine the effect of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) from fish oil and of the plant-derived alpha-linolenic acid (ALA) in 4837 elderly patients who had already had a myocardial infarction. It should be noted here also that all of these subjects with previously documented heart disease were also receiving state-of-the-art antihypertensive, antithrombotic, and lipid modifying therapy. The investigators formulated four margarines that were supplemented with one of the following: EPA-DHA, ALA, EPA-DHA+ALA, or placebo. They randomly assigned subjects to receive one of the four margarines. The authors found that neither the EPA-DHA supplemented margarine, nor the ALA supplemented margarine reduced the incidence of major coronary events. However, it should also be noted that the actual consumption of the active agents varied depending on consumption of margarine, and the average consumption of EPA-DHA was only 226 mg of EPA and 150 mg of DHA., which is quite low.
patients who had already had a myocardial infarction. It should be noted here also that all of these subjects with previously documented heart disease were also receiving state-of-the-art antihypertensive, antithrombotic, and lipid modifying therapy. The investigators formulated four margarines that were supplemented with one of the following: EPA-DHA, ALA, EPA-DHA+ALA, or placebo. They randomly assigned subjects to receive one of the four margarines. The authors found that neither the EPA-DHA supplemented margarine, nor the ALA supplemented margarine reduced the incidence of major coronary events. However, it should also be noted that the actual consumption of the active agents varied depending on consumption of margarine, and the average consumption of EPA-DHA was only 226 mg of EPA and 150 mg of DHA., which is quite low.
Kwak SM, Myung SK, Lee YJ, Seo HG; Korean Meta-analysis Study Group. Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta-analysis of randomized, double-blind, placebo-controlled trials. Arch Intern Med. 2012;172(9):686-94.
In 2012 this study group conducted a meta-analysis of randomized clinical trials examining the effectiveness of fish oil supplementation in patients with known coronary heart disease. They concluded that there was insufficient evidence of a secondary preventive effect of omega-3 fatty acid supplements against overall cardiovascular events among patients with a history of cardiovascular disease.
In the same issue of the Archives of Internal Medicine there was an invited commentary by Dr. Frank Hu and Dr. Joanne Manson from the Department Epidemiology at Harvard School of Public Health:
|
Excerpts from an invited commentary by Frank B. Hu, MD, PhD; JoAnn E. Manson, MD, DrPH in Arch Intern Med. 2012;172(9):694-696 May 14, 2012. "Omega-3 Fatty Acids and Secondary Prevention of Cardiovascular Disease—Is It Just a Fish Tale?: Comment on "Efficacy of Omega-3 Fatty Acid Supplements (Eicosapentaenoic Acid and Docosahexaenoic Acid) in the Secondary Prevention of Cardiovascular Disease" "One question that has been raised is why more recent trials ... have not replicated significant effects of fish oil supplementation on secondary prevention of CVD that were found in earlier trials. Differences in study designs, population characteristics, and types and dosages of omega-3 fatty acids are possible explanations. Most important, the newer trials were each substantially underpowered and unable to detect significant small to modest benefits on CVD outcomes because of their small sample sizes and much lower-than-expected event rates. Another explanation could be that the patients in the more recent trials received much better treatment with statins and antithrombotic and antihypertensive medications than those in earlier trials. The additional benefits of fish oil supplementation or any other therapy on top of statins, β-blockers, angiotensin-converting enzyme inhibitors, and other cardiovascular medications are likely to be small; therefore, a much larger sample size is critical to achieve sufficient power. Another important question is whether fish oil has different effects in primary and secondary prevention of CVD. While waiting for more definitive results, what should physicians tell their patients? To date, there is no conclusive evidence to recommend fish oil supplementation for primary or secondary prevention of CVD. However, a diet high in fatty fish (≥2 servings of marine fish per week) should continue to be recommended for the general population and for patients with existing CVD because fish not only provides omega-3 fatty acids but also may replace less healthy protein sources, such as red meat. Individuals who are unable or unwilling to eat fish or related products should consider increasing their consumption of plant-derived omega-3 fatty acid (α-linolenic acid). For primary or secondary prevention, omega-3 supplementation cannot supersede an overall healthy diet, but a cardioprotective diet needs to be rich in omega-3 fatty acids." |
The failure of the newer trials to replicate the apparent benefits seen in earlier trials may be due to the fact that patients in the newer trials are already receiving optimal medical therapy with statins and antithrombotic and antihypertensive medications, while patients in the earlier trials for secondary prevention were not. This also leaves unanswered the question regarding the efficacy of fish oil for primary prevention of coronary heart disease. Since the incidence of significant cardiac events would be much lower in subjects with no prior history of coronary disease, a randomized clinical trial to test efficacy in these subjects would require a massive sample size and would be prohibitively expensive.
The Mediterranean Diet
In 2003 Antonia Trichopoulou and colleagues published the results of a prospective cohort study conducted in Greece showing that close adherence to a Mediterranean style diet was associated with a significant reduction in mortality from cardiovascular disease and cancer. Of interest, while the degree of adherence to a Mediterranean diet was associated with reduced mortality, there was no significant association with any particular diet component.
|
Characteristics of the Traditional Mediterranean Diet |
||
|
High Intake of: |
Moderate Intake of: |
Low Intake of: |
|
olive oil, fruit nuts vegetables cereals |
fish poultry wine in moderation with meals |
dairy products red meat processed meats sweets |
More recently, a randomized clinical trial (Estruch et al.: Primary Prevention of Cardiovascular Disease with a Mediterranean Diet, N Engl J Med; online article published Feb, 13, 2013) among subjects at high risk of developing cardiovascul
Trans Fats
Trans fats are unsaturated fatty acids with at least one double bond in the trans configuration, as illustrated by elaidic acid in the figure on the right (Source: Mozaffarian D, et al.: Trans fatty acids and cardiovascular disease. N Engl J Med 2006;354:1601-13.) Trans fats are formed by subjecting vegetable oil to a process of "hydrogenation," which was popular in the commercial food industry because of their increased their shelf life, stability during deep fat frying, and their conversion into a semisolid state at room temperature (e.g., margarine). The use of trans fats is increasingly being discouraged, but they were commonly used in fried foods, and in the manufacture of margarines and commercial baked goods, such as donuts, cookies, and crackers.
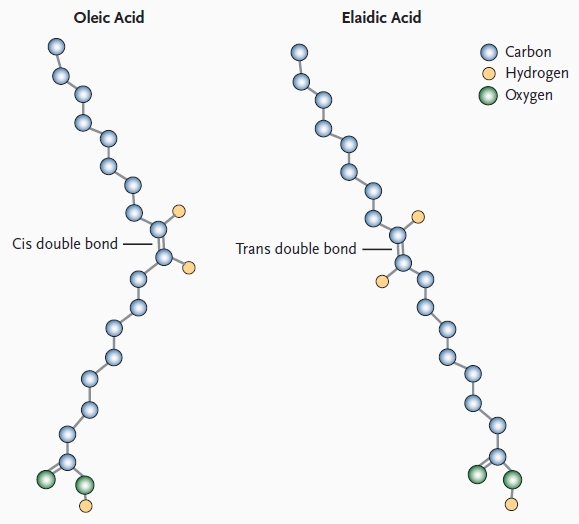
Source: Mozalfarian, D. et al.: N Engl J Med 2006; 354:1601-1613
Trans fats have several adverse effects that increase the risk of coronary heart disease:
- increase LDL cholesterol in blood; increase VLDL and triglycerides; decrease HDL; decrease LDL size
- cause endothelial cell dysfunction
- promote inflammation
- may increase the risk of sudden death from cardiac causes
The US Food and Drug Administration (FDA) now requires that nutrition labels must indicate the content of trans fatty acids, and the US Department of Agriculture recommends reducing intake of trans fats. The New York City Department of Health and has asked restaurants and food suppliers to stop using partially hydrogenated oils.
Anthocyanins (Blueberries and Strawberries)
Cassidy A, et al.: High Anthocyanin Intake Is Associated With a Reduced Risk of Myocardial Infarction in Young and Middle-Aged Women. Circulation. 2013;127:188-196.
There is growing evidence indicating that dietary flavonoids have a beneficial effect on endothelial function and blood pressure. Flavonoids are believed to improve endothelial function through an anti-inflammatory effects which reduces oxidation of LDL and increased synthesis of nitric oxide in endothelial cells. Flavonoids are found in a variety of plants and can be consumed as fruits, vegetables, tea, and wine.
These researchers used data from the Nurses' Health Study to examine the relationship between anthocyanins and other flavonoids and the risk of MI. Intake of flavonoid subclasses was calculated from validated food-frequency questionnaires collected every 4 years. They found that the highest intake of anthocyanins (upper quintile) was associated with a 32% reduction in risk of CHD (compared to the lowest quintile after adjusting for other risk factors (hazard ratio, 0.68; 95% confidence interval, 0.49–0.96; P=0.03, highest versus lowest quintiles). Combined intake of 2 anthocyanin-rich foods, blueberries and strawberries, tended to be associated with a decreased risk of MI in subjects consuming >3 servings per week (hazard ratio, 0.66; 95% confidence interval, 0.40–1.08). While these finding are intriguing, they will need to be confirmed by randomized clinical trials.
Red Meat: Choline, Carnitine, Gut Bacteria, and Trimethylamine-N-oxide (TMAO)
Red meat has been suspected of being a risk factors for heart disease for a number of years, and recent studies have provided evidence for such an association. Bernstein et al. ( Bernstein AM, Sun Q, Hu FB Stampfer MJ, Manson JE, and Willett WC: Major Dietary Protein Sources and Risk of Coronary Heart Disease in Women. Circulation. 2010;122:876-883.) prospectively followed 84,136 women aged 30 to 55 years in the Nurses' Health Study. All women were initially free of known cardiovascular disease for about 26 years. Diet was assessed periodically using a standardized questionnaire. The authors reported that higher intakes of red meat, red meat excluding processed meat, and high-fat dairy were significantly associated with elevated risk of CHD, while higher intakes of poultry, fish, and nuts were significantly associated with lower risk.
A subsequent study from Boston University School of Public Health (Ashaye A, Gaziano J, Djoussé L: Red meat consumption and risk of heart failure in male physicians. Nutr Metab Cardiovasc Dis. 2011 Dec;21(12):941-6.) reached a similar conclusion in a cohort of male physicians. Men in the highest quintile for red meat consumption had a 24% increase in risk of heart failure compared to men in the lowest quintile of consumption (risk ratio: 1.24; 95% confidence limits, 1.03-1.48.
Other recent studies suggest that the association between consumption of red meat and heart disease may be related to the metabolism of dietary choline and carnitine in the human intestine. Phoshatidylcholines (lecithins) are a family of phospholipids that are important components of all cell membranes, and dietary phosphatidylcholine the major dietary source of choline, which has several metabolic roles besides being a major component of cell membranes. It is involved in lipid metabolism and it is a precursor for the synthesis of the neurotransmitter acetylcholine. Intestinal microbial organisms (microbiota) metabolize dietary choline to trimethylamine (TMA), which is then absorbed by the intestine and tranported to the liver, where it is converted into timethylamine-N-oxide (TMAO). TMAO is believed to promote atherosclerosis by promoting the transformation of macrophages into foam cells and fostering the deposition of cholesterol in arterial lesions.
A 2013 publication in the New England Journal of Medicine provided evidence for the conversion of dietary choline to TMAO by gut microbes. [Tang WH, Wang Z, et al.: Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013 Apr 25;368(17):1575-84.] These investigators had healthy subject eat two hard-boiled eggs as a source of phosphatidylcholine and measured TMAO production. Plasma levels of TMAO increased after ingestion of the eggs, but TMAO production was markedly suppressed when broad spectrum antibiotics were given to reduce gut bacteria. These investigators also studied the relationship between fasting plasma levels of TMAO and incident cardiovascular events (death, myocardial infarction, or stroke) during 3 years of follow-up in 4007 patients undergoing elective coronary angiography. Increased plasma levels of TMAO were associated with an increased risk of cardiovascular disease even after adjustment for other know risk factors (hazard ratio = 2.54 for the highest TMAO quartile compared to the lowest; 95% confidence interval: 1.96 to 3.28; P<0.001). They concluded that production of TMAO from dietary phosphatidylcholine is dependent on metabolism by the intestinal microbiota, and that increased TMAO levels are associated with an increased risk of incident major adverse cardiovascular events.
Another recent study [Koeth RA, Wang Z, et al.: [Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013 May;19(5):576-85] provided evidence that dietary carnitine, which is abundant in red meat, can also be converted to TMAO by intestinal microbes. They found that omnivorous human subjects produced more TMAO than vegans or vegetarians after ingestion of L-carnitine. They found that specific types of gut bacteria were associated with both plasma TMAO concentration and dietary status. Moreover, higher plasma L-carnitine concentrations were found in patients with known heart disease, and higher levels of carnitine were also associated with an increased incidence of subsequent cardiovascular events (myocardial infarction, stroke or death) in 2,595 subjects who were followed after cardia evaluation . Studies in mice have shown that chronic dietary L-carnitine supplementation altered gut microbial composition and dramatically increased formation of TMA and TMAO, and increased atherosclerosis. However, this did not occur if intestinal microbe populations were suppressed by administration of broad spectrum antibiotics.
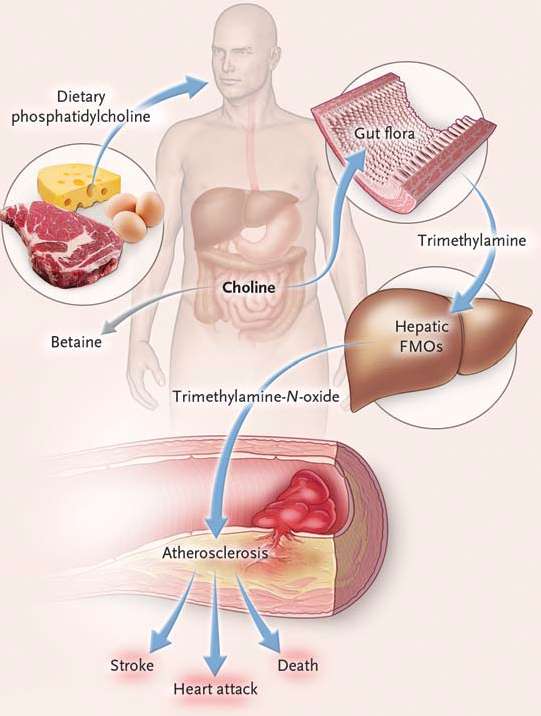
Source: Tang, WHW, et al.: N. Engl. J. Med. 2013;368:1575-1584.
TMAO production is also influenced by genetic factors. Taken together, these observations provide evidence of a complex interaction among humans, their resident gut flora, and environmental and behavioral factors (diet). Moreover, these newer observations raise the possibility of new interventions, e.g., by modifying diet to reduce consumption of L-carnitine and phosphatidylcholine, by modifying gut flora via antibiotics or probiotics, or by inhibiting the synthesis of TMAO pharmacologically. It is advisable to limit red meat consumption and to avoid lecithin (phosphatidlycholine) supplements (which are sold as tablets in drug stores and "health food stores."
Current Dietary Recommendations from the American Heart Association
Note that these recommendations do not include specific recommendations based on some of the newest scientific evidence cited above.
|
American Heart Association Recommendations |
|---|
|
As part of a healthy diet, an adult consuming 2,000 calories daily should aim for:
Other Dietary Measures:
|
Some Myths About Diet and Heart Disease
- Eating eggs increases one's risk of atherosclerosis and heart disease. False. Eggs are rich in cholesterol, but there is no evidence that eating eggs (even daily) increases plasma cholesterol or risk of heart disease. The cholesterol in an egg will be absorbed by the intestine and packaged into chylomicrons and distributed, but ultimately the exogenous cholesterol will temporarily result in increased cholesterol levels in liver cells; this will down-regulate (turn off) endogenous production of cholesterol in the liver. [Shin JY, Xun P, et al.: Egg consumption in relation to risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2013 Jul;98(1):146-59.
- Consuming garlic supplements reduces heart disease. False. Gardner et al. randomly assigned 192 adults with low-density lipoprotein cholesterol (LDL-C) concentrations of 130 to 190 mg/dL to one of the following treatment arms: raw garlic, powdered garlic supplement, aged garlic extract supplement, or placebo. Garlic product doses equivalent to an average-sized garlic clove were consumed 6 d/wk for 6 months. None of the garlic treatments had any statistically significant or clinically significant effects on LDL-C or other plasma lipid concentrations in these adults with moderate hypercholesterolemia. [Gardner CD, Lawson LD, et al.: Effect of raw garlic vs commercial garlic supplements on plasma lipid concentrations in adults with moderate hypercholesterolemia: a randomized clinical trial. Arch Intern Med. 2007 Feb 26;167(4):346-53.]
- A low-fat diet reduces the risk of heart disease. False. [Howard BV, Van Horn L, et al.:Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006 Feb 8;295(6):655-66] These investigators conducted a randomized controlled trial of 48,835 postmenopausal women aged 50-79 years. Subjects were randomly assigned to one of two treatment groups: 1) intensive behavior modification idesigned to reduce total fat intake to 20% of calories and increase intakes of vegetables/fruits to 5 servings/d and grains to at least 6 servings/d. or 2) a comparison group receiving diet-related education materials. After a mean of 8.1 years of follow up, the investigators concluded that reduced total fat intake and increased intakes of vegetables, fruits, and grains did not significantly reduce the risk of CHD, stroke, or CVD in postmenopausal women.