HIV and XDR-TB, a Fatal Combination
Immuno-compromised people are more likely to contract TB, and the combination of HIV and MDR- or XDR-TB can be fatal. With drugs prolonging the lives of HIV-positive individuals and with no current cure for HIV, the incidence of XDR-TB increases and poses a serious problem. While 75% of healthy people with MDR-TB recover, the death rate for HIV-infected people who have also contracted MDR-TB is 40-60% (Shufro, 2007).
|
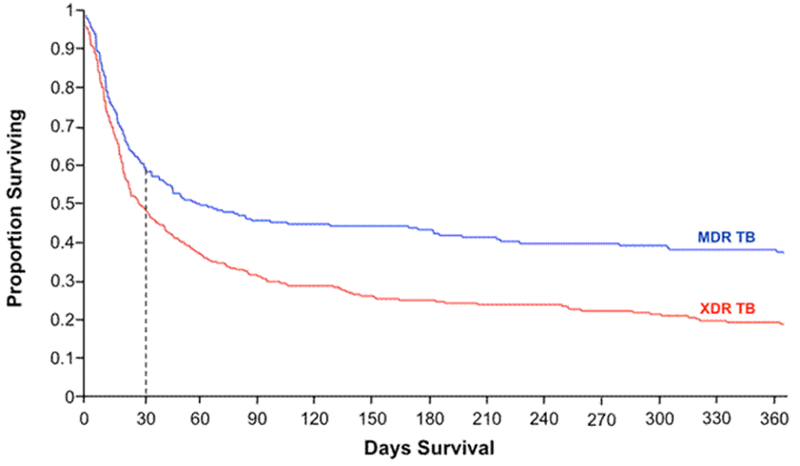
Figure 3: The Kaplan-Meier survival plot from a retrospective observational study of 272 MDR and 384 XDR-TB cases co-infected with HIV in South Africa shows the survival disparity between the two groups. The graph indicates that those with MDR-TB and HIV have a 40% chance of survival, whereas those with XDR-TB and HIV have a 20% chance, supporting the claim that those with XDR-TB have a higher relative risk of early mortality than those with MDR-TB (HIV Web Study, 2010). |
|
A study conducted by Yale University between 2003 and 2007 on HIV and drug-resistant TB in rural South Africa defined the growing global problem with XDR-TB. Of the 53 patients with XDR-TB, all of them were also confirmed or suspected HIV cases. 52 of those patients died with an average survival rate of less than a month after their sputum was taken for testing: "'what was repeated over and over again was the mortality rate: 98 percent...people are waking up. They are realizing that TB is a worldwide catastrophe,'" proclaimed Friedland, one of the lead scientists (Shufro, 2007).
Again, the problem of affordable and accessible drugs persists. Yale discovered that South African doctors only had two or three expensive second-line drugs to treat MDR-TB, however, they were less effective. When the drugs did not work, patients died (Shufro, 2007).
"'This is an issue of grave worldwide importance...MDR and XDR [TB] carry the danger of blunting or reversing the success of TB programs and the roll-out of anti-retroviral [sic] therapies for HIV where they are desperately needed in resource limited settings,'" said Friedland. He calls for urgency in intervening to treat and prevent drug-resistant TB, especially now that MDR- and XDR-TB are more prevalent than previous thought and that XDR-TB and HIV co-infections are associated with high mortality (ScienceDaily, 2006).
Can XDR-TB be contained? Can epidemiologists fully predict its course? Or will it become, as Friedland called a "'slow tsunami,'" like AIDS, "'a vague and yet very palpable feeling of dread that something very bad was happening'" (Shufro, 2007).
Are There Any Solutions?
In the CDC pod cast, Dr. Cegielski is asked to share his thoughts on a solution to the influx of XDR-TB cases: "'we need stronger labs in countries that are most infected [sic] by drug-resistant TB. And we need new drugs. But those are years in the future'"(CDC, 2008). TB continues to grow resistant to the second-line drugs faster than scientists can find new, effective third-line drugs to treat XDR-TB. Research must be focused on increasing the effectiveness of overseas labs in diagnosis and treatment of MDR- and XDR-TB, as well as focused on discovering stronger third-line drugs. 40 years is too long to wait for a new treatment to a quickly spreading and potentially fatal disease.
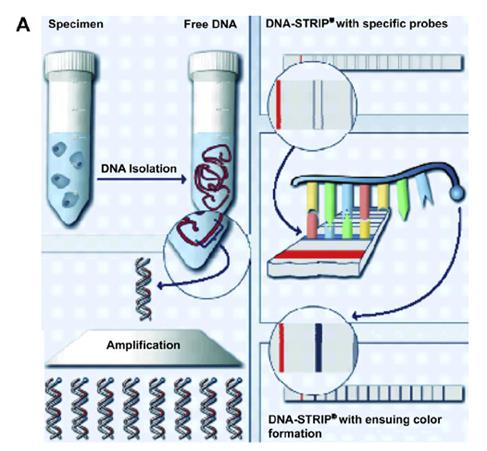
A 2013 study conducted in India, the country with the highest rates of TB and second highest rates of MDR-TB after China, according to WHO (National Academy of Sciences, 2012), tested the efficacy of a drug resistance testing device, GenoType® MTBDRsl assay in determining MDR- and XDR-TB cases. The scientists found that the GenoType ® MTBDRsl assay produced accurate second-line drug resistance diagnoses within 5 hours, as opposed to 1-2 months, which provided more information on the frequency of mutation trends responsible for XDR-TB resistance. Rapid diagnosis and identification of XDR-TB will aid in faster implementation of proper control techniques, such as isolation and country-specific TB action programs, to prevent the further spread of the disease.
|
Figure 4: For XDR-TB screening, the DNA strip indicates whether the specimen contains TB resistant to fluoroquinolones, aminoglycosides/cyclic peptides, and/or ethambutol, evident via a dark line on the specific strip marker. The process is as follows: 1--TB DNA is extracted from the sputum sample 2--DNA is amplified via PCR 3--DNA is applied to strip with specific probes 4--DNA is detected on strip using reverse hybridization and enzymatic color reaction, resulting in a dark line when detection is positive. (Schaaf, 2009). |
|
Continued efforts on educating the world about the importance of treatment compliance and the basics on TB may continue to help reduce the incidence of MDR-TB with hopes that XDR-TB, too, will be kept at bay.