
Equity
Health Disparities, Social Determinants & Vulnerable Populations

The health of a community is determined by many factors besides the quality of medical care. Health disparities are differences in health or health-related outcomes associated with a socio-economic or environmental disadvantage. This module will examine economics, education, health care access and health outcomes for a racial and ethnic minorities, and it will also explore disparities related to gender and age (both young and old).
We will also briefly discuss mental health with a focus on finance, access and stigma. Stigma for persons with mental illness and substance use disorders is an enormous problem which prevents people from seeking care, changes the way they perceive themselves, and affects how they are treated by others.
 |
|---|
| A health disparity is a particular type of health difference that is closely linked with social, economic, and/or environmental disadvantage. Racial and ethnic minorities still lag behind in many health outcome measures. They are less likely to get the preventive care they need to stay healthy, more likely to suffer from serious illnesses, such as diabetes or heart disease, and when they do get sick, are less likely to have access to quality health care. Disparities are documented in many conditions, including: cardiovascular disease, asthma, diabetes, flu, infant mortality, cancer, HIV/AIDS, chronic lower respiratory diseases, viral hepatitis, chronic liver disease and cirrhosis, kidney disease, injury deaths, violence, behavioral health, and oral health. (Fact Sheet: The HHS Action Plan to Reduce Racial and Ethnic Health Disparities.)
From the HHS Action Plan to Reduce Racial and Ethnic Health Disparities, 2011 |
As an introduction to the week, watch this short video on health equity from the Association of American Medical Colleges.
|
Living in Disadvantaged Neighborhoods is Bad for Your Health |
Each year the Agency for Healthcare Research and Quality (AHRQ) reports on the opportunities for improving health care quality and reducing health care disparities in the United States. Based on the latest data, reports show health care quality continues to improve—but health care disparities persist for many of America's minorities and the poor. As AHRQ Director Dr. Carolyn Clancy explains, "These reports show that health care quality in the US is continuing to improve, but at a very slow rate and that, generally, inequalities in health care are not improving. We need to ramp up our overall efforts to improve health care quality and focus specific attention on areas that need the greatest improvement so that all Americans have access to high-quality, appropriate, and safe health care."
|
|
The National Health Disparities Report
The National Health Disparities Report for 2013 (May 2014) presents the nation's priorities and action plans to reduce health disparities among racial and ethnic minorities. The plan reflects provisions of the ACA and HP 2020 goals.
|
AHRQ's priority populations, specified by Congress in the Healthcare Research and Quality Act of 1999 (Public Law 106-129), are:
Other populations, such as LGBT (lesbian, gay, bisexual and transgender persons) and those with multiple chronic medical conditions (MCC), are also included.
|
|
|
The National Center on Minority Health and Health Disparities (NCMHD) promotes minority health and leads, coordinates, supports, and assesses the NIH effort to reduce and ultimately eliminate health disparities. The NCMHD works independently and in partnership with the NIH Institutes and Centers and with other Federal agencies and grassroots organizations in minority and in other medically underserved communities to:
Important Events in NCMHD History
1990 – The Office of Research on Minority Health (ORMH) was established, with the encouragement of Congress, by the Director, National Institutes of Health (NIH).
1992 – The Minority Health Initiative (MHI), the centerpiece of the ORMH agenda, was launched. This biomedical and behavioral research and research training program co-funds: through its partnerships:
The Indian Health Service is an agency within the U.S. Department of Health and Human Services with the mission to be the principal advocate for and provider of health services to American Indians and Alaska Natives.
The Migrant Health Center Program was established by the Migrant Health Act (1962) to provide medical and support services to migrant farm workers and their families.
Women have a greater life expectancy than men, but face greater morbidity and poorer health outcomes when compared to men, and may develop more acute and chronic illnesses and resulting disabilities. Also, certain mental disorders, especially depression, are more common among women. Women are the principal users of health care services, and often coordinate health care for their families. But women under the age of 65 are less likely to be insured than men.
Though insurance discrimination will be banned as a result of the Affordable Care Act and women will no longer have to pay higher premiums because of their gender, this has not always been the case. Why did this happen in the first place? Insurers say they have a sound reason for charging different premiums: Women ages 19 to 55 tend to cost more than men because they typically use more health care, especially in the childbearing years. Additionally, they are more likely to visit doctors, to get regular checkups, and to take prescription drugs. Low-income women are especially disadvantaged. Low-income pregnant women may be eligible for Medicaid. As we have said before, insurance coverage is the first step towards access. In some areas there are not OB/GYN providers accepting Medicaid and women may have to travel hours for pre-natal care. The most vulnerable group is women with low-income in the more disadvantaged racial and ethnic groups presented earlier in this session.
Kaiser Family Foundation Presentation on women's health and how both Medicaid and the ACA impact gender disparities.
May 14, 2013 The Role of Medicaid and Medicare In Women's Health Care, JAMA, May 15, 2013
Children, on the other hand, may have a developmental vulnerability. Your readings and lecture illustrate how illness, injury, family, and other social circumstances can have an impact on a child's life-course trajectory. Additionally, there is a dependency in children as a special circumstance, in that adults generally have to recognize and respond to their health care needs. Older children may face challenges as well, related to drug and alcohol abuse, family and neighborhood violence, emotional disorders, learning problems, and other problems such as teenage pregnancies, tobacco use, etc. They point out that these dysfunctions are usually linked to family and socioeconomic conditions.
Children are the age group most impacted by poverty, especially young children. Black and Hispanic children are disproportionately affected. Children are not the least likely to be insured, however, because of Medicaid and SCHIP (State Children's Health Insurance Program). Read some sobering statistics below from the Children's Defense Fund.
 Moments in America for Children from the Children's Defense Fund's The State of America's Children 2014 Handbook
Moments in America for Children from the Children's Defense Fund's The State of America's Children 2014 Handbook
In 1997 the State Children's Health Insurance Program (SCHIP or CHIP) was enacted to provide coverage for uninsured low-income children who did not qualify for Medicaid. SCHIP was reauthorized in February of 2009. States had the option of creating a separate SCHIP program, using the funds to expand existing state Medicaid programs, or creating a hybrid program. SCHIP was expanded in 2009 with funds from taxes on tobacco products.
The video below shows Children's Defense Fund President Marian Wright Edelman testifying before the House Committee on Energy and Commerce on June 23, 2009, about health care reform and children at risk in our country. She makes specific reference to the disparities across states for Medicaid coverage by FPL.
|
CDF President Marian Wright Edelman Health Care Reform Testimony |
Elders have quantitatively and qualitatively different care needs than adults. We have previously seen how the population of elders and the very elderly (85 years and up) is growing. Fragmented care and lack of geriatric-specific services are among the many specific challenges of this vulnerable population.
According to the Institute of Medicine's report, Retooling for an Aging America: Building the Health Care Workforce, the number of older adults in the United States "will almost double between 2005 and 2030, the nation is not prepared to meet their social and health care needs, [and] that the baby boomer generation starts to turn 65 in 2011, which will create multiple challenges for the health care system."
One major issue is that many adults who do not have insurance go long periods of time without medical care until they can qualify for Medicare. In so doing, they are jeopardizing their current and future health, and potentially increasing the costs of care to the public. This, according to the report, is a potentially serious concern for older adults who tend to have more chronic conditions and medical needs than younger adults. Coverage options will expand with the ACA from the Exchanges. Coverage for the very poor depends on the state's decision to expand Medicaid.
Turning 65 may mean a Medicare card is coming, but it does not end worry about health care costs. Remember: Medicare is not free. There are premiums and cost sharing arrangements depending on the part. More than a quarter of Medicare recipients rate their own health as fair to poor. About half are living on a limited income, and half have limited savings (not mutually exclusive groups).
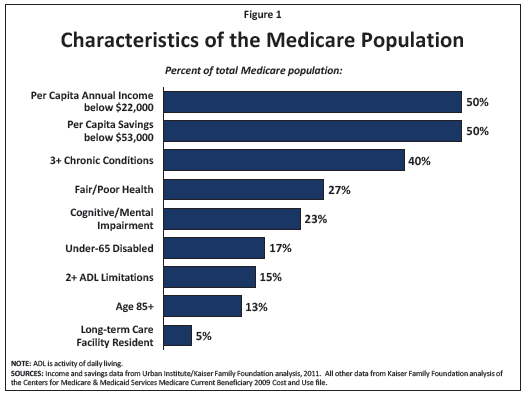
Source::www.kff.org/medicare/upload/1066-15.pdf
Here is a creative and efficient idea: why not have an Emergency Room built especially for older adults? Joseph Shapiro notes that only infants go to the emergency department at a higher rate than people 75 and older, and for years, many hospitals have set up separate emergency rooms just for kids. So why not set up an ER specifically for patients 65 and older—one that is staffed by health professionals who are trained in gerontology and geriatric medicine? An Emergency Room Built Specially For Seniors
The Program of All Inclusive Care to the Elderly (PACE) keeps participants in the community, living at home, and attending a mandatory day health program. PACE provides comprehensive medical and social services to certain frail, community-dwelling elderly individuals, most of whom are dually eligible for Medicare and Medicaid benefits . An interdisciplinary team of health professionals provides PACE participants with coordinated care. For most participants, the comprehensive service package enables them to remain in the community rather than receive care in a nursing home.
A program local to Boston University is the Commonwealth Care Alliance (CCA). As with PACE this is a program for dual eligible (those with Medicaid and Medicare). Both programs are PCMHs. In PACE the medical home is at the adult day care. In CCA the medical home is at the person's actual residence.
CCA is a Senior Care Options Program (SCO), and several of these were discussed in your reading . Much of the medical care for CCA patients is provided at home by a team of nurse practitioners. Home visits are scheduled on a routine basis, and added as needed for acute concerns and post-hospitalization follow up. The other staff person central to this model of care is the geriatric care worker As you read about this week, social support is key to the success of this type of program.
Watch the video below. The woman featured attends an adult care center, but as an add-on to the home-based services. Dr. Robert Masters is interviewed in the video, and speaks specifically to the need for social services.
|
|
Please watch the following slide show on racial and ethnic disparities. As you will see, several of the groups are more likely to be in low-income groups when compared to the reference group (usually non-Hispanic Whites). Watch and listen to get a general impression of the changing racial and ethnic makeup of the US, how these groups differ in the aspects of socioeconomic status, patterns of health disparities, and how causes of death differ. The US is becoming a minority-majority nation, starting with newborns. By the end of this should you should be able to explain this concept.
Before you start there are several methodological notes related to the data. Collection of race and ethnicity data is complex and ever changing. A serious challenge is how to capture the increasing number of individuals with multi-racial or multi-ethnic backgrounds.
In this presentation African-Americans will generally refer to Black Americans, African Americans and those of non-Hispanic Caribbean ancestry.
The Latino population is lumped into one group as Hispanic, but this is a gross oversimplification. A shared language does not mean a shared culture. Familiarity with the country of origin is key to understanding some of the cultural differences, which are also seen in socioeconomic status and health disparities. There are geographic patterns of immigration. If you are working in an area with a Latino population it is important to know this and become as familiar as possible with the specific groups.
The national data sets used do not generally collect and report out results specific to Native Hawaiians or Pacific Islanders. They are generally grouped in with Asians.
The term Indian is also ambiguous. American Indian refers to the group of people indigenous to the Americas. Outside of data collection this group is referred to as Native American. Persons from the continent of India were previously East Indians, now often South Asian, but in the data Asian Indians in the Asian American category.
|
|
Disparities are about more than the people, they are also about the place. Remember we looked at the influence of geography on multiple health services measures: hospital beds, Medicaid eligibility, uninsurance rates and more. While overall life expectancy in the United States has improved, racial and socioeconomic disparities in mortality and health status have widened. Many Americans fail to receive treatments of proven benefit -- a burden that falls most heavily on racial and ethnic minorities, and low-income populations. As numerous studies have documented, income and race are important determinants of both the health care patients receive and of patients' health care outcomes.
These disparities are particularly striking when examined across US states and regions; it's not only who you are that matters, but also where you live. Indeed, many studies that report racial disparities based on national samples do not account for the tremendous variation across regions and procedures. The rate of leg amputation -- a devastating complication of diabetes and peripheral vascular disease -- is four times greater in blacks than in whites; but rates of amputation vary nearly tenfold across regions. For evidence-based services, such as screening mammography and appropriate testing for diabetes, disparities across regions are substantially greater than the differences by race; there are some regions where blacks receive equal or better care than whites but where care for all patients is less than ideal.
Geographic variations in health care are responsible for a substantial component of the observed racial disparity in care, since blacks live disproportionately in parts of the country that have low-quality hospitals and providers. Hospitals and regions of the country also vary enormously in the extent to which disparities are present. Health care disparities are the result of both unequal treatment within a hospital or by a given provider, and unequal treatment because of where people live. These findings highlight the importance of understanding health and health care within a local context -- and of efforts to explore and address the underlying causes of disparities within and across regions.
From www.dartmouthatlas.org/keyissues/issue.aspx?con=2942
Often we speak about income in terms of income by household or per capita (per person). There is increasing data supporting the idea of income inequality as an important measure in understanding health disparities. What is someone's income relative to other members of the population? How is income distributed across a population? Are there widening gaps between the rich and the poor? What about the wealthy and the middle class?
Median income by household for 2009-2011 was $50,443. Inspect the map below to see which states are above and below this household income.

Social mobility is the movement of individuals between socioeconomic groups. For our purposes think of vertical mobility. How likely is a person to be able to move from one socioeconomic group to another? Movement can be downward (down the social hierarchy) or upward (advancement). Mobility is seen as a proxy for opportunity within the social system.
Relative income is an important concept. Please watch this talk by Richard Wilkinson entitled "How Economic Inequality Harms Societies."
|
How Economic Inequality Harms Societies |
Not all Americans have equal access to health care—or similar health care outcomes. The site points out that low-income Americans, racial and ethnic minorities, and other underserved populations often have higher rates of disease, fewer treatment options, and reduced access to care. They are also less likely to have health insurance than the population as a whole. So it makes sense that by improving access to quality health care for all Americans, the Affordable Care Act can help reduce these health disparities. The new law will bring down health care costs, invest in prevention and wellness, and give individuals and families more control over their own care.
The Affordable Care Act will help reduce disparities by making improvements in:

One of the major strategies to improve health in the United States is the science-based, 10-year national objectives initiative called Healthy People (HP). This initiative, which integrates medical care with preventive services, has set and monitored national health objectives since 1979. Healthy People attempts to meet a broad range of health needs, to encourage collaboration across sectors, to guide individuals toward making informed health decisions, and to measure the impact of prevention activity. Every 10 years, HHS includes scientific insights and lessons learned from the past decade, along with current data and information about trends and innovations.
The Healthy People 2020 (HP 2020) initiative, launched in 2010, outlined the leading health indicators to measure the health of the nation over a span of 10 years. The video below, which features Dr. Howard Koh, the Assistant Secretary for Health, US Department of Health and Human Services. Dr. Koh received his MPH from the Boston University School of Public Health.
|
Source: Preparing for the Next Decade: A 2020 Vision for Healthy People |
Key goals for 2020:
|
|
| Source: www.healthypeople.gov/2020/LHI/2020indicators.aspx | |
Each indicator has a set of measurable objectives. Each objective has a baseline and a target, as well as the data source. Here is an example of the Healthy People 2020 goals regarding Access to Health Care:.For example, click "AHS-1.1" in the iFrame below to expand it.
To learn more about Healthy People 2020, click on these helpful links:
 |
|---|
The World Health Organization (WHO) notes that social determinants of health are "the conditions in which people are born, grow, live, work and age" that can contribute to or detract from the health of individuals and communities. Marked differences in social determinants, such as poverty, low socioeconomic status (SES), and lack of access to care, exit along racial and ethnic lines. These differences can contribute to poor health outcomes (from the HHS Action Plan to Reduce Racial and Ethnic Health Disparities, p. 2).
The CDC Health Impact Pyramid, created by Dr. Thomas Frieden, Director of the Centers for Disease Control and former Commissioner of the NYC Health Dept., is a five-tier pyramid that best describes the impact of different types of public health interventions and provides a framework to improve health.
|
CDC Health Impact Pyramid
|
At the base of this pyramid, indicating interventions with the greatest potential impact, are efforts to address socioeconomic determinants of health such as poverty, education, housing, and inequality. In ascending order are interventions that change the context to make individuals' default decisions healthy, such as fluoridation of our water, elimination of transfats in our diets and our restaurants, policies and laws that facilitate smoke-free environments, and taxing harmful substances, such as tobacco, alcohol, and sugar-sweetened beverages.
Clinical interventions that require limited contact but confer long-term protection include immunizations, brief or sporadic interventions, as well as treatments such as smoking cessation programs.
Ongoing direct clinical care such as treatment for hypertension, high cholesterol, diabetes, and heart disease may demonstrate a smaller impact over the long haul, as well as health education and counseling, in which people are taught to eat healthy and increase their levels of physical activity.
Interventions focusing on lower levels of the pyramid tend to be more effective because they reach broader segments of society and require less individual effort. Implementing interventions at each of the levels can achieve the maximum possible sustained public health benefit.
The essays below from the Robert Wood Johnson Foundation offer further evidence of the impact of social determinants on health outcomes.
|
Health Starts Where We Live, Learn, Work and Play |
|
|
|
 Health Starts Where We Learn |
 Health Starts Where We Work |
 Health Starts Where We Play |
"Health Starts Where We Live, Learn, Work and Play" from www.rwjf.org/pr/product.jsp?id=70928
The project: www.rwjf.org/en/research-publications/find-rwjf-research/2010/01/a-new-way-to-talk-about-the-social-determinants-of-health.html
This video by the Boston Public Health Commission's Center for Equity and Social Justice highlightis the work of three grantees from their community-based strategies for eliminating racial and ethnic health inequities program.
|
The Center for Health Equity and Social Justice: Shifting the Public Health Paradigm
|
Mental health is a state of well-being in which an individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community. In this positive sense, mental health is the foundation for individual well-being and the effective functioning of a community.
About half of adults will meet criteria for a mental health disorder over their lifetime. Mental health diagnoses include mental illness and substance abuse. Traditionally, mental illness has been conceptualized as disorders of mood or thought. Examples are depression, bipolar disorder, anxiety disorders, and psychotic disorders. It may seem tidy to be able to categorize conditions into seemingly dichotomous groups for physical or mental disorders. In reality there is an increasingly recognized biologic basis for mental illness, and for all individuals body and mind exist on a continuum. We know mental illness is not the consequence of poor character, but significant stigma remains. Even more stigmatized are the substance use disorders (SUDs). Persons with dependence on alcohol or illicit drugs are often unable to stop using without support. Sources of this support include peer groups, medical care providers, and counselors with training in addiction medicine. From a clinical perspective the SUDs are mental health disorders, but systems of treatment are generally separate.
The term "behavioral health" is sometimes used for mental health and substance use services. One could argue that behavioral health is a less stigmatizing term. One could also argue that it has more of a negative connotation and attributes blame to the person with the illness - as though a cure is merely a matter of will-power. The bottom line is that words matter. For more information read this excellent fact sheet from NAMI titled, Facts about Mental Illness and Stigma in Diverse Communities.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is published by the American Psychiatric Association (APA).The APA is a large and powerful interest group. The DSM provides the diagnostic criteria used to classify mental illness, SUD, and intellectual disorders. Revisions have been underway and the 5th edition is expected to be released in May 2013. Revisions are always controversial as these criteria often define eligibility for services. Adults with mental health disorders are more likely to have chronic, physical illnesses. This serves to further fragment care as systems of care for medical and mental disorders have both separate and different systems for organization, provision of services, and finance.
Mental health is an integral and essential component of health. The World Health Organization (WHO) constitution states: "Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity." An important consequence of this definition is that mental health is described as more than the absence of mental disorders or disabilities."
Multiple social, psychological, and biological factors determine the level of mental health of a person at any point of time. For example, persistent socio-economic pressures are recognized risks to mental health for individuals and communities. The clearest evidence is associated with indicators of poverty, including low levels of education.
oor mental health is also associated with rapid social change, stressful work conditions, gender discrimination, social exclusion, unhealthy lifestyle, risks of violence and physical ill-health and human rights violations.
There are also specific psychological and personality factors that make people vulnerable to mental disorders. Lastly, there are some biological causes of mental disorders including genetic factors and imbalances in chemicals in the brain.
From: The World Health Organization. Mental Health: Strengthening our Response. Fact sheet N°220, September 2010
Substance Use Disorders (SUD) are also classified by the DSM. In the new version of the DSM (DSM-5) it is expected that the categories of abuse and dependence will be replaced by the umbrella of SUD. Alcohol, cocaine, opioids anThis is important because the formal diagnosis with DSM criteria is necessary to qualify an individual to receive services. Payers require documentation to reimburse for services.
Substance Use in the United States (2011, SAMHSA Survey)
It is estimated that 8.7 percent of the population aged 12 or older used illicit drugs within the past month. Illicit drugs include marijuana/hashish, cocaine (including crack), heroin, hallucinogens, inhalants, or prescription-type psychotherapeutics (pain relievers, tranquilizers, stimulants, and sedatives) used non-medically.
Alcohol use:
Alcohol use followed a different pattern. Binge drinking and heave use were highest (> 20%) in whites and Native Americans/Alaskan Natives.
What about treatment for alcohol and drug dependence?
|
Figure 7.11 Reasons for Not Receiving Substance Use Treatment among Persons Aged CREDIT: www.samhsa.gov/data/NSDUH/2k11Results/NSDUHresults2011.htm#High |
Dual Diagnoses
Estimates vary, but there is significant known overlap between mental illness and substance use populations. This is k, i.e., dual diagnoses. These individuals present unique treatment needs as facilities designed for either population may not have the capacity to provide appropriate treatment for both.
Now think about the co-occurrence with physical health problems. The systems of care for mental illness, substance abuse, and medical care often operate in silos. The challenges of providing quality (or even minimally acceptable) care to this vulnerable population can be overwhelming.
Potential Impact of the ACA