Trends and Need Characteristics
Women
Women have a greater life expectancy than men, but face greater morbidity and poorer health outcomes when compared to men, and may develop more acute and chronic illnesses and resulting disabilities. Also, certain mental disorders, especially depression, are more common among women. Women are the principal users of health care services, and often coordinate health care for their families. But women under the age of 65 are less likely to be insured than men.
Though insurance discrimination will be banned as a result of the Affordable Care Act and women will no longer have to pay higher premiums because of their gender, this has not always been the case. Why did this happen in the first place? Insurers say they have a sound reason for charging different premiums: Women ages 19 to 55 tend to cost more than men because they typically use more health care, especially in the childbearing years. Additionally, they are more likely to visit doctors, to get regular checkups, and to take prescription drugs. Low-income women are especially disadvantaged. Low-income pregnant women may be eligible for Medicaid. As we have said before, insurance coverage is the first step towards access. In some areas there are not OB/GYN providers accepting Medicaid and women may have to travel hours for pre-natal care. The most vulnerable group is women with low-income in the more disadvantaged racial and ethnic groups presented earlier in this session.
Kaiser Family Foundation Presentation on women's health and how both Medicaid and the ACA impact gender disparities.
May 14, 2013 The Role of Medicaid and Medicare In Women's Health Care, JAMA, May 15, 2013
 |
Change slides by using the arrows or drop-down menu. I |
|
This content requires JavaScript enabled.
|
|
Children
Children, on the other hand, may have a developmental vulnerability. Your readings and lecture illustrate how illness, injury, family, and other social circumstances can have an impact on a child's life-course trajectory. Additionally, there is a dependency in children as a special circumstance, in that adults generally have to recognize and respond to their health care needs. Older children may face challenges as well, related to drug and alcohol abuse, family and neighborhood violence, emotional disorders, learning problems, and other problems such as teenage pregnancies, tobacco use, etc. They point out that these dysfunctions are usually linked to family and socioeconomic conditions.
Children are the age group most impacted by poverty, especially young children. Black and Hispanic children are disproportionately affected. Children are not the least likely to be insured, however, because of Medicaid and SCHIP (State Children's Health Insurance Program). Read some sobering statistics below from the Children's Defense Fund.
 Moments in America for Children from the Children's Defense Fund's The State of America's Children 2014 Handbook
Moments in America for Children from the Children's Defense Fund's The State of America's Children 2014 Handbook
- 2 mothers die in childbirth
- 4 children are killed by abuse or neglect
- 24 children or teens die from accidents
- 66 babies die before their first birthday
- 187 children are arrested for violent crimes
- 865 babies are born at low birth weight
- 1,392 babies are born into extreme poverty
The State Children's Health Insurance Program
In 1997 the State Children's Health Insurance Program (SCHIP or CHIP) was enacted to provide coverage for uninsured low-income children who did not qualify for Medicaid. SCHIP was reauthorized in February of 2009. States had the option of creating a separate SCHIP program, using the funds to expand existing state Medicaid programs, or creating a hybrid program. SCHIP was expanded in 2009 with funds from taxes on tobacco products.
The video below shows Children's Defense Fund President Marian Wright Edelman testifying before the House Committee on Energy and Commerce on June 23, 2009, about health care reform and children at risk in our country. She makes specific reference to the disparities across states for Medicaid coverage by FPL.
|
CDF President Marian Wright Edelman Health Care Reform Testimony |
Elders Aging in the Community, Community-Based LTC, and Nursing Homes
Elders have quantitatively and qualitatively different care needs than adults. We have previously seen how the population of elders and the very elderly (85 years and up) is growing. Fragmented care and lack of geriatric-specific services are among the many specific challenges of this vulnerable population.
According to the Institute of Medicine's report, Retooling for an Aging America: Building the Health Care Workforce, the number of older adults in the United States "will almost double between 2005 and 2030, the nation is not prepared to meet their social and health care needs, [and] that the baby boomer generation starts to turn 65 in 2011, which will create multiple challenges for the health care system."
One major issue is that many adults who do not have insurance go long periods of time without medical care until they can qualify for Medicare. In so doing, they are jeopardizing their current and future health, and potentially increasing the costs of care to the public. This, according to the report, is a potentially serious concern for older adults who tend to have more chronic conditions and medical needs than younger adults. Coverage options will expand with the ACA from the Exchanges. Coverage for the very poor depends on the state's decision to expand Medicaid.
Turning 65 may mean a Medicare card is coming, but it does not end worry about health care costs. Remember: Medicare is not free. There are premiums and cost sharing arrangements depending on the part. More than a quarter of Medicare recipients rate their own health as fair to poor. About half are living on a limited income, and half have limited savings (not mutually exclusive groups).
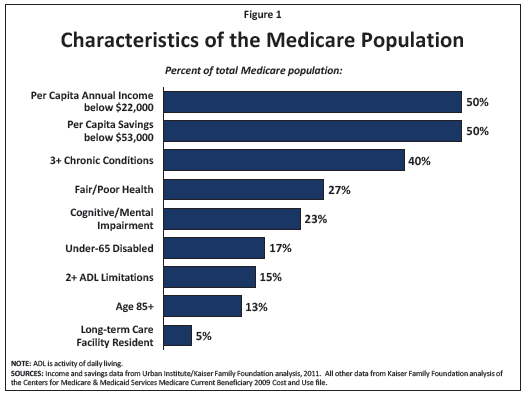
Source::www.kff.org/medicare/upload/1066-15.pdf
Here is a creative and efficient idea: why not have an Emergency Room built especially for older adults? Joseph Shapiro notes that only infants go to the emergency department at a higher rate than people 75 and older, and for years, many hospitals have set up separate emergency rooms just for kids. So why not set up an ER specifically for patients 65 and older—one that is staffed by health professionals who are trained in gerontology and geriatric medicine? An Emergency Room Built Specially For Seniors
Long Term Care
- Medicare does not pay for long-term care. What does this mean?
- Medicare will pay for up to 100 days in a nursing or rehabilitation facility for rehabilitation
- Medicare will not pay for residential placement or custodial nursing care
- State laws vary, but in many cases an elder must spend down through his or her savings and will then quality for Medicaid (become a dual eligible)
- About 30% of Medicaid expenditures go to long term care, about 1/3 of this is for skilled nursing facilities
The Program of All Inclusive Care to the Elderly (PACE) keeps participants in the community, living at home, and attending a mandatory day health program. PACE provides comprehensive medical and social services to certain frail, community-dwelling elderly individuals, most of whom are dually eligible for Medicare and Medicaid benefits . An interdisciplinary team of health professionals provides PACE participants with coordinated care. For most participants, the comprehensive service package enables them to remain in the community rather than receive care in a nursing home.
A program local to Boston University is the Commonwealth Care Alliance (CCA). As with PACE this is a program for dual eligible (those with Medicaid and Medicare). Both programs are PCMHs. In PACE the medical home is at the adult day care. In CCA the medical home is at the person's actual residence.
CCA is a Senior Care Options Program (SCO), and several of these were discussed in your reading . Much of the medical care for CCA patients is provided at home by a team of nurse practitioners. Home visits are scheduled on a routine basis, and added as needed for acute concerns and post-hospitalization follow up. The other staff person central to this model of care is the geriatric care worker As you read about this week, social support is key to the success of this type of program.
Watch the video below. The woman featured attends an adult care center, but as an add-on to the home-based services. Dr. Robert Masters is interviewed in the video, and speaks specifically to the need for social services.
|
|
Minorities and Low Income Families
Please watch the following slide show on racial and ethnic disparities. As you will see, several of the groups are more likely to be in low-income groups when compared to the reference group (usually non-Hispanic Whites). Watch and listen to get a general impression of the changing racial and ethnic makeup of the US, how these groups differ in the aspects of socioeconomic status, patterns of health disparities, and how causes of death differ. The US is becoming a minority-majority nation, starting with newborns. By the end of this should you should be able to explain this concept.
Before you start there are several methodological notes related to the data. Collection of race and ethnicity data is complex and ever changing. A serious challenge is how to capture the increasing number of individuals with multi-racial or multi-ethnic backgrounds.
-
In this presentation African-Americans will generally refer to Black Americans, African Americans and those of non-Hispanic Caribbean ancestry.
-
The Latino population is lumped into one group as Hispanic, but this is a gross oversimplification. A shared language does not mean a shared culture. Familiarity with the country of origin is key to understanding some of the cultural differences, which are also seen in socioeconomic status and health disparities. There are geographic patterns of immigration. If you are working in an area with a Latino population it is important to know this and become as familiar as possible with the specific groups.
-
The national data sets used do not generally collect and report out results specific to Native Hawaiians or Pacific Islanders. They are generally grouped in with Asians.
-
The term Indian is also ambiguous. American Indian refers to the group of people indigenous to the Americas. Outside of data collection this group is referred to as Native American. Persons from the continent of India were previously East Indians, now often South Asian, but in the data Asian Indians in the Asian American category.
|
|

